The prevalence of falls in RA patients ranges from 14.3% to 54%. Some tools for assessing falls risk predict this in the elderly population. As RA usually begins at a younger age, it would be worth exploring the risk of falls in this age set of patients. Downton index>3 and a Tinetti scale<18 are predictive of fall risk. The study aims to determine the association of RA disease activity and health assessment with falls risk.
Materials and methodsObservational, cross-sectional study in RA patients. Demographics, DAS28, HAQ-DI medications, Tinetti scale, and Downton index were obtained.
ResultsWe included 108 patients, 98 (90.7%) were women. Patients’ mean age was 52.5±10.8 years. Median DAS-28 and HAQ-DI scores were 3.6 and .81. Sixty (55.6%) patients had previous falls. We observed a positive significant correlation between the Downton index and patient's age (rho=.44, p<.001), RA diagnosis time (rho=.23, p=.014), RA activity (DAS-28 score) (rho=.61, p<.001), and a HAQ-DI score (rho=.709, p<.001). Overall, the total Tinetti evaluation scale was significantly correlated with age (rho=−.36, p<.001), time since RA diagnosis (rho=−.20, p=.031), RA activity (DAS-28 score) (rho=−.77, p<.001), and HAQ-DI score (rho=−.835, p<.001). After a multivariate analysis, we found that for a high risk of falls by Downton score, age>52 years had an OR 7.5 (95% CI, 3.1–17.7; p=.001), a DAS-28>3.5 had an OR 9.1 (95% CI, 3.7–22.1; p=.02), and a HAD-QI>.94 had an OR 27.9 (95% CI, 7.1–100.9; p=.001). For a Tinetti score that predicts risk of falls, a HAD-QI>1.44 had an OR 1.8 (95% CI, 1.28–2.52; p=.001).
ConclusionsThere is a correlation between DAS-28 and HAD-QI scores and risk of falls in younger RA patients. The DAS-28 and HAD-QI can predict falls risk using surrogate scales. The risk of falls is an assessment that should be considered RA patients.
La prevalencia de caídas en pacientes con artritis reumatoide (AR) oscila entre el 14,3 y el 54%. Algunas herramientas para evaluar el riesgo de caídas se emplean en adultos mayores. Como la AR generalmente comienza a una edad más temprana, valdría la pena explorar el riesgo de caídas en este grupo de edad. El índice de Downton > 3 y una escala de Tinetti <18 predicen el riesgo de caídas. El estudio tiene como objetivo determinar la asociación de la actividad de la enfermedad de AR y la evaluación de la salud con el riesgo de caídas.
Materiales y métodosEstudio observacional, transversal en pacientes con AR. Se obtuvieron datos demográficos, DAS-28, medicamentos HAQ-DI, escala de Tinetti e índice de Downton.
ResultadosSe incluyeron 108 pacientes, 98 (90,7%) eran mujeres. La edad media de los pacientes fue 52,5±10,8 años. Las medianas de las puntuaciones DAS-28 y HAQ-DI fueron 3,6 y 0,81; 60 (55,6%) pacientes tuvieron caídas previas. Observamos una correlación significativa positiva entre el índice de Downton y la edad del paciente (rho=0,44, p<0,001), el tiempo de diagnóstico de la AR (rho=0,23, p=0,014), la actividad de la AR (puntuación DAS-28) (rho=0,61, p<0,001) y una puntuación HAQ-DI (rho=0,709, p<0,001). En general, la escala de evaluación total de Tinetti se correlacionó significativamente con la edad (rho=-0,36, p<0,001), el tiempo desde el diagnóstico de la AR (rho=-0,20, p=0,031), la actividad de la AR (puntuación DAS-28) (rho=- 0,77, p<0,001) y la puntuación HAQ-DI (rho=-0,835, p<0,001). Tras un análisis multivariado, se encontró para un alto riesgo de caídas según el puntaje de Downtown, una edad > 52 años con OR 7,5 (IC 95%, 3,1-17,7; p=0,001), DAS-28 >3,5 con OR 9,1 (IC 95%, 3,7-22,1; p=0,02), y HAD-QI >0,94 con OR 27,9 (IC 95%, 7,1-100,9; p=0,001). Para un puntaje de Tinetti que predice el riesgo de caídas, un HAD-QI >1,44 con OR 1,8 (IC 95%, 1,28-2,52; p=0,001).
ConclusionesExiste una correlación entre las puntuaciones DAS-28 y HAD-QI y el riesgo de caídas en pacientes más jóvenes con AR. El DAS-28 y HAD-QI pueden predecir un riesgo de caídas con escalas surrogadas. El riesgo de caídas es una valoración que deben considerar los pacientes con AR.
