Sjögren syndrome (SS) is an autoimmune disease, rarely affecting the central nervous system. The case is reported on a 68-year-old male patient who presented with keratoconjunctivitis sicca and xerostomia, during neuropsychological evaluation showed moderate to severe multidomain cognitive impairment. The magnetic resonance showed evidence of hypertrophic pachymeningitis. The CSF study showed pleocytosis, mild proteinuria, and negative cultures. The immune positive profile, Anti SS-A, SS-B and salivary gland biopsy was compatible with SS. The treatment was started with methylprednisolone pulses at a dose of 1g every 24h for three days, and controlled with maintenance therapy, showing a favorable response. Chronic meningitis is a diagnostic challenge; among the less common causes is hypertrophic pachymeningitis in SS, and less frequently in male patients (1/9). Non-specific neurological manifestations should be considered, such as headaches or neuropsychiatric symptoms, as on some occasions rare cases may be encountered, such as the one described.
El síndrome de Sjögren (SS) es una enfermedad autoinmune que rara vez afecta al sistema nervioso central. En este informe de caso describimos a un paciente varón, de 68 años, que presentó queratoconjuntivitis seca y xerostomía, y a la evaluación neuropsicológica mostró deterioro cognitivo multidominio en grado de moderado a grave. La resonancia magnética mostró evidencia de paquimeningitis hipertrófica. El estudio del LCR mostró pleocitosis, proteinuria leve y cultivos negativos; el perfil inmunológico positivo anti SS-A, SS-B y la biopsia de la glándula salival compatible con SS. El tratamiento se inició con pulsos de metilprednisolona a una dosis de 1g/cada 24h/durante 3 días, control con terapia de mantenimiento, mostrando una respuesta favorable. La meningitis crónica es un desafío para el diagnóstico, entre las causas menos frecuentes está la paquimeningitis hipertrófica en el SS, y con menor frecuencia en los pacientes varones (1/9). Se deben considerar manifestaciones neurológicas inespecíficas, como dolores de cabeza o síntomas neuropsiquiátricos, ya que en algunas ocasiones podemos enfrentarnos a casos raros como el descrito.
Chronic meningitis is a persistent meningeal irritation and inflammation of more than four weeks associated with cerebrospinal fluid pleocytosis. Due to the diverse etiologies, a systematic diagnostic approach is required based on a thorough anamnesis, rigorous clinical examination, patient's immune status assessment, epidemiological data, etc. Among the autoimmune causes, Sjögren's syndrome is a rare etiology.1 Primary Sjögren's Syndrome (pSS) is a low-prevalent chronic autoimmune disease (61/100000 people with a female: male ratio 9:1). Lymphocytic infiltration in the exocrine glands, manifesting xerostomia and dry keratoconjunctivitis are distinctive features.2 Extraglandular manifestations can occur in one third of patients with pSS. Between 8.5% and 67% of patients with Sjögren's syndrome develop central nervous system involvement with meningeal injury being 20%.3 Sjögren's sydrome could affect the peripheral as well as the central nervous system. The most frequent peripheral nervous system manifestations are sensory neuronopathy, small fiber polyneuropathy and autonomic neuropathy. On the other hand the most frequent SNC manifestations are cognitive, neuropsychiatric and multifocal (mutiple sclerosis like).4,5
In particular, diffuse non-focal neurological signs and symptoms are considered more prevalent.5 The majority of reported cases describe acute, subacute or recurrent symptoms, providing limited information about the clinic and follow-up of chronic conditions. In addition, there are few cases of hypertrophic pachymeningitis associated with pSS. Here, we report the case of a male patient with chronic meningitis as the main manifestation of pSS.
Case reportA 68-year-old, right-handed male from Callao-Peru, presented to consultation complaining bilateral oppressive headache, nausea, dizziness, retroocular pain associated with mild conjunctival erythema and low-grade fever. Symptoms developed insidiously five months before, triggered bilateral hearing loss, left hemiparesthesia, increased intensity of headache, and a seizure with brief loss of consciousness. The patient's vital signs as well as his neurological assessment were unremarkable. Physical examination revealed bilateral hearing loss, skin peeling with plaques of the nasal and bilateral retro-auricular area. Normal examination of cardiac, respiratory and digestive system. However, due to the history of persistent headache and sudden sensorineural hearing loss, it was decided to hospitalize him to expand studies.
