To determine the abnormal findings in the distal phalanx tuft of the hands (DPTH) in plain radiographs associated with the presence of rheumatoid arthritis (RA) in adults subjects.
MethodsA systematic review was performed following the PRISMA guidelines using databases, such as, Medline, Embase, Bireme, Scielo, and Google Scholar. The main changes in the DPTH included erosion, resorption, sclerosis, and proliferation detected on plain radiographs in adults with RA. Prevalence of radiographic findings was analyzed using a Mantel–Haenszel fixed effects model. Statistical associations (according to study type) were expressed as relative risk (RR) or odds ratio (OR) with their respective confidence intervals (CI) and p values.
ResultsA total of 9 studies were included, in which sclerosis prevalence in the DPTH was 28.3% (95% CI: 0.23–0.34; p<0.001, and I2 value=75%). Resorption prevalence in the DPTH was 1.8% (95% CI: 0.006–0.05; p<0.001, and I2 value=0%). No study reported proliferation or erosions in DPTH.
ConclusionSclerosis in the DPTH is the most frequent radiographic alteration in patients with RA. However, it cannot be considered a pathognomonic finding of that condition, therefore new studies with a more solid methodological structure are needed to clarify this association.
Finally, proliferation, erosion or resorption on the DPTH are not typical radiographic findings in subjects with RA.
Determinar en radiografía simple los hallazgos anormales del penacho de la falange distal de los dedos de la mano (PFDM) asociados a la artritis reumatoide (AR) en adultos.
MétodosSe desarrolló una revisión sistemática siguiendo los parámetros de las guías PRISMA en las bases de datos: Medline, Embase, Bireme, Scielo, Google Scholar, entre otras, incluyendo como resultados primarios las alteraciones del PFDM (erosiones, resorción, esclerosis y proliferación) detectadas por radiografía simple en adultos con AR. La prevalencia de los hallazgos radiográficos fue sintetizada usando el modelo de efectos fijos de Mantel-Haenszel. Las asociaciones estadísticas (según el tipo de estudio) se expresaron en términos de riesgo relativo (RR) u odds ratio (OR), con sus respectivos intervalos de confianza y valores p.
ResultadosNueve estudios observacionales fueron incluidos; la prevalencia de esclerosis del PFDM fue del 28,3% (IC 95%: 0,23-0,34; p<0,001), y un valor I2=75%. De otro lado, la prevalencia de resorción del PFDM fue del 1,8% (IC 95%: 0,006-0,05; p<0,001), con un I2=0%. Ningún estudio reportó proliferación o erosiones del PFDM.
ConclusionesLa esclerosis del PFDM es la alteración radiográfica más frecuente de esta zona en pacientes con AR, sin embargo, no constituye un hallazgo patognomónico de esta entidad, por tanto, nuevos estudios con mayor solidez metodológica son necesarios para esclarecer esta asociación.
Finalmente, la proliferación, erosiones o resorción del PFDM no son lesiones radiográficas típicas de individuos con AR.
Rheumatoid arthritis (RA) is a symmetrical polyarthritis characterized by synovitis and bone erosions.1 The triggering mechanism of the erosions is not clear; McGonagle et al.2 propose that lesions due to micro-stress of the bone adjacent to the synovio-entheseal complex (SEC) are the most important factor in their development, since in individuals with early RA the erosions in small joints do not have a random distribution but a typical location adjacent to the SEC,2,3 which is formed by the collateral ligaments, adjacent cartilages, bone and synovium.