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease with an autoimmune etiology, characterized by inflammation and proliferation of the synovial membrane of diarthrodial joints. It evolves in joint destruction and deformities, disability, and decreased life expectancy. RA patients present a considerable decrease in their quality of life and increased dependence on caregivers.1
The definition of a fall, according to the World Health Organization, is “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.” Falls are the second leading cause of accidental or unintentional injury deaths worldwide and are a public health problem. Fall-related injuries may be fatal, though most are non-fatal, but they can be severe enough to require medical attention.2
Falls can have physical, psychological, and social consequences. Individuals with RA have a high risk of falls because of a difficulty in maintaining postural control, and impairing balance in activities of daily living.3–5 Mamoto et al. did not observe a higher incidence rate of falls in well-controlled RA patients (HAQDI of 0.25) compared to controls.6 Although falls are associated with the elderly, middle-aged RA patients also suffer from falls, and almost two-thirds of patients experience fear related to falling.7,8 Some previously described non-RA related fall risk factors include a history of prior fall, medications, unsteady gait, environmental hazards, fair or poor health status perception, and use of a cane, walker, or crutches, while RA-related factors involve chronic hip pain, number of joint involvement, and muscle pain and atrophy.9
Some tools for assessing falls risk are useful to predict it in the elderly population.10 As RA usually begins before the age of 60, it would be worthy to explore these factors in RA patients. It is noteworthy to consider that the prevalence of falls in RA patients ranges from 14.3 to 54% in over a one-year period, which is higher compared to the age-matched population.4,5,7,11 The study aims to determine the association of disease activity, health assessment status, and the risk of falls (geriatric tools), to explain the high prevalence of falls in RA patients.
MethodsWe conducted an observational, cross-sectional study of RA patients attending a General Hospital of the Mexican Social Security Institute in Northern Mexico. We applied surveys between August and October 2016 in patients who met the RA 2010 ACR/EULAR classification criteria.12 This study was approved by the local ethics committee (approval code: R-2017-1904-99).
Patients with diagnosed RA of both genders over 18 years of age were included. A certified rheumatologist confirmed the RA diagnosis and performed the clinical evaluation (joint count) to assess disease activity. Patients were excluded if they had wheelchairs use, amputated lower extremity, and those whose educational level did not allow them to answer the questionnaires or who suffered from a mental disease that prevented them from consciously participating.
From the RA patient cohort clinic (216 regular attending patients), we calculated a sample from a simple random probabilistic sampling, with an estimate of 108 individuals. The number was based on a sample proportion calculation for an expected fall prevalence of 17% with an 80% statistical power and 5% significance level.
We applied a questionnaire to obtain demographic variables, such as age and gender. We also obtained the Disease Activity Score (DAS-28)13 and the Spanish version of the Stanford Health Assessment Questionnaire-Disability Index (HAQ-DI).14 The HAQ-DI consists of 20 items that evaluate the self-perceived degree of difficulty (physical disability) in performing activities of daily living grouped into 8 categories: dressing, rising, eating, walking, hygiene, reach, grip, and usual activities. DAS-28 and HAD-QI scores were evaluated at the time of the inclusion of the patient in the study, regardless its time of evolution or prior treatments (which are only described for the purpose of this study). The questionnaires were applied only by a previously trained physician (OMD). All patients filled out written informed consent before participating.
We directly asked any history of falls in the previous year. We assessed the risk of falls through the Tinetti scale and Downtown fall risk index. The Tinetti scale assesses both gait and balance,15–17 and along with the Downton fall risk index,18,19 they were applied by a trained physician (OMD). The Tinetti scale is used to determine the risk of an early fall in an older person. The Tinetti test has a gait score and a balance score. It uses a 3-point ordinal scale of 0, 1, and 2. Gait is scored over a maximum score of 12, and balance is scored maximum score of 16, totaling 28 points. A score≤18 on the Tinetti test has is associated with a higher the risk of falling, 19–23 with an intermediate-risk, and ≥24 with a low risk of falling.15 The Downton scale is used to assess a person's risk of falling. It consists of 5 items: previous falls, medication, sensory deficits, mental state, and ambulation, in a dichotomous way. If the score of the scale is three or more points, the patient is considered with a high risk of falling.20
The results were analyzed with the SPSS version 20 statistical program using measures of central tendency (mean, median) and measures of dispersion (standard deviation, interquartile interval) for quantitative variables, and frequency and proportions for qualitative variables. We tested for normal distribution for each quantitative variable with the Kolmogorov–Smirnov test. After identification of a non-parametric distribution among evaluated scores (DAS28, Tinetti, Downton, and HAQ-DI), we used Spearman correlation coefficient (rho) to assess the level of correlation of these with other patient quantitative factors. The correlation was defined according to the following values: 0–0.5 null, 0.5–0.25 low, 0.25–0.50 medium, 0.50–0.75 moderate and 0.75–1 high. We performed a receiver operator curve (ROC) analysis to identify the prediction yield of several variables for risk of falls by Downtown and Tinetti scales; we obtained an area under the curve (AUC) and selected the cut-off point with highest Youden index for sensibility (Sen) and specificity (Spe). Then, we performed a multivariate analysis through multivariate logistic regression with these cut-off points to select the best predictive model of risk of falls for each scale and reported each odds ratio (OR). We considered a p<0.05 and a confidence interval of 95% (95% CI) as statistically significant.
