Systemic lupus erythematosus (SLE) can affect the nervous system and present a variety of neurological and psychiatric syndromes but the prevalence of neuropsychiatric manifestations in Colombia is unknown.
MethodsCross-sectional study. Patients were assessed by the department of rheumatology between 2010 and 2013 and included randomly chosen subjects over 18 years of age. Prevalence of neurological manifestations was calculated using a confidence interval of 95%. SLE disease activity index was used as baseline to compare statistically with activity, neurological manifestations and fatality. Mann–Whitney U test was used for quantitative variables, while chi-square test was used for qualitative variables.
Results306 subjects initially entered into the study, 274 were analyzed, 89.1% were women with a median age of 43 years (interquartile range: 23). Prevalence of neuropsychiatric manifestations was 26.2% (95% CI: 21.2–31%). The most common symptoms were headache (13.1%; 95% CI: 9.1–17.2%), cerebrovascular disease (8%; 95% CI: 5.1–11.3%), acute confusional state (6.6%; 95% CI: 4–9.1%), seizure disorders (4.7%; 95% CI: 2.6–7.3%), and aseptic meningitis (2.2%; 95% CI: 0.7–4%); autonomic neuropathy, polyneuropathy, and myelopathy each occurred at 0.7% (95% CI: 0–1.8%). Patients with neuropsychiatric manifestations had severe disease activity (45.8%) and (31.9%) had moderate disease activity.
ConclusionsIn hospitalized patients diagnosed with SLE, NPS manifestations can occur in up to 26% of cases, the most frequent being headache, cerebrovascular disease, acute confusional state, seizures, and aseptic meningitis and the most frequent treatment being systemic steroids. Prospective studies are required to determine their prognostic implications in this group of patients.
El lupus eritematoso sistémico (LES) puede afectar el sistema nervioso con una amplia variedad de síndromes psiquiátricos y neurológicos. La prevalencia de manifestaciones neuropsiquiátricas en Colombia es desconocida.
MétodosEstudio de cohorte transversal. A partir de la revisión del sistema de información del hospital se obtuvieron datos de los pacientes con diagnóstico de LES, mayores de 18años, que fueron valorados por reumatología entre 2010 y 2013. Se utilizó un muestreo aleatorio del listado de sujetos con diagnóstico de lupus en el hospital, se calculó la prevalencia de manifestaciones neurológicas con IC 95%, se realizaron cruces exploratorios entre la actividad de la enfermedad por SLEDAI y las manifestaciones neurológicas, y desenlace de fallecimiento.
ResultadosDe 306 sujetos ingresados al estudio se llevaron al análisis final 274 individuos, de los cuales el 89,1% fueron mujeres; la mediana de edad fue de 43años (RIQ: 23); la prevalencia de manifestaciones neuropsiquiátricas fue del 26,2% (IC 95%: 21,2-31). Los síntomas neurológicos en orden descendente incluyen cefalea (13,1%; IC 95%: 9,1-17,2), enfermedad cerebrovascular (8%; IC 95%: 5,1-11,3), estado confusional agudo (6,6%; IC 95%: 4-9,1), trastornos convulsivos (4,7%; IC 95%: 2,6-7,3), meningitis aséptica (2,2%; IC 95%: 0,7-4), neuropatía autonómica, polineuropatía y mielopatía (presentes en el 0,7%; IC 95%: 0-1,8). Dentro de la población con manifestaciones neuropsiquiátricas se encontró que el 45,8% tenía actividad severa de la enfermedad y el 31,9% actividad moderada.
ConclusionesEn pacientes hospitalizados con diagnóstico de LES las manifestaciones neuropsiquiátricas pueden ocurrir hasta en el 26% de los casos; las más frecuentes son cefalea, enfermedad cerebrovascular, estado confusional agudo, convulsiones y meningitis aséptica, y el tratamiento más frecuente son los esteroides sistémicos. Se requieren estudios prospectivos para determinar sus implicaciones pronósticas en este grupo de pacientes.