The erosions and the regular joint space narrowing are the typical imaging alterations that usually appear late in a plain radiograph, for this reason its use is reserved to evaluate the extension of the disease and for the follow-up of the response to treatment.4,5 Other radiographic findings in RA include soft tissue edema, juxta-articular osteopenia, subluxations and the resorption of the distal phalanx tuft of the hands (DPTH).6,7
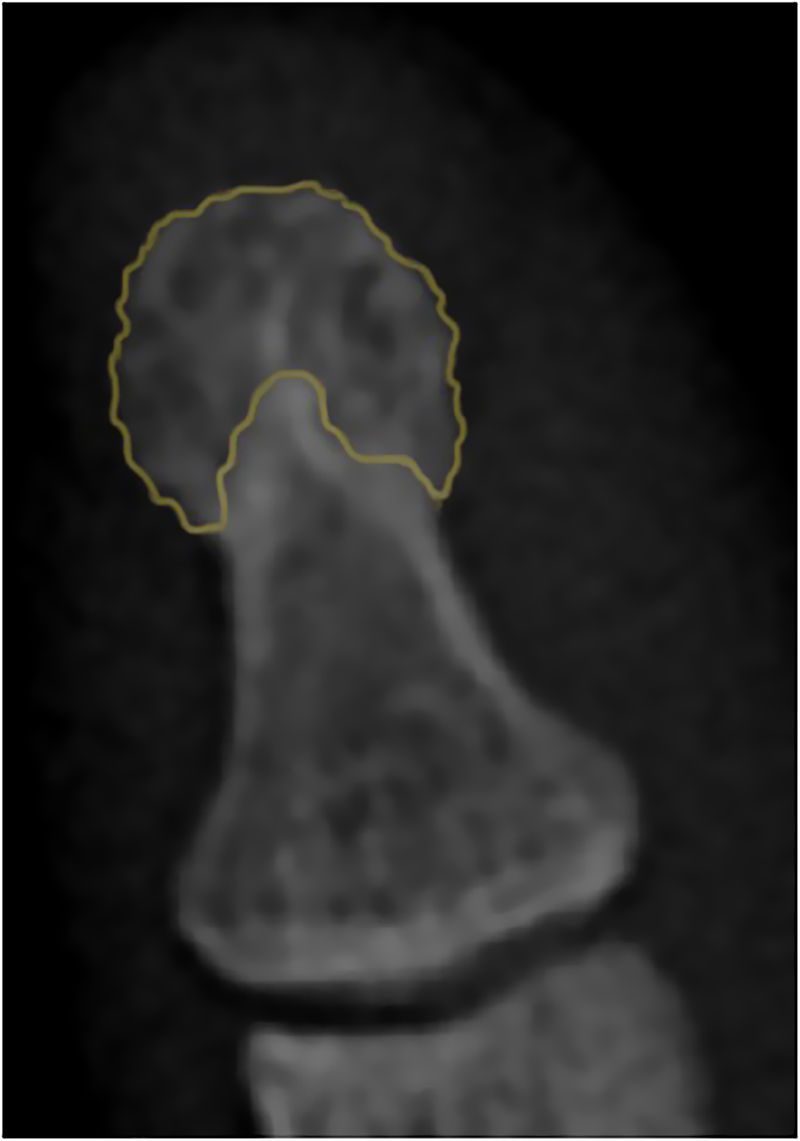
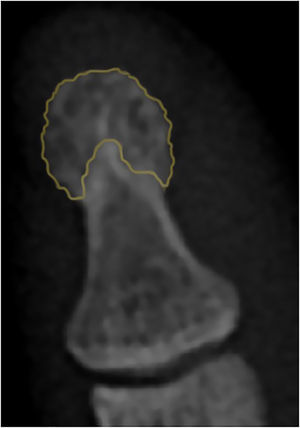
The DPTH does not have a universal radiographic definition, nevertheless, it can be considered as the area of the distal phalanx where the cortical changes from being completely smooth, to acquire a lanceolated appearance8 (Fig. 1). The DPTH is close related with the SEC, therefore, it is a very useful element in the approach of the inflammatory joint diseases (IJD) that can be easily characterized by plain radiography, however, the evidence about the radiographic lesions that compromise it and its performance to establish a differential diagnosis between the IJD is limited.
The purpose of this review is to determine in a plain radiograph the abnormal findings in the DPTH associated to RA in adults.
MethodologyThis review was developed observing the parameters of the PRISMA guidelines9,10 and its protocol was registered in the PROSPERO database of systematic reviews of the University of York, with registration number CRD42015025185, which can be consulted at the following link: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015025185.