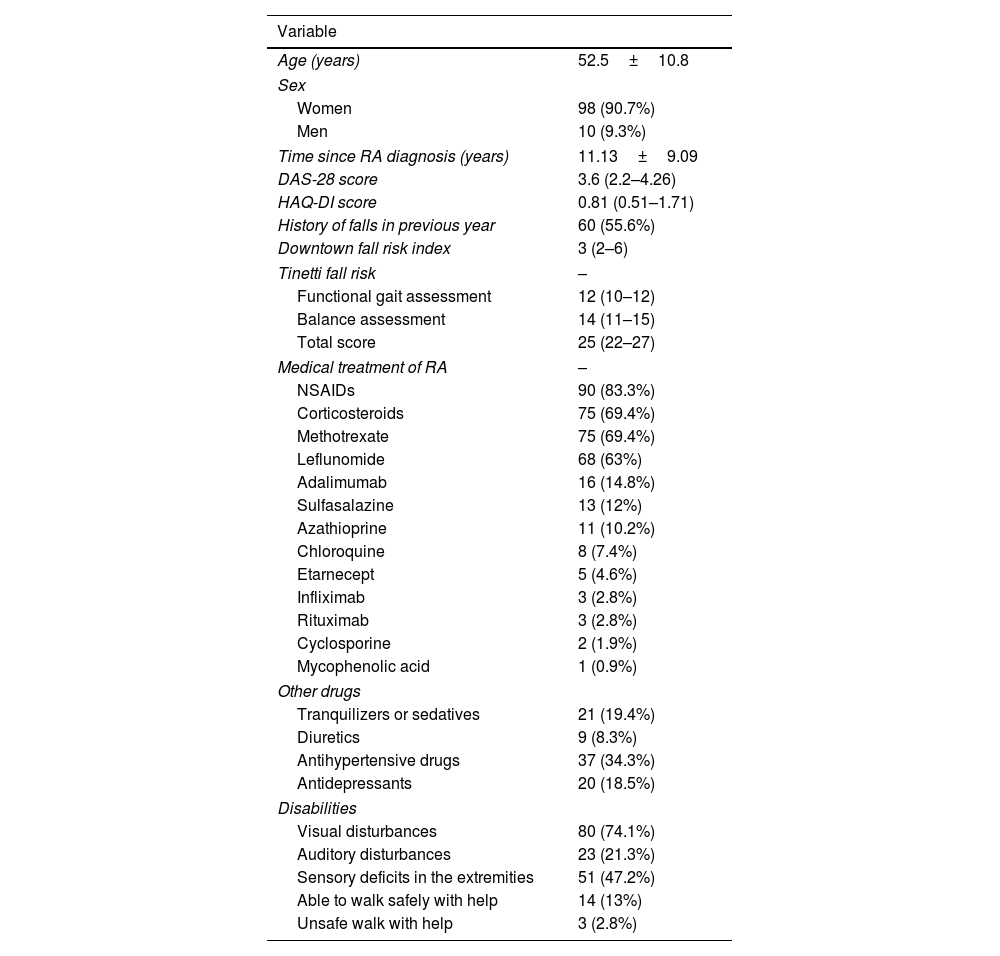
ResultsPatient characteristicsWe included 108 patients, 98 (90.7%) were women. Patients’ mean age was 52.5±10.8 years, ranging from 21 to 77 years. Patients’ characteristics are resumed in Table 1. The mean time since the diagnosis of RA was 11.13±9.09 years. The median of the DAS-28 was 3.6 and HAQ-DI median score of 0.81.
Patient demographic characteristics.
| Variable | |
|---|---|
| Age (years) | 52.5±10.8 |
| Sex | |
| Women | 98 (90.7%) |
| Men | 10 (9.3%) |
| Time since RA diagnosis (years) | 11.13±9.09 |
| DAS-28 score | 3.6 (2.2–4.26) |
| HAQ-DI score | 0.81 (0.51–1.71) |
| History of falls in previous year | 60 (55.6%) |
| Downtown fall risk index | 3 (2–6) |
| Tinetti fall risk | – |
| Functional gait assessment | 12 (10–12) |
| Balance assessment | 14 (11–15) |
| Total score | 25 (22–27) |
| Medical treatment of RA | – |
| NSAIDs | 90 (83.3%) |
| Corticosteroids | 75 (69.4%) |
| Methotrexate | 75 (69.4%) |
| Leflunomide | 68 (63%) |
| Adalimumab | 16 (14.8%) |
| Sulfasalazine | 13 (12%) |
| Azathioprine | 11 (10.2%) |
| Chloroquine | 8 (7.4%) |
| Etarnecept | 5 (4.6%) |
| Infliximab | 3 (2.8%) |
| Rituximab | 3 (2.8%) |
| Cyclosporine | 2 (1.9%) |
| Mycophenolic acid | 1 (0.9%) |
| Other drugs | |
| Tranquilizers or sedatives | 21 (19.4%) |
| Diuretics | 9 (8.3%) |
| Antihypertensive drugs | 37 (34.3%) |
| Antidepressants | 20 (18.5%) |
| Disabilities | |
| Visual disturbances | 80 (74.1%) |
| Auditory disturbances | 23 (21.3%) |
| Sensory deficits in the extremities | 51 (47.2%) |
| Able to walk safely with help | 14 (13%) |
| Unsafe walk with help | 3 (2.8%) |
Sixty (55.6%) patients had previous falls. Median Downton fall risk index was 3; median functional gait assessment of the Tinetti fall risk index was 12, 62 (57.4%) patients with a score >3; and median balance assessment was 14, and median total assessment of gait and balance with the Tinetti fall risk index was 25, twelve (11.1) patients had a total score<18.
