To estimate the prevalence of depression and abuse and identify the associated factors in medical interns in Peruvian hospitals.
MethodsWe conducted a multicentre, cross-sectional and analytical study during the months of March to May 2016. We included medical interns from 18 Peruvian hospitals, in Lima and provinces. We used a survey that included sociodemographic data and a scale to measure the perception of abuse (psychological, physical and sexual). In addition, we used the Spanish version of the PHQ-9 to evaluate depression. We used Poisson regression with robust variances to calculate prevalence ratios (PRs).
ResultsA total of 402 medical interns participated in the study, the median age was 25 [IQR: 21–33], and 52.7% were male. Moreover, 25.4% of them suffered from depression. In the adjusted model, the variables associated with depression were age (PRa=1.15), the number of hours they sleep per day (PRa=1.23), being a woman (PRa=3.33), performing the internship in a province (PRa=0.25), studying at a public university (PRa=0.64), living with parents (PRa=0.65) or alone (PRa=0.33), and having perceived some type of abuse (PRa=1.07).
ConclusionsA quarter of surveyed medical interns had depression. Early screening is necessary to identify perceived abuse and other triggering depression factors that may adversely affect work performance and overall mental health during medical internships.
Estimar la prevalencia de depresión y maltrato e identificar sus factores asociados en los internos de Medicina de los hospitales peruanos.
MétodosEstudio multicéntrico, transversal y analítico, llevado a cabo durante los meses de marzo a mayo de 2016. Conformaron la población los internos de Medicina en 18 sedes hospitalarias de Lima y provincias. Se aplicó una encuesta que incluía características sociodemográficas y una escala para medir la percepción de maltrato (psicológico, físico y sexual). Asimismo, para evaluar la depresión, se usó el cuestionario PHQ-9 en su versión en español. Se usó regresión de Poisson con varianzas robustas para calcular las razones de prevalencia (RP).
ResultadosParticiparon 402 internos de Medicina; la mediana de edad fue 25 [intervalo intercuartílico, 21-33] años y el 52,7% eran varones. Además, el 25,4% padecía depresión. En el modelo ajustado, las variables asociadas con padecer depresión son edad (RPa=1,15), cuántas horas duermen durante el día (RPa=1,23), ser mujer (RPa=3,33), realizar el internado en provincia (RPa=0,25), estudiar en una universidad pública (RPa=0,64), vivir con sus padres (RPa=0,65) o solo (RPa=0,33) y percibir algún tipo de maltrato (RPa=1,07).
ConclusionesLa cuarta parte de los internos encuestados tenían depresión. Es necesario realizar un cribado temprano para identificar posibles maltratos percibidos y otros factores desencadenantes de depresión, y así evitar repercusiones negativas en el desempeño laboral y la salud mental general durante el internado médico.
Depression is considered a public health problem that affects occupational, academic and family related activities. It is one of the major causes of disability due to neuro-psychiatric conditions worldwide.1
Medical students are constantly exposed to high academic and emotional loads, as well as high levels of stress and depression.2,3 These conditions are more intense during the internship.4 Medical internship is the last year of the medical career and represents a transition from the university life to the hospital environment.5 This period includes multiple stress factors such as work overloads, dealing with problematic patients, dealing with the patient's pain and death, workplace violence or mistreatment, non-fixed duty-hours and others.5–7
Globally, a prevalence of depression and depressive symptoms in medical students has been reported at 27.2%.8 In Asia, a study in Saudi Arabia found that 48% of medical students had depressive symptoms.9 In Latin America, a study made in Brazil10 reported that medical interns had higher scores on the Beck Depression Inventory (BDI) compared to the first-year medical students. In Peru,11 it has been reported that 35% of the interns in a hospital in Lima suffered from depression and 34.2% had burnout syndrome.
During the academic training, medical students are vulnerable to multiple factors such as mistreatment, depression, burnout, anxiety, stress and poor sleep quality.12–15 In addition, during the months prior to the internship, students often experience the fear of “knowing nothing”.16,17 These conditions increase when they start the internship. Also, some stressors add up: continuous night shifts, reduced time to recreational activities10,18 and the increasing pressure from the Examen Nacional de Estudiantes de Medicina (ENAM), which approval is mandatory for the Servicio Rural Urbano Marginal en Salud (SERUMS) in Peru.