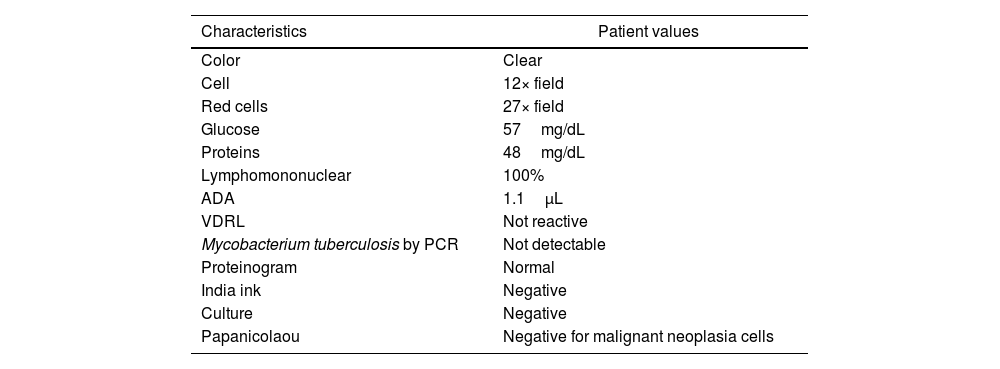
The patient's peripheral white blood cell count was 9650cellsmm3 (72.2% neutrophils, 15.9% lymphocytes, 7.5% eosinophils), and his erythrocyte sedimentation rate was 102mm/h. Serum tests such as glucose, urea, creatinine, thyroxine, TSH, PSA, folic acid, transferrin, B12 vitamin were normal. Infectious diseases panel causing chronic meningitis was requested giving negative results (HIV, HTLV-1, C hepatitis, syphilis). CSF uiexhibited a mild lymphocytosis and slight increase in protein levels without glucose level disturbances (Table 1).
Characteristics of cerebrospinal fluid.
| Characteristics | Patient values |
|---|---|
| Color | Clear |
| Cell | 12× field |
| Red cells | 27× field |
| Glucose | 57mg/dL |
| Proteins | 48mg/dL |
| Lymphomononuclear | 100% |
| ADA | 1.1μL |
| VDRL | Not reactive |
| Mycobacterium tuberculosis by PCR | Not detectable |
| Proteinogram | Normal |
| India ink | Negative |
| Culture | Negative |
| Papanicolaou | Negative for malignant neoplasia cells |
ADA: Adenosine deaminase; VDRL: Venereal Disease Research Laboratory.
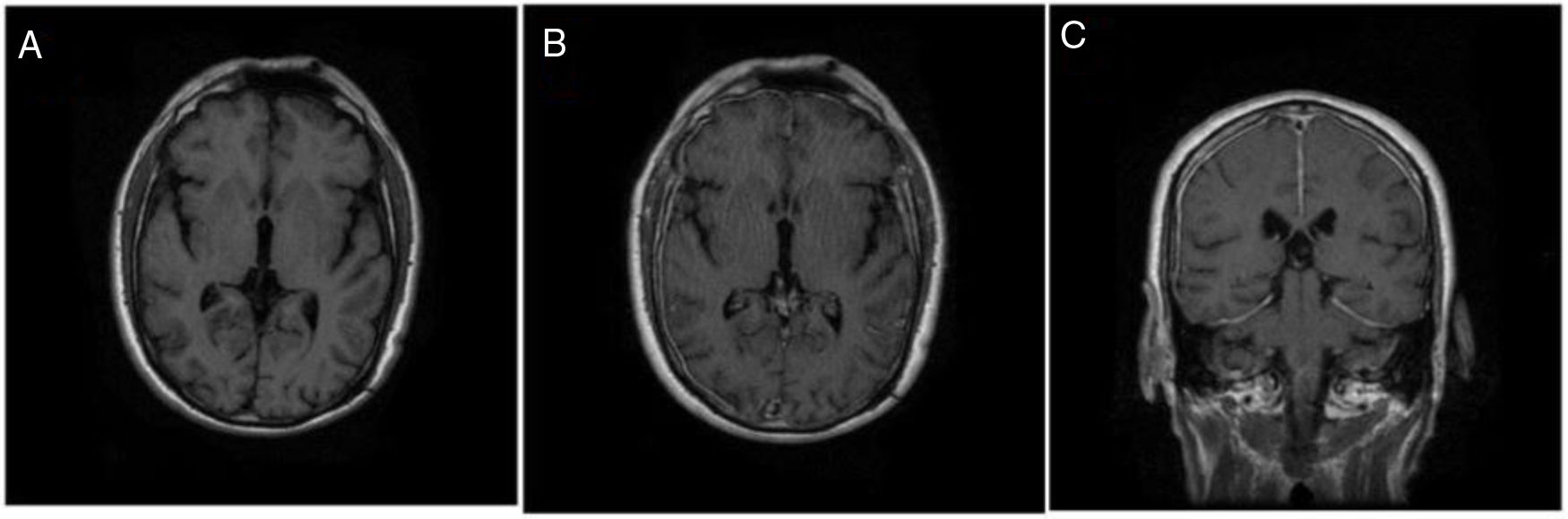
Chest X-ray was normal. MR scan of brain showed multiple subcortical frontal and parietal T1-hypointense, FLAIR-hyperintense. In the Contrast-enhanced MRI, the meninges were with a diffuse thickening involving the tentorium and posterior fossa (Fig. 1C).