Overall, the most frequently employed RA medication were NSAIDs in 90 (83.3%), corticosteroids in 75 (69.4%) (with a mean prednisone daily dose of 5mg), methotrexate 75 (69.4%) and leflunomide 68 (63%). We found that 21 (19.4%) used tranquilizers or sedatives; 9 (8.3%) used diuretics; 37 (34.3%) used antihypertensive drugs; 20 (18.5%) used antidepressants; and 53 (49.1%) used other drugs. Regarding sensory deficits, 80 (74.1%) had visual disturbances, 23 (21.3%) auditory disturbances, 51 (47.2%) sensory deficits in the extremities. Also, 14 (13%) were able to walk safely with help, and 3 (2.8%) had an unsafe walk with help, and no patient had an altered mental state.
Functional assessment of gait and balanceGait assessment with the Tinetti fall risk indexIn the initial gait, 5 (4.6%) had some hesitation or needed multiple attempts to start. In the length and height of the step, 100 (92.6%) exceeded the left foot and the right foot and wholly separated from the ground, 99 (91.7%) exceeded the right foot and the left foot and wholly separated from the ground, in 99 (91.7%) patients, step length seemed equal. In 95 (88%) cases the steps seemed continuous, 82 (75.9%) presented a trajectory without deviations or the use of aids; 85 (78.7%) did not unbalance, flex, or use other aids when walking.
Balance assessment with the Tinetti fall risk indexConcerning sitting balanced, 54 (50%) were able to maintain balance, but use their arms to help them; 52 (48.1%) were able to sit without using their arms, 93 (86.1%) were able to get up in one attempt, and once standing, 91 (84.3%) had a stably maintained balance without using a cane or other objects, and 90 (83.3%) continued to walk stably without a walker or other support.
When the patient got a small push against the sternum three times, 67 (62%) maintained their balance. With eyes closed, 96 (88.9%) remained stable. When making a 360° turn, 16 (14.8%) had discontinuous and unstable steps (wobble or grip), 35 (32.4%) had continuous and unstable steps (wobble or grip), and 57 (52.8%) had continuous and stable steps. When sitting, only 1 (0.9%) patient was insecure and miscalculated the distance.
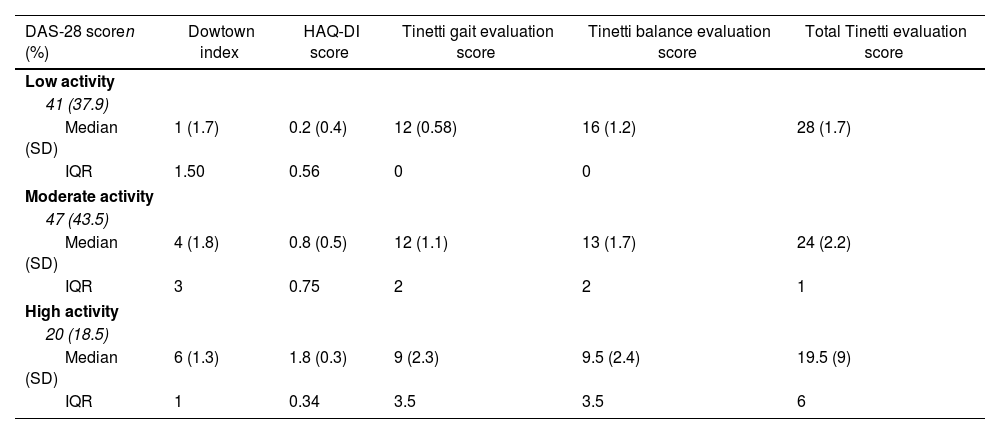
The characteristics of the risk scales stratified by disease activity are resumed in Table 2.
Falls risk scales stratified according to disease activity.