On the other hand, attending physicians and residents usually use wrongs strategies to strengthen learning. For example, negative comments, yells, threats or unjustified criticisms, which together constitute the most frequent psychological mistreatment to medical students.6 This is associated with high levels of anxiety, stress and depression, being even more frequent during medical internship.19
The above mentioned represents a significant mental health problem for the medical intern, and may affect their learning and health-care performance.20,21 However, despite the importance of the topic, there is little national evidence to address this problem and identify the main contributing factors. For this reason, the aim of the study was to estimate the prevalence of depression and mistreatment and identify the factors associated in medical interns of Peruvian hospitals.
MethodsStudy designWe conducted a multicenter, cross-sectional and analytical study during the months of March to May 2016.
ParticipantsThe population was constituted by medical interns who were rotating in the departments of Surgery, Internal Medicine, Gynecology or Pediatrics in Peruvian hospitals. We included 18 hospitals located in 11 Peruvian regions. Two hospitals were in Lima and 16 were in provinces (Ancash, Arequipa, Ayacucho, Ica, Lambayeque, Loreto, Puno, San Martin, Tacna and Ucayali). Figure 1 shows the study geographic distribution.
Location of the Peruvian hospitals included in the study. 1: Hospital Apoyo Iquitos “César Garayar García”; 2: Hospital Regional de Loreto “Felipe Santiago Arriola Iglesias”; 3: Hospital III EsSalud Iquitos; 4: Hospital Regional Docente “Las Mercedes”; 5: Hospital II-2 Tarapoto; 6: Hospital La Caleta; 7: Hospital Regional Eleazar Guzmán Barrón; 8: Hospital Regional de Pucallpa; 9: Hospital Nacional Guillermo Almenara Irigoyen; 10: Hospital Nacional Hipólito Unanue; 11: Hospital Regional de Ayacucho “Miguel Ángel Mariscal Llerena”; 12: Hospital Regional de Ica; 13: Hospital Santa Maria del Socorro de Ica; 14: Hospital Carlos Monge Medrano; 15: Hospital III EsSalud Juliaca; 16: Hospital III Regional Honorio Delgado; 17: Hospital Hipólito Unanue; 18: Hospital III Daniel Alcides Carrión.
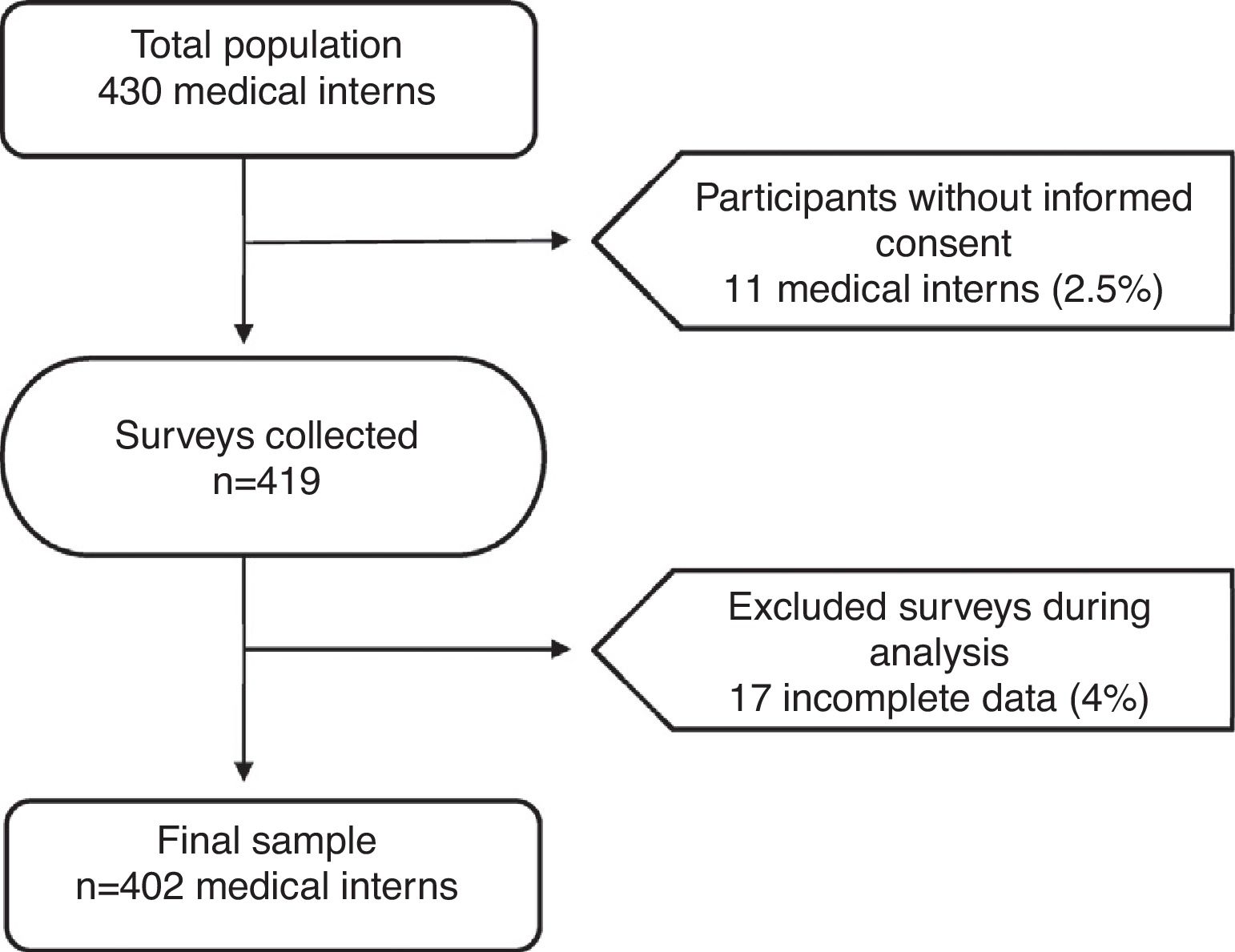
The total population was 430 medical interns, and we proposed a census study. Eleven participants did not provide their informed consent and 17 were excluded because they had not completed the survey correctly. At the end, we analyzed the data of 402 medical interns (figure 2).
Procedures and variablesWe requested the necessary permissions in each hospital. The data were collected by the researchers in 11 Peruvian regions. In some cases, the interviewers had to return more than twice to the hospital due to the low time availability of the medical interns.
We gave each participant in the study the Patient Health Questionnaire-9 (PHQ-9),22 in its Spanish validated version.23 The PHQ-9 consists on 9 items formulated from the DSM-IV diagnostic criteria for depression screening, with an internal consistency from 0.86 to 0.89.24
