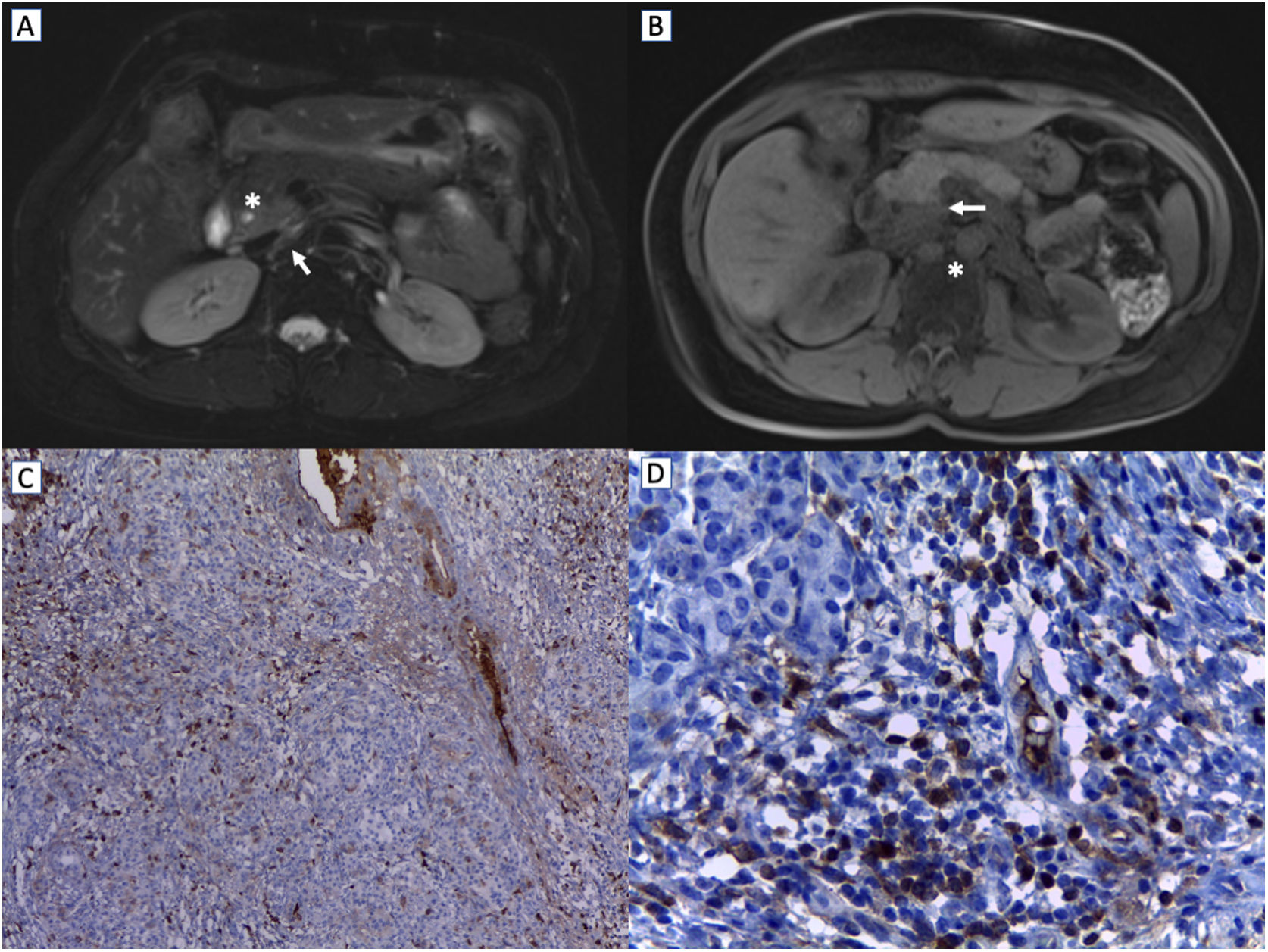
A 54-year-old woman was presented to our institution for an elective Whipple procedure due to a history of chronic jaundice and a hyperintensity in the pancreatic uncinate process on magnetic resonance imaging (Fig. 1) congruent with a mass on endoscopic retrograde cholangiopancreatography. Surgical description reported sclerosed gallbladder, lithiasis, mucosal edema, and a mass of 2cm×2cm in the pancreas head. There were no immediate complications in cholecystectomy and proximal pancreaticoduodenectomy. Later she presented fever secondary to small collections around the surgical area as an infective source. Therefore, she had percutaneous drainage and an antibiotic scheme.