| DAS-28 scoren (%) | Dowtown index | HAQ-DI score | Tinetti gait evaluation score | Tinetti balance evaluation score | Total Tinetti evaluation score |
|---|---|---|---|---|---|
| Low activity | |||||
| 41 (37.9) | |||||
| Median (SD) | 1 (1.7) | 0.2 (0.4) | 12 (0.58) | 16 (1.2) | 28 (1.7) |
| IQR | 1.50 | 0.56 | 0 | 0 | |
| Moderate activity | |||||
| 47 (43.5) | |||||
| Median (SD) | 4 (1.8) | 0.8 (0.5) | 12 (1.1) | 13 (1.7) | 24 (2.2) |
| IQR | 3 | 0.75 | 2 | 2 | 1 |
| High activity | |||||
| 20 (18.5) | |||||
| Median (SD) | 6 (1.3) | 1.8 (0.3) | 9 (2.3) | 9.5 (2.4) | 19.5 (9) |
| IQR | 1 | 0.34 | 3.5 | 3.5 | 6 |
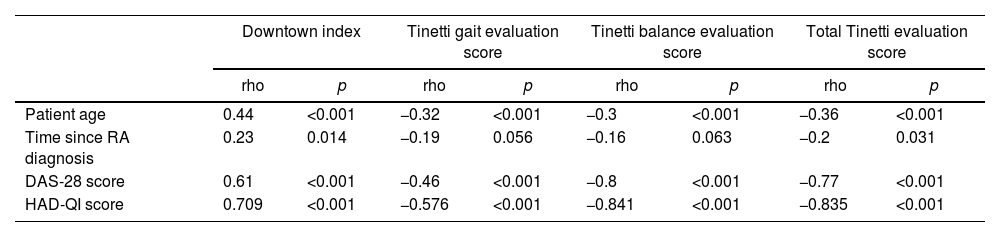
We observed a positive significant correlation between the Downton index and patient's age (medium) (rho=0.44, p<0.001), RA diagnosis time (low) (rho=0.23, p=0.014), RA activity (DAS-28 score) (moderate) (rho=0.61, p<0.001), and a HAQ-DI score (moderate) (rho=0.709, p<0.001). We also observed a significant negative correlation between the Tinetti gait and the balance evaluation score and age, RA activity (DAS-28 score), and HAQ-DI. Overall, the total Tinetti evaluation scale was significantly correlated with age (medium) (rho=−0.36, p<0.001), time since RA diagnosis (low) (rho=−0.20, p=0.031), RA activity (DAS-28 score) (high) (rho=−0.77, p<0.001), and HAQ-DI score (high) (rho=−0.835, p<0.001) (Table 3).
Correlation analysis between RA activity and disability scores and risk of falls scores.
| Downtown index | Tinetti gait evaluation score | Tinetti balance evaluation score | Total Tinetti evaluation score | |||||
|---|---|---|---|---|---|---|---|---|
| rho | p | rho | p | rho | p | rho | p | |
| Patient age | 0.44 | <0.001 | −0.32 | <0.001 | −0.3 | <0.001 | −0.36 | <0.001 |
| Time since RA diagnosis | 0.23 | 0.014 | −0.19 | 0.056 | −0.16 | 0.063 | −0.2 | 0.031 |
| DAS-28 score | 0.61 | <0.001 | −0.46 | <0.001 | −0.8 | <0.001 | −0.77 | <0.001 |
| HAD-QI score | 0.709 | <0.001 | −0.576 | <0.001 | −0.841 | <0.001 | −0.835 | <0.001 |
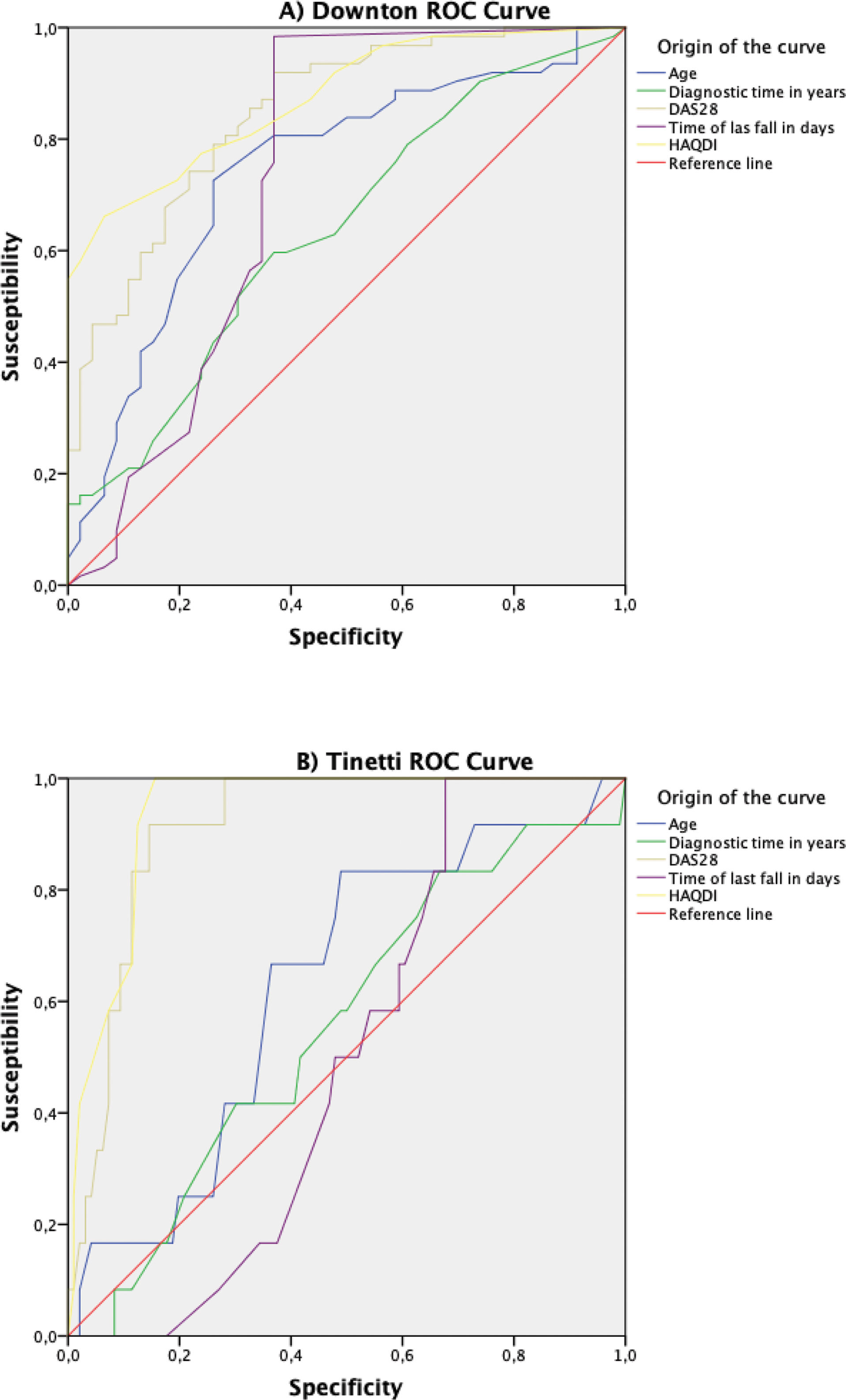