Search strategy and eligibilitySearch method for identification of the studiesA systematic search was conducted until December 2015, without language or date restrictions, in the following databases: Medline, Embase, Biblioteca Regional de Medicina (Bireme), Literatura Latinoamericana y del Caribe en Ciencias de la Salud (Lilacs), Scielo, Evidence-Based Medicine Reviews (EBMR), Cochrane Central Register of Controlled Trials, Clinical Trials and Google Scholar.
The search in Medline was carried out through PubMed using the MeSH terms arthritis, rheumatoid, finger phalanges and radiography, linking them with the Boolean connector AND. In order to increase the sensitivity, the respective entry terms for each MeSH term were added to the search, linking them with the Boolean connector OR. Given that DPTH does not have a MeSH equivalent, an additional search was made by replacing the MeSH term finger phalanges with the words: tuft OR plume.
The search strategy used in Medline was adapted for Bireme using the respective DeSC terms, and keywords equivalent to the MeSH-DeSC already described were used for the other databases. The complete search terms can be consulted in the supplementary material of the protocol registered in the PROSPERO platform.
Screening of the studiesOnce the duplicates were extracted, 2 authors (LMC and SVG) who were not experts in radiology or rheumatology evaluated the potential articles. Those documents with at least one of the following words in the title or abstract: erosion, resorption, sclerosis or proliferation (adapting them to the original language of the publication) were included. Any disagreement was resolved by consensus with a third author (YEI).
Inclusion criteria
- 1.
Types of studies: case reports, case–control studies, cross-sectional studies, cohort studies, and randomized or non-randomized assays were included.
- 2.
Population type: adults with diagnosis of RA according to the diagnostic criteria accepted for the date of publication of the study.
- 3.
Intervention: studies evaluating the DPTH in plain radiograph of the hand in one or more projections.
Exclusion criteria
- 1.
Investigations evaluating subjects with simultaneous diagnosis of RA and other musculoskeletal diseases.
The full texts of the screened articles were acquired from electronic databases, searches of printed journals available in public libraries, and in some cases it was necessary to contact the editors or authors of the journals to access the original article.
The verification of the inclusion criteria was developed by 3 authors (ECP, LMC and SVG) evaluating independently the full texts of the publications screened. Any disagreement was resolved through discussion and consensus.
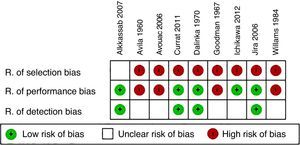
Evaluation of the risk of biasIndividually, 3 authors (LMC, SVG and FSZ) carried out the evaluation of the risk of bias of the studies included in the qualitative synthesis. The studies were initially classified according to the levels of evidence of the Oxford Center for Evidence-based Medicine 2011.11 In addition, the risk of selection bias, detection bias and performance bias of each one of the articles was determined according to questions elaborated by the authors that can be consulted in the protocol registered in the PROSPERO platform.
The risk results for each article were recorded in a table designed for that purpose, using the categories “high risk of bias”, “low risk of bias” or “unclear risk of bias” following the recommendations of the Cochrane Handbook for Systematic Review of Interventions.12 The differences between the evaluations of the authors were resolved by mutual agreement.
Types of measures of resultsDefinition of variablesFor the record of the results, the following radiographic definitions were taken into account:
Acro-osteolysis: destructive process characterized by a decrease in the tuft size, finding that has been classified according to its severity in 4 degrees.13,14
Resorption of the tuft: loss of the lanceolated pattern of the DPTH acquiring a concave morphology, with or without rupture of the cortical.
Sclerosis of the tuft: thickening of the cortical of the DPTH greater than 1mm, with increased bone radiopacity.15
Tuft erosion: focal area of disruption of the cortical of the DPTH.16
Calcinosis of the distal phalanx: calcification of the soft tissues adjacent to the DPTH.14
Bony proliferation of the tuft: cottony or spiculated excrescences adjacent to the bone surface of the DPTH that are usually accompanied by periostitis or thickening of the cortical.17,18
Summary measuresThe quantitative variables were synthesized using the mean and the standard deviation as measures of central tendency and dispersion. The prevalence data were extracted as fraction and equivalent percentage; finally, the statistical associations were expressed in terms of relative risk (RR) or odds ratio (OR) (depending on the type of study), with their respective confidence intervals and p values.