Systemic lupus erythematosus (SLE) can affect the nervous system and present a variety of neurological and psychiatric syndromes. All of these effects fall under the general term of Neurolupus.1–3
There is no gold standard test for the specific diagnosis of neuropsychiatric SLE (NPSLE). Generally, it is necessary to evaluate the clinical manifestations. This is accomplished by referring to the standards established by the American College of Rheumatology (ACR), which in 1999 prepared a list of 19 neuropsychiatric syndromes seen in SLE. Of these, 12 relate to the central nervous system (CNS), including aseptic meningitis, cerebrovascular disease, demyelinating disease, headache, movement disorder, myelopathy, seizures, acute confusional state, anxiety disorder, cognitive dysfunction, mood disorder, and psychosis.3,4
Since there is no gold standard test and due to the broad variability in clinical manifestations, estimations of prevalence are widely variable between populations. In 2011, Unterman et al. conducted a meta-analysis of papers published from 1999 to 2008, where they applied the 1999 ACR case definitions to populations in the Americas, Africa, Asia, and Europe. The final analysis included 5057 patients that had already been diagnosed with SLE, and found a 56.3% prevalence of NPSLE (95% CI: 42.5–74.7%).5 Estimations of prevalence can vary within a specific continent; for example, Sanna et al. reported a prevalence of 57% in the United Kingdom,6 whereas Ainiala et al. reported a prevalence of 91.3% in Finland.7
Indeed, different estimations can be observed not just between different countries on the same continent, but within the same country. In Beijing, Zhou et al. reported a prevalence of 12.2%,8 while in Egypt, Abdel-Nasser et al. reported a value of 81%.9 In Latin America, prevalence has been reported as 26% in Brazil by Schenatto et al.,10 and up to 94.7% in Mexico by Sibbitt et al.11 Notably, another study in Brazil, from Appenzeller et al. in 2005, reported a prevalence of 65%.12 All data were from populations admitted to hospitals.
The following is a summary of the most common neuropsychiatric syndromes, described by the American College of Rheumatology which are still valid and are applicable4:
Headache 28.3% (18.2–44.1%)
Mood disorders 20.7% (11.5–37.4%)
Cognitive dysfunction 19.7% (10.7–36%)
Seizures 9.9% (4.8–20.5%)
Cerebrovascular disease 8.0% (4.5–14.3%)5
Since prevalence in Colombia is unknown, the objective of this study is to determine the prevalence and neuropsychiatric manifestations of NPSLE in a cohort of Colombian patients hospitalized due to SLE.
Materials and methodsA cross-sectional study of patients admitted to the San Rafael Clinic University Hospital between 2010 and 2013 was performed. Medical histories were reviewed with the objective of determining the prevalence of neuropsychiatric manifestations in patients with SLE. NP syndromes were defined using the American College of Rheumatology (ACR) nomenclature and case definitions.4 Demographic variables (age, sex), pharmacological treatment, disease activity and mortality were included in the analysis. Patients who were 18 years and older and who had a SLE diagnosis consistent with the SLICC 2012 guidelines13 were included, but only if their medical histories were complete with respect to the studied variables and if they did not have any other concomitant autoimmune disease.
The required sample size was estimated using the program EPIDAT 4.0. Considering a total population of 5000 subjects with a prevalence of 25%, confidence level of 95%, and precision of 10%, a minimum requirement of 274 subjects was identified. The obtained data was transcribed to an Excel spreadsheet (Microsoft Office 2016). Afterwards, the data were input to the licensed statistics program, SPSS version 20. The quantitative variables were processed to yield medians and interquartile ranges (IQRs), given that they did not present a normal distribution. Meanwhile, the qualitative variables were summarized as frequencies and percentages. Furthermore, the outcome variables, such as the prevalence of neuropsychiatric manifestations, were calculated as proportions with accompanying confidence intervals. Finally, the variables of disease activity, pharmacological treatment, and mortality were statistically compared to the neuropsychiatric outcome variables to determine any significant relations. The Mann–Whitney U test was used for the quantitative variables, while the chi-square test was used for the qualitative variables.