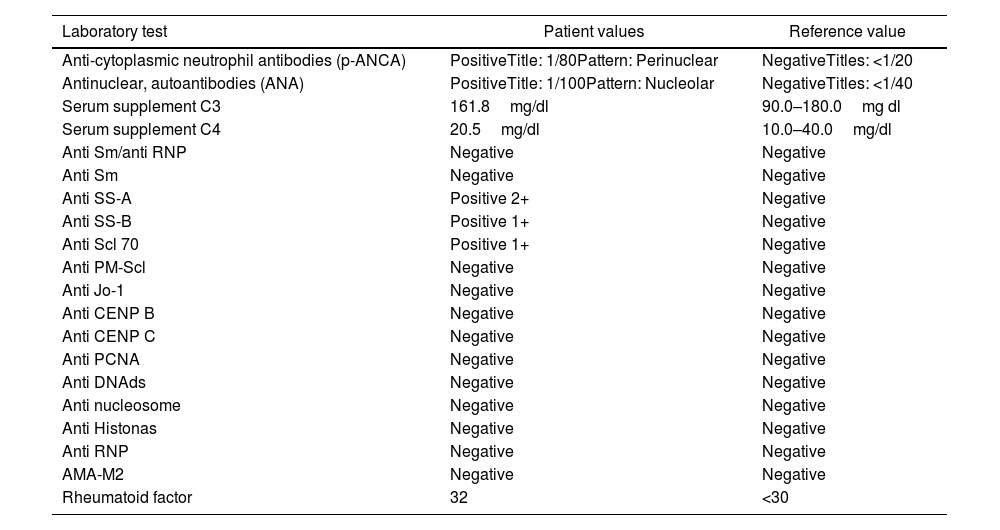
During hospitalization, the patient presented a xerostomia, so the immunological profile was evaluated, which oriented us to Sjögren's syndrome (Table 2). A salivary gland biopsy showed atrophy, fibrosis and periductal lymphocytic foci compatible with lymphocytic sialadenitis. Ophthalmological assessment revealed right eye pseudophakia, scleral inflammation, slight increase in intraocular pressure (23/19mmHg), as well as a pathological Schirmer test (<5mm/5min). Furthermore, auditory evoked potentials confirmed dysfunction bilateral sensorineural hearing pathway. Neuropsychological report showed diffuse alteration fronto-temporal prevalence and multi-domain cognitive impairment in moderate to severe degree.
Immunological profile.
| Laboratory test | Patient values | Reference value |
|---|---|---|
| Anti-cytoplasmic neutrophil antibodies (p-ANCA) | PositiveTitle: 1/80Pattern: Perinuclear | NegativeTitles: <1/20 |
| Antinuclear, autoantibodies (ANA) | PositiveTitle: 1/100Pattern: Nucleolar | NegativeTitles: <1/40 |
| Serum supplement C3 | 161.8mg/dl | 90.0–180.0mg dl |
| Serum supplement C4 | 20.5mg/dl | 10.0–40.0mg/dl |
| Anti Sm/anti RNP | Negative | Negative |
| Anti Sm | Negative | Negative |
| Anti SS-A | Positive 2+ | Negative |
| Anti SS-B | Positive 1+ | Negative |
| Anti Scl 70 | Positive 1+ | Negative |
| Anti PM-Scl | Negative | Negative |
| Anti Jo-1 | Negative | Negative |
| Anti CENP B | Negative | Negative |
| Anti CENP C | Negative | Negative |
| Anti PCNA | Negative | Negative |
| Anti DNAds | Negative | Negative |
| Anti nucleosome | Negative | Negative |
| Anti Histonas | Negative | Negative |
| Anti RNP | Negative | Negative |
| AMA-M2 | Negative | Negative |
| Rheumatoid factor | 32 | <30 |
A leptomeninges and dura mater biopsy showed a minimal chronic inflammatory infiltrate, dense fibro-connective tissue with lymphoid follicles foci and some vessels with reparative fibrosis no granulomas.
Treatment was started with methylprednisolone (1g/day for five days), followed by maintenance therapy with prednisone 20mg/day. Headache, nausea, dizziness, and retroocular pain improved quickly after treatment. CSF cellularity and proteins return to normal levels with acute immunotherapy. Seizures were controlled with valproic acid and no new episodes of seizures have been reported during last three years of follow-up.
