A case report is presented of a 50-year-old woman who was seen in Accident and Emergency because of pain in the lumbar area. She was subsequently diagnosed with septic arthritis of the left hip due to being Neisseria gonorrhoeae positive for beta-lactamase. She responded to treatment with ceftriaxone, but later required a total hip replacement.
Presentamos el caso de una mujer de 50años, sin antecedentes de importancia, a quien se le diagnosticó inicialmente lumbago e infección de vías urinarias. Por persistencia del dolor y limitación de la movilidad en la cadera izquierda se inicia el estudio de artritis séptica, que fue provocada por Neisseria gonorrhoeae betalactamasa positiva, sensible a tratamiento con ceftriaxona, con posterior deterioro articular, el cual requirió reemplazo total de cadera.
Septic arthritis (SA) is associated with hematogenous dissemination mainly caused by gram-positive cocci (43%) given their ability to interact with extracellular matrix proteins.1–3 Early and rapid destruction of the cartilage and synovial membrane is seen due to increased joint pressure caused causing ischemia and a direct damage to the cartilage by toxins and proteases (e.g. metalloproteinases).3,4 We present a case of a woman without any relevant pathological background and an unusual initial clinical presentation with an unsatisfactory progression.
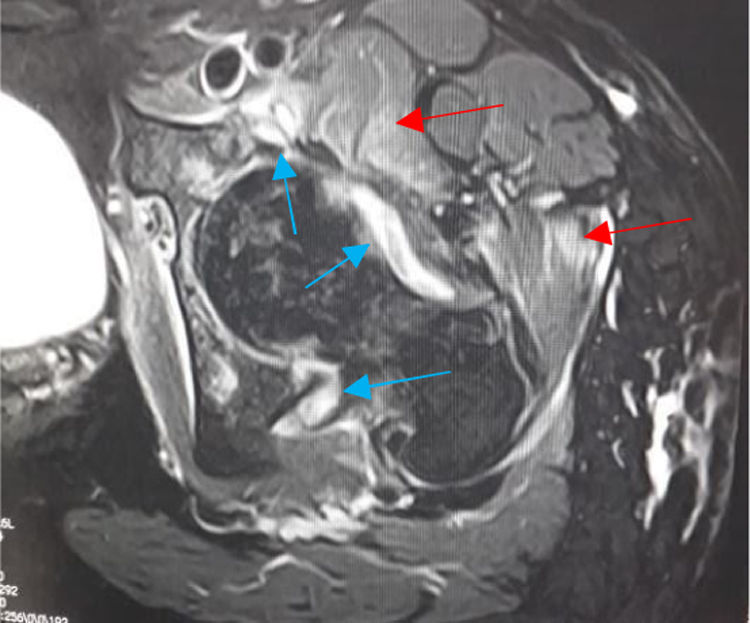
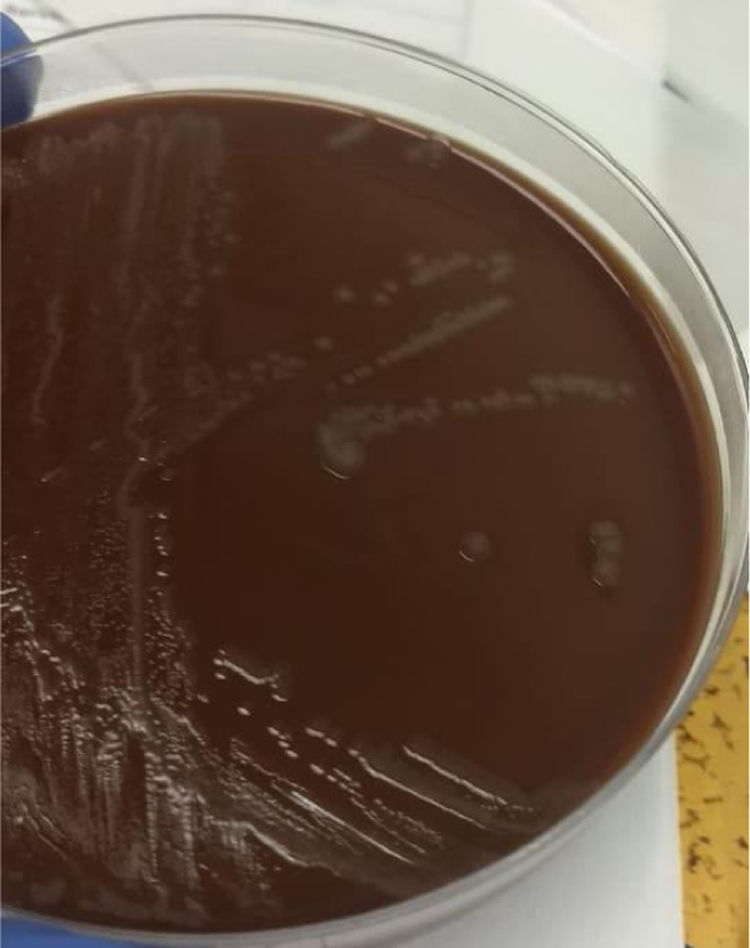
Case reportA 50-year-old female patient, without any relevant medical history, assisted to an emergency room (ER) because a 6-day clinical picture consisting of sudden-onset stabbing pain in the lumbar and left gluteal area. Nonrelevant finding at the physical examination was referred into the medical record and was discharged with an upper urinary tract infection diagnosis. She came to our ER facilities 72h later with low back pain exacerbation and significant limitation of the gait. At the physical exam, no fever, pain in the right iliac fossa during superficial and deep palpation, no signs of cellulitis around the gluteal and inguinal area, limitation in 70° for flexion and 30° for abduction of the left hip. We requested a magnetic resonance which showed abductor muscles myositis and increased intra-articular coxofemoral fluid (Fig. 1). A CT-guided arthrocentesis was performed reporting 2cc of purulent fluid. Orthopedics performed a synovectomy with chondroplasty through arthroscopy finding fibrinopurulent membranes, synovitis, chondral damage with generalized fibrillation, and severe chondromalacia. At 30h synovial fluid culture and blood cultures evidenced growth of Neisseria gonorrhoeae (Table 1, Fig. 2). Screening for sexual transmitted disease (STD) was negative. A single dose of macrolide and 3 weeks of ceftriaxone were given. Five months later patient was proposed a hip replacement due to a secondary severe arthrosis and instability of the joint.
Left hip synovial fluid antibiogram.
| Neisseria gonorrhoeae | ||
|---|---|---|
| Antibiotic | Sensitivity | Minimum inhibitory concentration (MIC) mg/L |
| Cefuroxime | Sensible | ≤0.125 |
| Cefoxitin | Sensible | ≤0.125 |
| Cefepime | Sensible | ≤0.125 |
| Ciprofloxacin | Medium/intermediate | 0.05 |