This study was evaluated and approved by the research ethics committee of the San Rafael Clinic University Hospital of Bogotá, ensuring that the identity and information of the subjects were confidential.
ResultsA random representative sample of 306 patients with a diagnosis of SLE was selected. 32 patients were excluded because the medical records were incomplete.
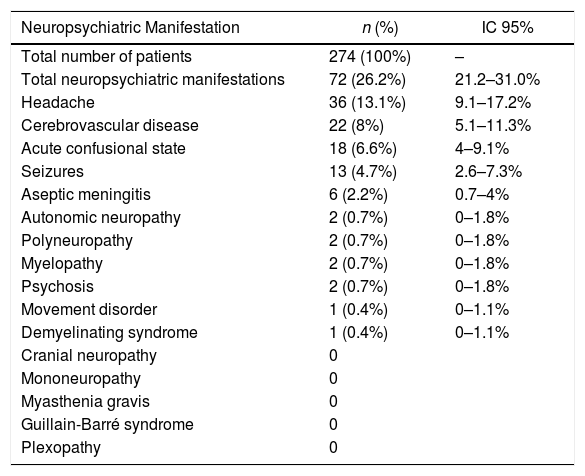
Of these 274 subjects, the median age was 43 years (IQR: 23) and 89.1% were women. The prevalence of neuropsychiatric manifestations was 26.2% (95% CI: 21.2–31%). The manifestations that were found are described in Table 1; the most common were headache (13.1%; 95% CI: 9.1–17.2%) and cerebrovascular disease (8%; 95% CI: 5.1–11.3%). No cases of cranial neuropathy, mononeuropathy, myasthenia gravis, Guillain-Barré syndrome, or plexopathy were observed. Taking into account the descriptive nature of the study it was not possible to evaluate mood disorders, anxiety disorders, and cognitive dysfunction.
Frequency of neuropsychiatric manifestations.
| Neuropsychiatric Manifestation | n (%) | IC 95% |
|---|---|---|
| Total number of patients | 274 (100%) | – |
| Total neuropsychiatric manifestations | 72 (26.2%) | 21.2–31.0% |
| Headache | 36 (13.1%) | 9.1–17.2% |
| Cerebrovascular disease | 22 (8%) | 5.1–11.3% |
| Acute confusional state | 18 (6.6%) | 4–9.1% |
| Seizures | 13 (4.7%) | 2.6–7.3% |
| Aseptic meningitis | 6 (2.2%) | 0.7–4% |
| Autonomic neuropathy | 2 (0.7%) | 0–1.8% |
| Polyneuropathy | 2 (0.7%) | 0–1.8% |
| Myelopathy | 2 (0.7%) | 0–1.8% |
| Psychosis | 2 (0.7%) | 0–1.8% |
| Movement disorder | 1 (0.4%) | 0–1.1% |
| Demyelinating syndrome | 1 (0.4%) | 0–1.1% |
| Cranial neuropathy | 0 | |
| Mononeuropathy | 0 | |
| Myasthenia gravis | 0 | |
| Guillain-Barré syndrome | 0 | |
| Plexopathy | 0 |
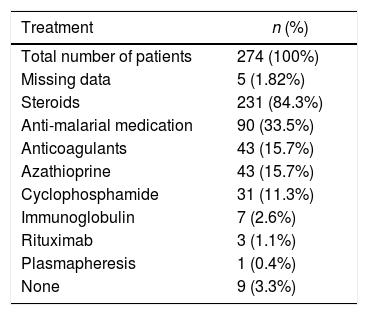
Of the final group of 274 patients, 96.7% received medication while hospitalized; out of that same total, 84.3% received steroids, 33.5% received antimalarial medication, 15.7% received azathioprine, and 15.7% received an anticoagulant (Table 2).