Data collection and analysisFor the studies included in the qualitative synthesis, 2 authors (FSZ and SVG) independently recorded the data in a form specifically designed for this purpose. If there were discrepancies, a third author (YEI) resolved the disagreement.
Statistical analysisUsing the software Review Manager (RevMan) version 5.319 the statistical associations of the dichotomous variables were calculated, expressing them as RR or OR, with their p value and 95% confidence interval for the articles that did not present, in the original text, their findings in these statistical terms. The prevalence of the radiographic findings was synthesized using the Mantel–Haenszel fixed-effects model with the software Comprehensive meta-analysis version 3.0.20 The heterogeneity of the studies was determined with the I2 test, taking as cut-off points >75%, between 51 and 74% and <50% for high, moderate and low heterogeneity, respectively.
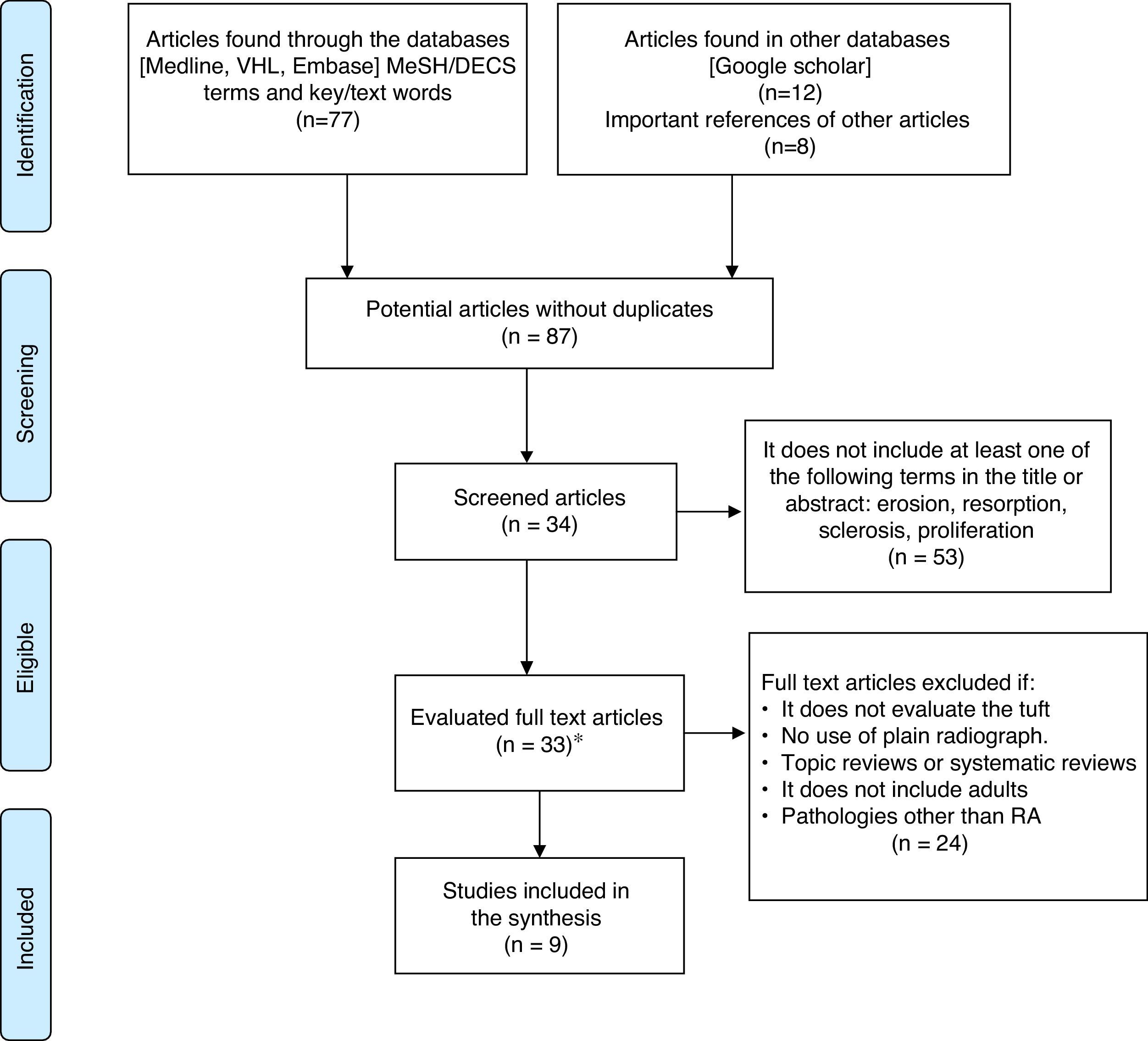
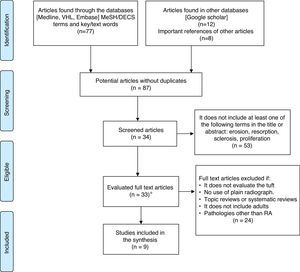
ResultsIn the initial search 25 articles were identified in Medline, 30 in Bireme, 22 in Embase, and 12 in Google Scholar. 