In the PHQ-9 each item is scored from 0 to 3 (0, not at all; 1, several days; 2, more than half the days, and 3, nearly every day). For screening depression purposes, the total PHQ-9 score is calculated by adding the score of each item, and it ranges from 0 to 27. More than 10 points indicates moderate or high levels of depression.24
Other variables taken into consideration were age, sex, marital status, region of origin, current residence, type of university, current department rotation at the hospital, person with whom the intern lives, presence of adverse events, sleeping hours per day and courses previously disapproved.
We also include the perception of mistreatment (psychological, physical or sexual). Psychological mistreatment was defined as the presence of acts that may damage mental, spiritual or moral sphere. Acts that use physical strength in order to produce damage or pain on another person were considered as physical mistreatment. Finally, sexual harassment was considered as the presence of forced acts not consented by the victim to satisfy sexual needs of the perpetrator.25–30. We used a 20-items questionnaire which was based on similar studies27,28 and had a previous validation in medical students26 with a Cronbach alpha=.8. The instrument was divided in 3 components corresponding to psychological, physical and sexual mistreatment.
Statistical analysisTwo different researchers entered the data in a Microsoft Excel spreadsheet. Both data sets were put together and then reviewed for quality control. The analysis was performed using the statistical package STATA v14.0 (STATA Corp.; College Station, Texas, United States). For the descriptive analysis, we presented the qualitative variables in frequencies and percentages. The quantitative data were presented in medians and ranges, after verifying the absence of normality with the Shapiro-Wilk test.
Our outcome of interest was the presence of depression. The independent variables were selected according to previous studies,3,8–10,13,14,17,21 in order to look for possible associations. We used Poisson regression models with robust variance to calculate the crude (PRc) and adjusted prevalence ratios (PRa) with their respective 95% confidence intervals (95%CI). For the multivariate analysis, we only included the independent variables with P<.05 in the crude analysis. P-values<.05 in adjusted analyses were considered significant.
Ethical aspectsThe study was approved by the Ethics and Research Committee of the Universidad Nacional de Ucayali (Ucayali, Peru). All persons included volunteered to participate in the study. The confidentiality was guaranteed through the use of individual codes for the collection and data analysis. Likewise, we used an informed consent which included information about the study and the voluntary participation of the medical interns.
ResultsGeneral characteristics of the populationWe surveyed 402 medical interns from 18 hospitals in Lima and provinces. The general characteristics of the population are presented in table 1.