Immunosuppressive treatment received by total cohort.
| Treatment | n (%) |
|---|---|
| Total number of patients | 274 (100%) |
| Missing data | 5 (1.82%) |
| Steroids | 231 (84.3%) |
| Anti-malarial medication | 90 (33.5%) |
| Anticoagulants | 43 (15.7%) |
| Azathioprine | 43 (15.7%) |
| Cyclophosphamide | 31 (11.3%) |
| Immunoglobulin | 7 (2.6%) |
| Rituximab | 3 (1.1%) |
| Plasmapheresis | 1 (0.4%) |
| None | 9 (3.3%) |
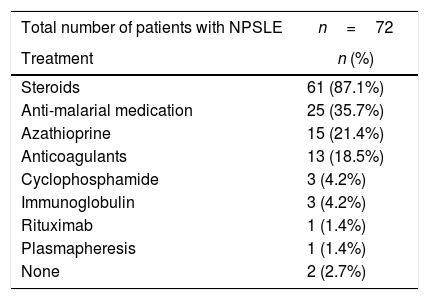
When reframing the data to focus specifically on those patients with NPSLE, 70 patients (97.2%) received treatment. As in the larger group, the most common treatment was with steroids (87.1%) (Table 3).
Immunosuppressive treatment in patients with neuropsychiatric symptoms.
| Total number of patients with NPSLE | n=72 |
|---|---|
| Treatment | n (%) |
| Steroids | 61 (87.1%) |
| Anti-malarial medication | 25 (35.7%) |
| Azathioprine | 15 (21.4%) |
| Anticoagulants | 13 (18.5%) |
| Cyclophosphamide | 3 (4.2%) |
| Immunoglobulin | 3 (4.2%) |
| Rituximab | 1 (1.4%) |
| Plasmapheresis | 1 (1.4%) |
| None | 2 (2.7%) |
NPSLE: Neuropsychiatric Systemic Lupus Erythematosus.
The total studied population exhibited a mortality of 5.8%, of which 50% exhibited moderate disease activity and just 1% had exhibited severe activity.
Among those patients with NPSLE, 45.8% had severe disease activity and 31.9% had moderate disease activity. Meanwhile, when comparing patients grouped according to neuropsychiatric symptoms, more than 50% of the subjects in each group had severe disease activity, with the exception of those with aseptic meningitis, who exhibited a 33% rate of severe disease activity.
DiscussionNeurological and psychiatric symptoms have been reported in 10–89% of patients with SLE.3–5 This study found a prevalence of 26%, which is similar to the findings of Schenatto et al. of 26.4% in a population of 87 subjects in Brazil.10 However, from the same country, there are dissimilar reports of prevalence, like the 65.5% value reported by Appenzeller et al.14 Likewise, Sibbitt et al. reported a value of 94%11 in Mexico in 2002. This discrepancy could be explained by differences in study design or in the recruited populations – for example, some studies employ both pediatric and adult populations.5 In addition, the lack of a gold standard for diagnosing NPSLE4 may have an effect, as well as possible biases that fail to provide a population that is representative of the NPSLE/SLE ratio, such as choosing a population that was admitted to a hospital and thereby obtaining an overestimate. Furthermore, a lack of standardization in neuropsychological tests for cognitive disorders could play a role, as well as the fact that NPSLE and SLE symptoms are not exclusive to these diseases. Finally, differences in severity could have an effect, as well as the different manifestations of the disease in accordance with the studied population.5,15
In our cohort, headache was the most prevalent manifestation (13.1%). The specific prevalence of headache in patients with SLE is unknown; while there are similar results, there are also discrepancies between different studies, such as in that of Unterman et al.5 Again, this could be due to differences in methodology, and especially to the lack of a universal definition of headache.16 There is a recognized kind of headache caused by SLE, named lupus headache; some authors, such as Gladman et al.,17 classify it as a persistent and severe headache, possibly similar to a migraine, that does not respond to analgesics, whereas others describe it as a severe and debilitating headache that does not respond to treatment and that lasts for 3 days.3,4,17,18 However, the above-mentioned definitions may capture other neuropsychiatric SLE events like aseptic meningitis or cerebrovascular events; therefore, given the lack of epidemiological information, defined diagnostic tools, and a verifiable pathogenic mechanism, lupus headache is, as of now, not treated as a distinct condition.