DiscussionSjogren's syndrome is a chronic systemic autoimmune disorder that affects the exocrine organs characterized by focal lymphocytic infiltration and destruction of these glands. The manifestations in the CNS are nonspecific such as dizziness, hemiparesis, seizure episode with loss of consciousness, persistent headache, etc. as well as alterations of the SNP retro-ocular pain, sub-febrile episodes, constitutional symptoms, sudden alterations of the cranial nerves, etc. Due to lymphocytic infiltration in the meninges and dorsal root ganglia without any vasculitic process.6,7 There are other processes, with the same target and similar symptoms, such as rheumatology (giant cell arteritis, neurosarcoidosis,8 Behcet,9 and exceptionally association of hypertrophic pachymeningitis with IGg410); oncological11 (dural carcinomatosis, lymphoma); and CNS infections12 (tuberculosis, syphilis, and fungi). Therefore, keep them in mind to raise issues during patient examination.
After a careful study, multiple glandular involvement, brain MRI findings, and CSF features revealed a chronic meningitis a manifestation of an underlying autoimmune disease. Five of the six criteria proposed by the American-European Consensus Group13 were met for the diagnosis of Sjögren's syndrome: oral signs and symptoms; positivity of the Schirmer test; histopathological findings of the salivary glands; and, anti-SS-A and SS-B positive auto-antibodies. There was no suspicion of another autoimmune disease, so it was classified as Primary Sjögren's Syndrome (pSS).
Furthermore, both ANA and ANCA were positive. ANA may be present in 64% of patients with pSS.14 Despite the presence of ANCA-p, no granulomas were evident on biopsy of the leptomeninge, dura, or salivary gland. However, in view of the possibility of latent vasculitis, controls were carried out to especially evaluate renal function every six months.
CNS involvement in pSS is variable, with frequencies ranging from 8.5 to 67%. Disparity in diagnostic criteria for neurological damage and lack of agreement on white matter injuries are responsible of this wide range.3 Few cases regarding chronic meningeal involvement secondary to pSS as well as clinical manifestations have been reported. Gerraty RP et al. reported a fatal case of chronic aseptic meningitis of two years of evolution concordant with our clinical findings.15 Contrary to the cases reported by Kazuyuki Ishida et al.16 and Rosario Ross et al.17 about aseptic meningitis and pSS, our patient had a less florid symptomatology. This is the first case with a neuropsychological examination; however, multiple factors may have been involved in moderate cognitive decline such as comorbidities. MRI shows “Eifel Tower sign” (Fig. 1).18 Sjögren's syndrome is a rare cause of SPH. Yonekawa et al. reported only two cases of pSS in 159 Japanese patients with SPH, no detailed description of the symptoms, diagnosis and evolution.19
A clinical score proposed by Gopal et al.18 evaluated the improvement of clinical symptoms. In a score of over 12 points, he observed a decrease in the score from six to two points after rescue immunotherapy. However, during the three-year follow-up, bilateral hearing loss and cognitive impairment remained stable, affecting the patient's quality of life. Although the inflammatory process in the dura is stopped with immunomodulatory therapy, fibrosis is barely recoverable, which explains the persistence of neurological injury. Furthermore, in a compilation of three case series,18 the most frequently symptom described was headache like in our case.
In our hospital we have several medical specialties, this allows us to focus on rare diseases from different points of view, therefore, we encourage multidisciplinary management; On the other hand, the main limitation of this case is the lack of IGg4, despite the fact that simultaneous IgG4 with ANCA is rare.20
In conclusion, this rare case of chronic meningitis associated with hypertrophic pachymeningitis represents an example of central nervous system involvement in pSS. Nonspecific neurological manifestations such as headache, fever, or neuropsychiatric symptoms as possible manifestations of this syndrome even in elderly patients should be considered.
- •
It is essential to identify a guiding health problem; for example, the headache. Suspect of a secondary cause if we observe warning signs of headache.
- •
Chronic meningitis is a rare manifestation of Sjögren's syndrome.
- •
Neurological involvement of Sjögren's syndrome may have favorable outcomes with prompt diagnosis and corticotherapy; however, sequelae such as permanent bilateral hearing loss and cognitive impairment may remain.
JVC, AHR, RM and AT: manuscript preparation and review. CAD, KPB, RRS, NM: manuscript review.
Patient consent for publicationThe patient gave his informed consent before publication.
Ethics approvalThis study was approved by the Ethics Committee at Hospital Nacional Daniel Alcides Carrión.
Data sharing statementRequests for additional details regarding the case may be made by contacting RM (roberto.molina.ndg@gmail.com).
FundingThe authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors
Conflict of interestThe authors declare that there is no conflict of interest.
We would like to acknowledge and thank the patient and her family.