Characteristics of the medical interns from Peruvian hospitals (n=402).
| Characteristics | |
|---|---|
| Age (years) | 25 [21-33] |
| Sex | |
| Female | 190 (47.3) |
| Male | 212 (52.7) |
| Marital status | |
| Single | 373 (92.8) |
| Married | 14 (3.5) |
| Cohabiting | 15 (3.7) |
| Region of origin | |
| Coast | 162 (40.3) |
| Mountain region | 155 (38.6) |
| Jungle | 21 (1.4) |
| Current residence | |
| Capital (Lima) | 74 (18.4) |
| Province | 328 (81.6) |
| Type of university | |
| Private | 214 (53.2) |
| Public | 188 (46.8) |
| Department rotation | |
| Pediatrics | 98 (24.4) |
| Surgery | 107 (26.6) |
| Gynecology | 82 (20.4) |
| Internal Medicine | 115 (28.6) |
| Living with: | |
| Father | 21 (5.2) |
| Mother | 51 (12.7) |
| Both parents | 160 (39.8) |
| Alone | 123 (30.6) |
| Others | 47 (11.7) |
| Presence of adverse events | |
| Yes* | 254 (63.2) |
| No | 148 (36.8) |
| Sleeping hours per day | 5 [1-11] |
| Courses previously disapproved | 0 [0-16] |
The most frequent types of mistreatment regarding the psychological component were being shouted (90%) and being treated with apathy (89%). According to the physical component, being assigned excessive work (62%) and being exposed to unnecessary risks were more frequently perceived by medical interns (43%). Finally, regarding the sexual component, receiving sexual or obscene comments (22%) was the most frequently perceived form of mistreatment (figure 3).
Factors associated with depressionWe found that 25.4% of medical interns (n=102) had a positive screening for depression (PHQ-9 score ≥10): 8.5% major depression and 16.9% minor depression. In the adjusted model, we found an association between depression and the age of the participants (PRa=1.15; 95%CI, 1.10-1.21), sex (PRa=3.33; 95%CI, 2.11-5.27) and the sleeping hours per day (PRa=1.23; 95%CI, 1.10-1.38). Likewise, performing the medical internship in provinces decreased in 75% the probability of suffering depression compared to those who lived in the capital (Lima). Also, coming from a public university decreased by 36% the probability of having depression, and those who lived with both parents (PRa=0.65; 95%CI, 0.47-0.91) or alone (PRa=0.33; 95%CI, 0.19-0.58) had lower levels of depression. Finally, perceiving some type of mistreatment during medical internship increased the probability of depression by 7% (table 2).
Factors associated with depression in medical interns of Peruvian hospitals, 2016 (n=402).
| Variable | Crude model | Adjusted model | ||
|---|---|---|---|---|
| PRc | 95%CI | PRa | 95%CI | |
| Age | 1.21 | 1.15-1.28 | 1.15 | 1.10-1.21 |
| Sex | ||||
| Male | Ref. | Ref. | ||
| Female | 3.92 | 2.47-6.20 | 3.33 | 2.11-5.27 |
| Marital status | ||||
| Married | Ref. | Ref. | ||
| Single | 0.68 | 0.33-1.40 | 0.90 | 0.43-1.89 |
| Cohabiting | 1.31 | 0.54-3.18 | 1.04 | 0.48-2.24 |
| Region of origin | ||||
| Coast | Ref. | Ref. | ||
| Mountain region | 1.09 | 0.77-1.56 | 0.97 | 0.71-1.33 |
| Jungle | 0.62 | 0.36-1.07 | 0.70 | 0.42-1.14 |
| Current residence | ||||
| Capital (Lima) | Ref. | Ref. | ||
| Province | 0.21 | 0.16-0.28 | 0.25 | 0.18-0.35 |
| Type of University | ||||
| Private | Ref. | Ref. | ||
| Public | 0.57 | 0.40-0.82 | 0.64 | 0.45-0.88 |
| Department rotation | ||||
| Pediatrics | Ref. | Ref. | ||
| Surgery | 1.15 | 0.72-1.86 | 1.16 | 0.77-1.75 |
| Gynecology | 0.94 | 0.54-1.61 | 1.13 | 0.69-1.87 |
| Internal Medicine | 1.19 | 0.75-1.89 | 1.25 | 0.83-1.89 |
| Courses previously disapproved | 0.97 | 0.86-1.10 | 1.00 | 0.88-1.14 |
| Living with: | ||||
| Mother | Ref. | Ref. | ||
| Father | 0.93 | 0.55-1.58 | 1.00 | 0.69-1.45 |
| Both parents | 0.51 | 0.35-0.75 | 0.65 | 0.47-0.91 |
| Alone | 0.22 | 0.13-0.39 | 0.33 | 0.19-0.58 |
| Others | 0.42 | 0.23-0.77 | 0.56 | 0.30-1.02 |
| Sleeping hours per day | 1.34 | 1.18-1.52 | 1.23 | 1.10-1.38 |
| Suffer or have suffered an adverse event | 0.87 | 0.62-1.22 | 1.04 | 0.78-1.38 |
| Have suffered any type of mistreatment during internship | 1.05 | 1.02-1.08 | 1.07 | 1.03-1.11 |
Depression is a common problem in the last years of the medical career,10 and it is even more frequent during the internship stage.11 In our study, we found that a quarter of the medical interns had a positive screening for depression. These results are consistent with reports in Dubai,31 Israel,32 the United States,30,33 Brazil,10 Chile,34 and Peru,11 suggesting that this problem is frequent in Latin America and even extends to other continents such as Asia.