In general, headache in SLE is predominantly observed in women. Its prevalence generally increases the amount of time one has the disease; roughly 18% of the population exhibit this symptom at the onset, and this value reaches 58% after 10 years.19 This might also explain the disparity in the reported data, not to mention the kind of population enrolled in a given study and the prevalence of headache in the study population.5,15,16,19 This study found a prevalence of 13.1% (95% CI: 9.1–17.2%), similar to the value of 12.2% found by Unterman et al. in their meta-analysis.5
SLE might be associated with twice the risk of developing cerebrovascular disease compare with general population20,21; in this cohort, it was the second manifestation in order of frequency, at 8% (95% CI: 5.1–11.3%).
Approximately 10–20% of patients with SLE have seizures.12,21,22 Seizures can be the first manifestation of the disease, or a component of early-onset.22 In this study, seizures occurred with a frequency of 4.7%, similar to the 7% found in the Unterman et al. meta-analysis (p=0.03).5
Plexopathy, Guillain–Barré syndrome, myasthenia gravis, mononeuropathy, and cranial neuropathy are all uncommon5,23–25 and were not observed in this study.
The ACR defines cognitive dysfunction as a significant deficit in any of the following: simple or complex attention, reasoning, executive functioning, memory, visual-spatial processing, language, and psychomotor speed.4 These conditions have a wide range of prevalence across different studies, from 0 to 80% according to Unterman et al., which might be related to the variety of neuropsychological tests used in these trials.5 This factor was not included in this study given the study design and the lack of routine neuropsychological testing during hospitalization. Similarly, Unterman et al. reported in their meta-analysis a lower prevalence in cognitive dysfunction in retrospective studies due to lack of assessment; a value of 6.6% was obtained by averaging the different studies.5 This necessarily underestimates the real prevalence of cognitive dysfunction in SLE patients. As such, this could be a topic of interest for future research, especially since the prevalence of cognitive dysfunction is as high as 60% in studies wherein neuropsychological tests are conducted.
There is not enough evidence regarding which treatment would be the most effective. It seems that cyclophosphamide might be more effective than systemic steroids.26,27 This study did not aim to answer this question, though systemic steroids were the most used.
With the available data, it is not possible to establish through multivariate analysis the relationship between neuropsychiatric manifestations and serum biomarkers like antiphospholipid antibodies, anti-Ro, and anti-La; this is consistent with other studies.28 This might be an important issue for further research, which can aim to establish the role of biomarkers as predisposing factors for the development of neuropsychiatric manifestations.
The weaknesses of this study are its retrospective design, the inability to study causality between the studied variables, the lack of evaluation of cognitive and mood disorders, and the possibility of overestimating the real range of prevalence, given the inpatient population.
ConclusionsThis is the first study regarding the prevalence of neuropsychiatric manifestations in Colombian patients.
In hospitalized patients diagnosed with SLE, NPS manifestations can occur in up to 26% of cases, the most frequent being headache, cerebrovascular disease, acute confusional state, seizures, and aseptic meningitis and the most frequent treatment being systemic steroids. Prospective studies are required to determine their prognostic implications in this group of patients.
FundingNone.
Conflict of interestThe authors declare no conflict of interest.