We applied the Downton score, considering a threshold greater than 3 as indicative of high risk. Our analysis yielded the following AUC for various variables: age, AUC=0.742 (p=0.001, 95% CI 0.646–0.839); time to diagnosis of RA, AUC=0.637 (p=0.015, 95% CI 0.532–0.742); DAS28, AUC=0.848 (p=0.001, 95% CI 0.776–0.920); HAQ-DI, AUC=0.873 (p=0.001, 95% CI 0.810–0.936). Additionally, we assessed the relationship between the Tinetti scale scores and fall risk, finding a direct negative correlation. A Tinetti score of ≤18 was considered indicative of higher fall risk. The AUC values for this assessment were as follows: age, AUC=0.630 (p=0.144, 95% CI 0.474–0.786); time to diagnosis of RA, AUC=0.555 (p=0.535, 95% CI 0.391–0.719); DAS28, AUC=0.912 (p=0.001, 95% CI 0.853–0.971); HAQ-DI, AUC=0.938 (p=0.001, 95% CI 0.892–0.984) (Fig. 1).
ROC curves for risk of falls through Downton and Tinetti scales. (A) Yield of age, diagnostic time, DAS-28, time of last fall and HAD-QI for risk of falls through Downton scale. (B) Yield of age, diagnostic time, DAS-28, time of last fall and HAD-QI for risk of falls through Tinetti scale. DAS28, Disease Activity Score 28; HAQ-DI, Health Assessment Questionnaire Disability Index.
For a Downtown score >3, we obtained the following cut-off points: age, 52.5 years (Sen=0.726 and Spe=0.739, Youden index=0.465); time to diagnosis of RA, 9.5 years (Sen=0.597, Spe=0.630, Youden index=0.227); DAS28, 3.545 (Sen=0.742, Spe=0.783, Youden index=0.525); HAQ-DI, 0.940 (Sen=0.661, Spe=0.935, Youden index=0.596). For a Tinetti score≤18, we obtained the following cut-off points: DAS28, 4.10 (Sen=1.000, Spe=0.719, Youden index=0.719); HAQ-DI, 1.44 (Sen=1.000, Spe=0.844, Youden index=0.844).
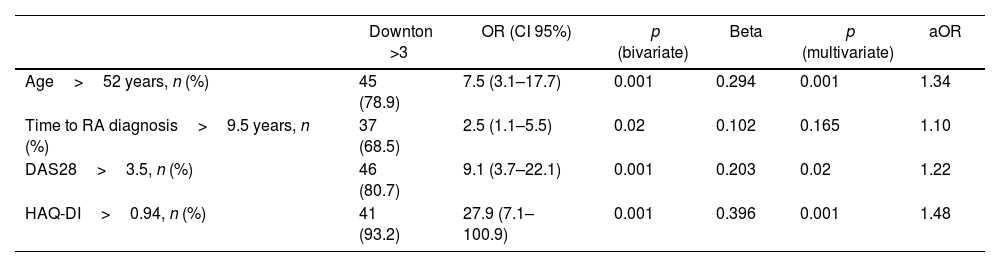
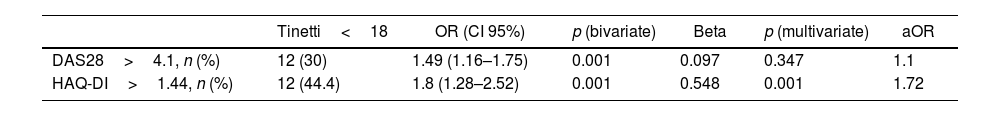
Multivariate prediction of risk of fallsAfter a multivariate analysis, we found that for a high risk of falls by Downtown score, an age>52 years had an OR 7.5 (95% CI, 3.1–17.7; p=0.001), a DAS-28>3.5 had an OR 9.1 (95% CI, 3.7–22.1; p=0.02), and a HAD-QI>0.94 had an OR 27.9 (95% CI, 7.1–100.9; p=0.001) (Table 4). For a Tinetti score that predicts risk of falls, a HAD-QI>1.44 had an OR 1.8 (95% CI, 1.28–2.52; p=0.001) (Table 5).