| Tetracycline | Resistant | >1 |
Note: Betalactamase positive.
N. gonorrhoeae, a gram-negative diplococcus, is rare in SA (≤1%), and probably underdiagnosed, but the most common cause in sexually active young patients, being more prevalent in women (2/3).2,5 Incidence ranges from 1 to 10 cases per 100,000 inhabitants and its prevalence of 0.5–1%.3,4,6,7 In Colombia there is no data related to its incidence nor prevalence. In 22% of patients none risk factor is known (e.g. pregnancy).3 Usually affects large joints, but it can manifest with migratory polyarthralgias or polyarthritis (60%), tenosynovitis (66%), fever and skin lesions (42%).3,4,8 Urinary symptoms occur in 21% of cases.8 Early evaluation of acute monoarthritis is useful for limiting several infectious and early mechanical complications because of its physiopathology as previously explained1–3; monoarthritis should be considered infectious until proven otherwise.1,3–8
Laboratory findings have low sensitivity and specificity (gram staining's sensibility of 25–50% and cultures of 50%).5,6,8 Arthrocentesis should always be made if liquid is observed on images and the liquid should always be cultured in an anaerobic and aerobic media, with a positive gram staining up to 25% being lower in cases of N. gonorrhoeae.3,6,7 Acute phase reactants are helpless given their low specificity (e.g. crystal-associated arthropathy, etc.). In sexually active young people cultures (urethra, rectum, oropharynx, cervical) should be considered to confirm the diagnosis; blood cultures should be taken in every patient with arthritis since up to 33% of cases are associated with bacteremia.9
Ceftriaxone during 2–3 weeks associated with a macrolide is the main treatment. The higher incidence of this pathology may be the result of an increase in a high-risk sexual behavior as well an increased rate of resistance to fluoroquinolones and azithromycin.1–4,10 In our country, in 57% of cases Neisseria is resistant to either penicillins, tetracycline or ciprofloxacin.11 Invasive joint decompression is always indicated if the hip is involved, in peripheric compromise (e.g. knee) not responding to antibiotics within a week or with compromised adjacent tissues.9
This case allows us to reflect the need for a robust clinical history including risk factors for STD when a non-clear clinical picture is present, which could accelerate the diagnosis and treatment avoiding further and invasive procedures. Never underestimate the possibility of an articular infection even if urinary sepsis is more common in the primary care, so to be more careful while doing the physical exam. Finally, remembering the importance of the physiopathology explaining earlier systemic complications, the presence of extra-articular compromise as well as rare complications such as psoas muscle involvement.
Ethical considerationsInformed consent was requested, although it is a risk-free study. At the same time, the images shown in the article are not capable of achieving the identification of the patient, in accordance with the regulations proposed by other international journals.
Conflict of interestsThe authors declare that they have no conflict of interest.