Similar to our findings, some studies have reported the influence of age on developing depression.30,35 Also, research in Mexico36 and Colombia37 found that women are more vulnerable, which may be due to the influence of certain sociocultural38,39 and biological factors.38,40
We found that living in province was a protective factor. This may be due to the fact that people living in the capital city usually have strenuous and complicated lifestyles,41 which may predispose them to suffer depression.11 Likewise, environmental factors typical of a large city (such as Lima) can directly affect the mental health of the person, causing high rates of burnout.11 However, it is important to mention that the majority of medical interns that participated in this study were from provinces (81.6%), which could have influenced this result.
In our study, coming from a public university was also a protective factor for depression. This may be due to the latent and even innate resilience of the students from public universities, who frequently face adverse situations during their higher education.42 These situations are probably less frequent in private universities, which would explain that when the internship stage arrives, the student from this type of university is “less prepared” to the new lifestyle with the stressors it implies.
We found that living with both parents decreased the likelihood of developing depression compared to those who lived only with their mothers. Firth-Cozenhs43 found that young housewives often feel overloaded, influencing negatively both in their personal lives and in their cohabiting environment, being a predictor related to depression both in housewives and in their family.43 This can be different when cohabitation is with both parents, because it represents a better support network for the medical intern, which may help to better face some problems related to mental health.44 However, we also found that living alone decreased the likelihood of suffering from depressive symptoms, despite some studies that reported that living alone was associated with psychological disadvantages and an increased risk of mental health problems.45 One possible explanation for our findings could be that the intern who lives alone usually has freedom and autonomy about himself. This would involve free decision-making, search for relaxation methods and recreational activities. Therefore, as medical internship is only a one-year program, does not represent a permanent lifestyle.
Previous studies have determined that having few sleeping hours increased the probability of suffering depression, anxiety or even problems of drugs and alcohol abuse.46,47 However, in our study we found an association between more sleeping hours per day and depression. A possible explanation is that there might be an inverse relationship between sleeping hours and study hours. Thus, if the student does not expend the adequate time to study, there will be a negative impact on his/her grades, and some studies discuss the association between depression and poor academic performance.42,48
It is also important to consider that a hierarchical organization, such as the one found in hospitals, facilitates the perpetration of acts of mistreatment, especially when the hospital heads consider such acts as irrelevant or “normal”.21,26 Regarding this, in our study we found that the most frequent type of mistreatment was the psychological one, followed by the physical one. Similar results were reported in two studies conducted in Peru.20,21 These findings show that medical interns are more likely to suffer some type of mistreatment during their duty-hours in the hospital, which is related to the amount of responsibilities and their workload.
Previous studies have identified the existence of mistreatment during medical internship, showing that this would be contributing to the appearance of depression, stress, irritability and loss of motivation towards their work.20,26,49,50 In our study, we corroborate the association between mistreatment and depression. This would serve as an indicator of the possible adverse conditions in which the medical intern works, suggesting an institutional culture in which also highlights the abuse of power.21
Within the limitations of the study was that we only had a population of 11 Peruvian departments (of a total of 24). However, our study included medical interns of the 3 Peruvian regions (coast, mountain region and jungle) which, in general terms, allows our results obtained to come closer to the national reality. We recommend performing a future longitudinal study to identify other important factors that trigger depression. Also, although the PHQ-9 is a validated tool which had demonstrated usefulness for the screening of depression, it is important to consider that depression is a complex disorder which diagnosis needs a complete psychopathological exploration.
ConclusionsWe found that a quarter of medical interns surveyed had a positive screening for depression. The factors associated with this condition were being a woman, having perceived some type of mistreatment, age and the sleeping hours per day. On the other hand, carrying out the internship in provinces, coming from a public university, living alone or with both parents were protective factors.
Conflict of interestsNone.