Bivariate and multivariate analysis to associate high fall risk by Downton score.
| Downton >3 | OR (CI 95%) | p (bivariate) | Beta | p (multivariate) | aOR | |
|---|---|---|---|---|---|---|
| Age>52 years, n (%) | 45 (78.9) | 7.5 (3.1–17.7) | 0.001 | 0.294 | 0.001 | 1.34 |
| Time to RA diagnosis>9.5 years, n (%) | 37 (68.5) | 2.5 (1.1–5.5) | 0.02 | 0.102 | 0.165 | 1.10 |
| DAS28>3.5, n (%) | 46 (80.7) | 9.1 (3.7–22.1) | 0.001 | 0.203 | 0.02 | 1.22 |
| HAQ-DI>0.94, n (%) | 41 (93.2) | 27.9 (7.1–100.9) | 0.001 | 0.396 | 0.001 | 1.48 |
This study provides that HAQ-DI and DAS-28 could correlate with the risk of falls in RA patients. We also observed that age of RA patients is indeed correlated with scores of risk of falling in a younger age group. Stanmore et al.,21 as Bugdayci et al.,22 evaluated RA patients and determined the incidence of falls, and established that the main factor in presenting a fall is the history of the previous one. Fesell and Nevitt demonstrated that RA patients over 50 years had a 50% fear of falling, and 38% modified their daily activities.23 In addition, the risk of falling could be related to decreased grip strength,24 which is a common situation among RA patients. Furthermore, it is crucial to address and detect this risk in our patients.
A systematic review of the literature suggests that falls incidence is independent of gender and RA disease duration. Female gender is associated with increased falls risk in healthy older adults. Disability in RA generally are associated with increasing length of the disease.5 In our study, 90% of participants were women, which could most easily extrapolate to a female population group.
To evaluate the self-perceived degree of difficulty (physical disability) causing by RA or other chronic diseases that impair functional status, we used the HAQ-DI, which was relatively low (with a mean score of 0.85 points) in comparison to other authors.9 We found the HAQ-DI was statistically correlated with the risk of falls, according to the Downton Scale and the Tinetti scale. Fessel found that a higher HAQ-DI predicts the fear of falling, as well as the history of a previous one.23 However, Hayashibara found no relationship between functional disability and the presence of falls, since five of the eight HAQ categories assess the function of the upper limbs.25 In our study, correlations were found between a lesser total Tinetti score with older age, and the higher DAS-28, according to Stanmore.21
RA patients had an increased number of falls. Smulders et al.9 compared the clinical profile between fallers and non-fallers; and determined that the visual analog scale (VAS) for pain and fall history were the main predictors to fall. But, they not evaluated the fall risk nor used a geriatric validated scale. Bugdayci22 described the RA population and found that falls correlated with age, VAS for pain, previous falls, use of assistive devices for ambulation, use of two or more medications, and ability to do heel–toe walking.
We used Downton and Tinetti based on the expertise in our center. Although these are scales validated and performed for geriatric populations, we believed these were the most available tools to address the risk of falls in a population group in which it is not usually evaluated and to our knowledge, there is not any other validated tool for this age group. In a meta-analysis is recommended the combination use of the Timed Up and Go test, which has stable sensitivity, and the Berg Balance Scale, which has a relatively increased diagnostic accuracy. The Downton and Tinetti scales have been used mainly in patients diagnosed with Multiple Sclerosis, Parkinson's disease, acquired brain injury, spinal cord injury, stroke, and the elderly population. Nonetheless, Downton scale had an overall sensitivity of 84% and Tinetti 68%. But these values are evaluated in a geriatric sample. It recommended that two assessment tools used together to evaluate the characteristics of falls in the elderly for predicting the occurrence of falls, as we did in our study.10
The Downton scale has been designed to assess fall risk in the elderly. But we found that RA patients are indeed, at a risk of falls despite their mean younger age (53 years). The mean of the Downton scale in our study was 3.44, considering that equal or above 3 points it is considered in a higher risk of falls. Of all RA patients, at least 51% reported using one or more medications such as tranquilizers/sedatives, diuretics, antihypertensive drugs, and antidepressants. Other authors also have found an increased fall risk associated with a previous history of falls and polypharmacy.4 The consumption of these drugs was evaluated by the Downton scale, as they contribute to the risk of falls.