MRI imaging: (A) Axial fat-suppressed (FS) T2-weighting image shows an area of a slight hyperintensity in the pancreatic uncinate process (white arrow), with an infiltrative pattern respecting the pancreatic margins and a patent pancreatic conduit (white asterisk). (B) Axial FS T1-weighting image shows a hypointensity in the pancreatic uncinate process, with a well-perfect delimitation of the rest of the tissue (white arrow). Besides, some peripancreatic and portacaval lymphadenopathy are observed (white asterisk) (C). In immunohistochemical stains, ≥100cells were positive for IgG, and (D) ≥40cells were positive for IgG4 per high power field.
The surgical specimen's biopsy showed lymphoplasmacytic inflammatory infiltrate around the pancreatic and common bile ducts. Storiform fibrosis surrounded the pancreatic duct. It also evidenced chronic pancreatitis changes with lymphocytes and plasma cells destroying pancreatic acini with a proliferation of ducts. Initial laboratories evidenced normal eosinophils count (50cells/mm3), IgE (17.1UI/ml) and IgG4 levels (0.222g/L). On a rheumatologist visit, the patient had stable vital signs on physical examination, no jaundice, a healthy surgical wound, and drains with scant bile. Anti-nuclear antibody, extractable nuclear antigen antibodies, levels of complement, and serum protein electrophoresis were normal. Finally, immunohistochemical staining showed periductal verticillated reticular weft. Positive IgG4+/IgG+stained cells ratio was greater than 40% (Fig. 1). Under the diagnosis of IgG4-related autoimmune pancreatitis, she started prednisolone 40mg/d and azathioprine 50mg/d. Once the infection was solved, she was discharged. On follow-up, the patient continued asymptomatic with no adverse events related to medication.
DiscussionThe pancreatic ductal adenocarcinoma is the first diagnosis to be ruled out due in the pancreatic mass approach due to its low 5-year survival rate (even in localized disease). These three inflammatory conditions are the principal differential diagnosis: chronic formative pancreatitis of mass, focal autoimmune pancreatitis (AIP), and paraduodenal pancreatitis.1 In the case of AIP, 41% of patients present with a focal mass typically located in the pancreatic head. Some findings on magnetic resonance imaging and endoscopic retrograde cholangiopancreatography could discard malignancy, such as the speckled enhancement pattern in the pancreatic phase, irregular narrowing due to infiltration (“penetrating duct” sign), duct narrowing with a greater length at 3cm, dilation of the main pancreatic duct less than 4mm, multiple duct stenoses, delayed homogeneous enhancement, low apparent diffusion coefficient, and hypointense capsule-shaped rim.2
In 2019 multiple organ involvement in IgG4-related disease (IgG4-RD) was classified into four groups to facilitate the diagnosis (pancreato-hepato-biliary disease; retroperitoneal fibrosis, and/or aortitis; head and neck-limited disease; classic Mikulicz syndrome with systemic involvement). From those, pancreato-hepato-biliary condition was the most frequent in 31% of patients.3 Type 2 autoimmune pancreatitis related to IgG4 positive plasma cells was described for the first time in 2003;4 unlike type 2 autoimmune pancreatitis, it predominates in men older than 50 years, its initial manifestation is jaundice (>60%), usually involves other organs, and has a higher relapse rate after steroid therapy (40%).5
The hallmarks findings in histology are lymphoplasmacytic sclerosing pancreatitis, storiform fibrosis, infiltration of IgG4+plasma cells, obliterating phlebitis, and no granulocytic epithelial lesions. Extrapancreatic manifestations include lacrimal gland enlargement, retroperitoneal fibrosis. Biliary system involvement like sclerosing cholangitis and autoimmune cholangitis (77%) are frequent.5 In conclusion, normal IgG4 serum levels did not exclude the disease because of its low sensitivity. The diagnosis must be confirmed with the tissue histology, in which the main criteria is an IgG4+/IgG+plasma cell ratio greater than 40%.6 Initial treatment includes high oral glucocorticoids and the addition of other immunosuppressants (azathioprine, mycophenolate mofetil, methotrexate, leflunomide, tacrolimus, cyclophosphamide among others) according to the patient relapse prognostic factor.7
AuthorshipAll authors had access to the data and a role in writing this manuscript.
FundingNone.
Conflicts of interestNone.