We have a significant association of risk falls by Downton scale in patients older than 52 years, more than 9.5 years of duration of the disease, but it was stronger for DAS28>3.5, HAQ-Di>0.94 with OR of 7.5, 2.5, 9.1 and 27.9 respectively. But after multivariate analysis, only age>51 years old, DAS28>3.5, and HAQ>0.94 were statistically significant. A HAQ-DI score>0.94 has a sensitivity of 0.66 and specificity of 0.935 to predict a Downton scale>3, hence risk fall. We choose the Tinetti Scales, which has better test–retest, discriminative and predictive validities concerning fall risk than other tests, including time Up and Go (TUG) test, one-leg stand, and functional reach test. Böhler C et al. has used the Tinetti test. In RA patients,8 they found that patients with higher disease activity achieved more inferior results in the Tinetti fall assessment. They as same us in our study, and also found that HAQ scores correlated with this tool.8
In our study, we were not able to give an objective incidence of falls over the last 12-month period, but we can record that sixty (55.6%) patients had previous falls according to their self-report. These findings are similar to reported in the study of Hayashibara et al.,25 who found that 50% of RA patients had one or more falls in a year. Clinic-based studies have examined the prevalence of falls in adults with RA.7,26 Jamison et al. reported that thirty-five percent of falls.7 This percentage is higher than the 30% reported among elderly RA patients, which is similar to the 28–52% reported among older and elderly persons living in the community.27,28 However, a study prospective of RA-controls there was not found differences in the incidence rate of falls between patients with RA and control over 4-years follow up period.6 This study showed that the titles of the anti-CCP antibody level of more than 300U/ml were the most reliable predictor for multiple falls among RA patients.6 In our study, the frequency and percent of patients with titles above this level were not considered. Other prospective studies reported frequencies from 32% to 41% of falls during the 1-year follow up period. They reported 1.11 risks of falls per person, which result in 5% of head injuries or fractures. And almost 9% requested emergency services.21 Although a small percentage of falls result in fractures, it may lead to fear of falling, restriction of activities, hopelessness, and reduced mobility in the long term.22 Vertebral and hip fractures are increased in RA patients, and the risk is related to low bone mineral density and increased risk of falls.11,29
The fear of falling is asked on the Tinetti scale. Fear of falling had a predictive value for the future falls from 63% to 87% in the elderly.7 In our study, in initial gait, 5 patients (4.6%) had some hesitation or needed multiple attempts to start. One fifth had some trouble in balance, flexing, or use other aids when walking. Concerning sitting balanced, half were able to maintain balance, but use their arms to help them; half patients were able to sit without using their arms, possibly related to lower limb joint pain and inflammation due to RA.21,30
Lourenco et al. found an increased fall risk associated with a previous history of falls and polypharmacy. There was no association with disease activity or disease duration, functional capacity, physical performance, and age or gender, that can be due to an activity restriction, and hence, reduced exposure to risk of falls situations.4 They used other tools as the Berg Balance Scale, TUG, 6-Minute Walk, and Short Physical Performance Battery tests, which were not used in our study.
Daily and cumulative glucocorticoid (GC) dosage has been reported to be associated with an increased risk of falling. It is accompanied by an increased risk of fractures, as well as other factors: older age (>60 years), overweight, deficits in muscle strength, and sarcopenia.11,31,32 We found 75 patients on corticosteroids, with a mean dose of 5mg of prednisone. According to Yamada, doses greater than 3.25mg per day of prednisone had an association with sarcopenia, a plausible surrogate of fall risk.31 In our study, this effect was not considered, although the majority of patients reported corticosteroid consumption.
The foot is a common site of pathology in the early stages of RA, and its involvement becomes more significant with disease progression.33 Foot deformity and altered function may also affect balance and increase the risk of falls, but these variables were not taken into account in our study. We assume that these foot deformities are probably minimal since our population did not have a high HAQ-DI score, and their time of evolution of RA was around 10 years. The joint counts in the DAS28 do not consider the feet involvement, which could be an underestimate for assessing risk of falls when taking into account the integrity and functionality of the foot in the basis of the risk of falls. Also, other factors like the physical deconditioning associated with inactivity may increase fear of falling,7,9 which was not taken into account and participants could have had a memory risk of bias when assessing for recent history of falls.
The risk of falls is an assessment that should be considered RA patients, because the complications of falling in a younger age group could lead to earlier disability and have a great impact on the quality of life of a RA patient. Prospective studies are needed to obtain more definitive conclusions regarding the role of these scales with the risk of falling. And also exists the need to develop fall prevention programs for RA patients with a history of falls to improve their independence and mobility.
ConclusionsThere is a relation between DAS-28 and HAD-QI scores and risk of falls in younger RA patients. The DAS-28 and HAD-QI could predict fall risk using surrogate scales (Downtown, Tinetti). The risk of falls is an assessment that should be considered RA patients.
What is already known about this subject?
- •
RA patients had an increased fall risk. Downton and Tinetti scores had been validated to assess fall risk in the elderly.
What does this study add?
- •
This study provides that HAQ-DI and DAS-28 correlate with scores of risk of falls, in RA patients.
- •
We showed that younger RA patients have a risk of falls that should be assessed.
- •
A cut off of 0.94 and 1.44 of the HAQ-DI score is predictive for the Downton score of >3 and a Tinetti scale <18 points, respectively.
How might this impact on clinical practice or further developments?
- •
There is a correlation between DAS-28 and HAD-QI scores and risk of falls in younger RA patients. The risk of falls is an assessment that should be considered RA patients.
All patients filled out written informed consent. The study was approved by the Local Ethics Committee with number R-2017-1904-99.
FundingNot apply.
Conflicts of interestThe authors declare that they have no competing interests.
None.