26 articles eligible for the review of the full text and 8 important references found in their respective bibliographies were obtained after the extraction of duplicates and screening. It was not possible to acquire one full text due to an inconsistency with the bibliographic citation provided by the database which was not clarified by the editorial committee of the journal.21
4 case reports and 5 case–control studies were included in the qualitative synthesis. The flowchart of the systematic review and the articles included in the analysis is shown in Fig. 2.
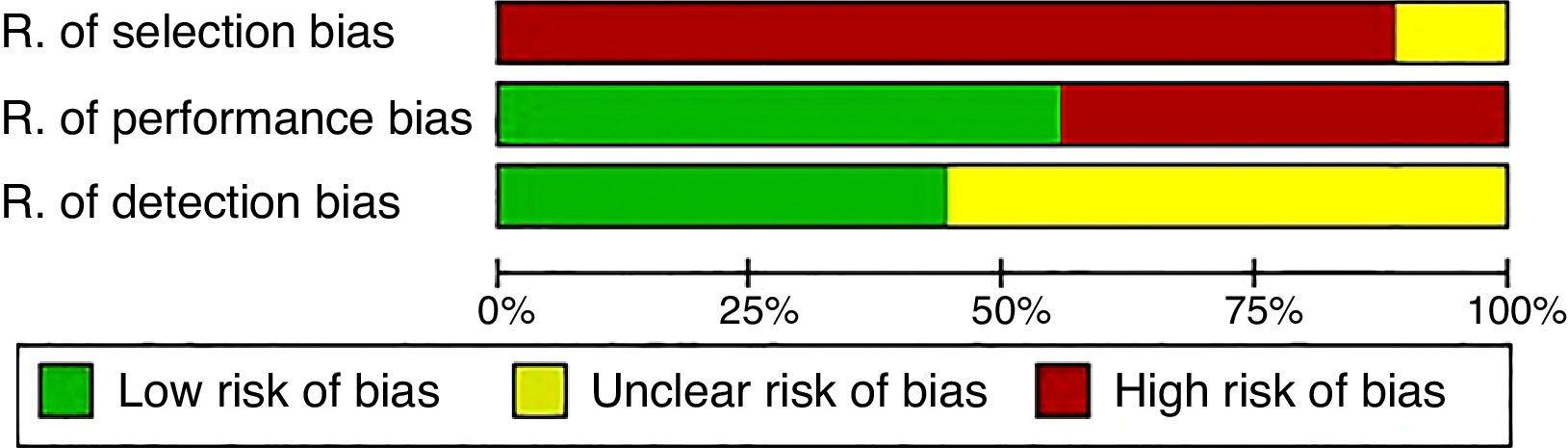
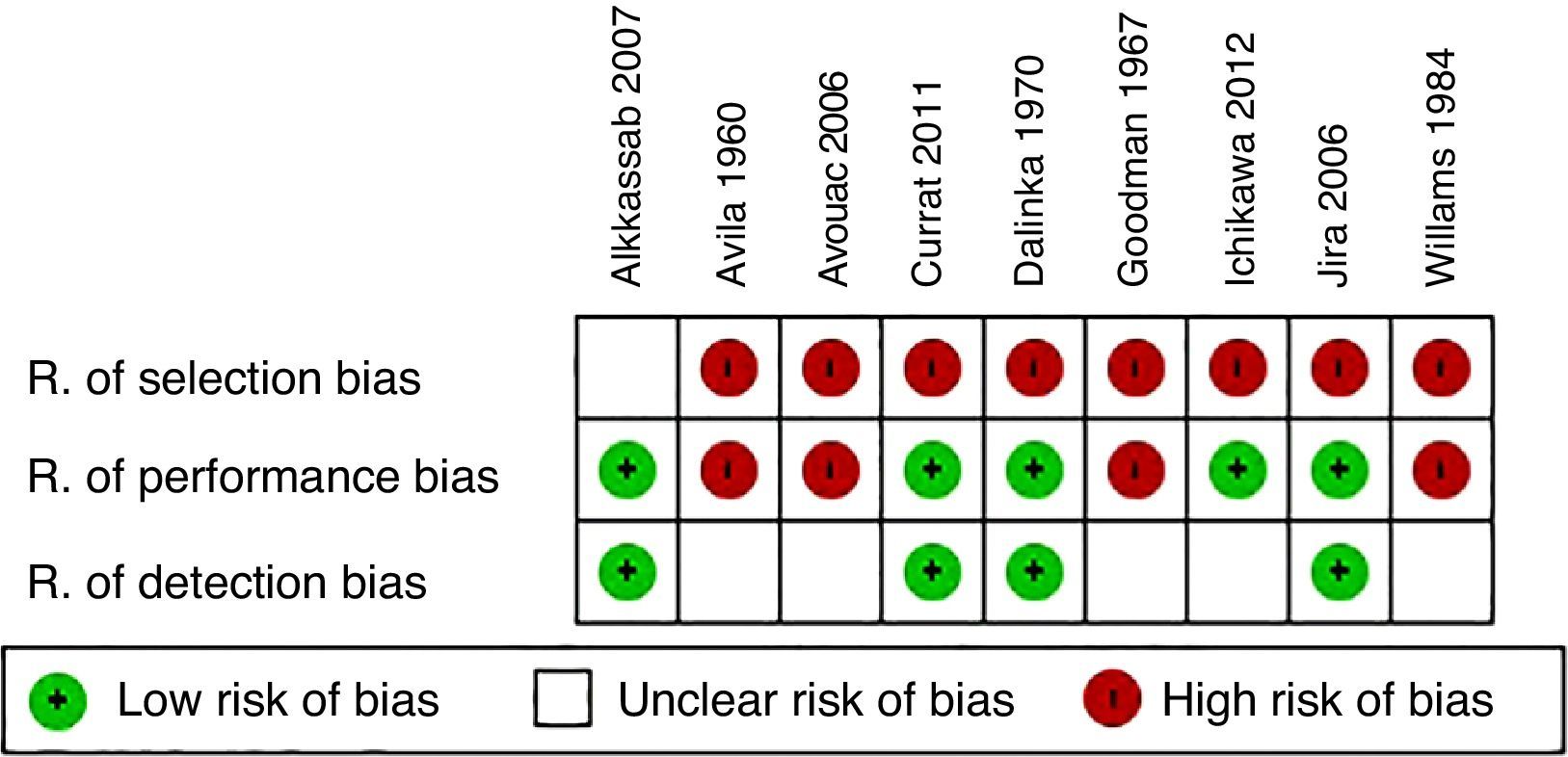
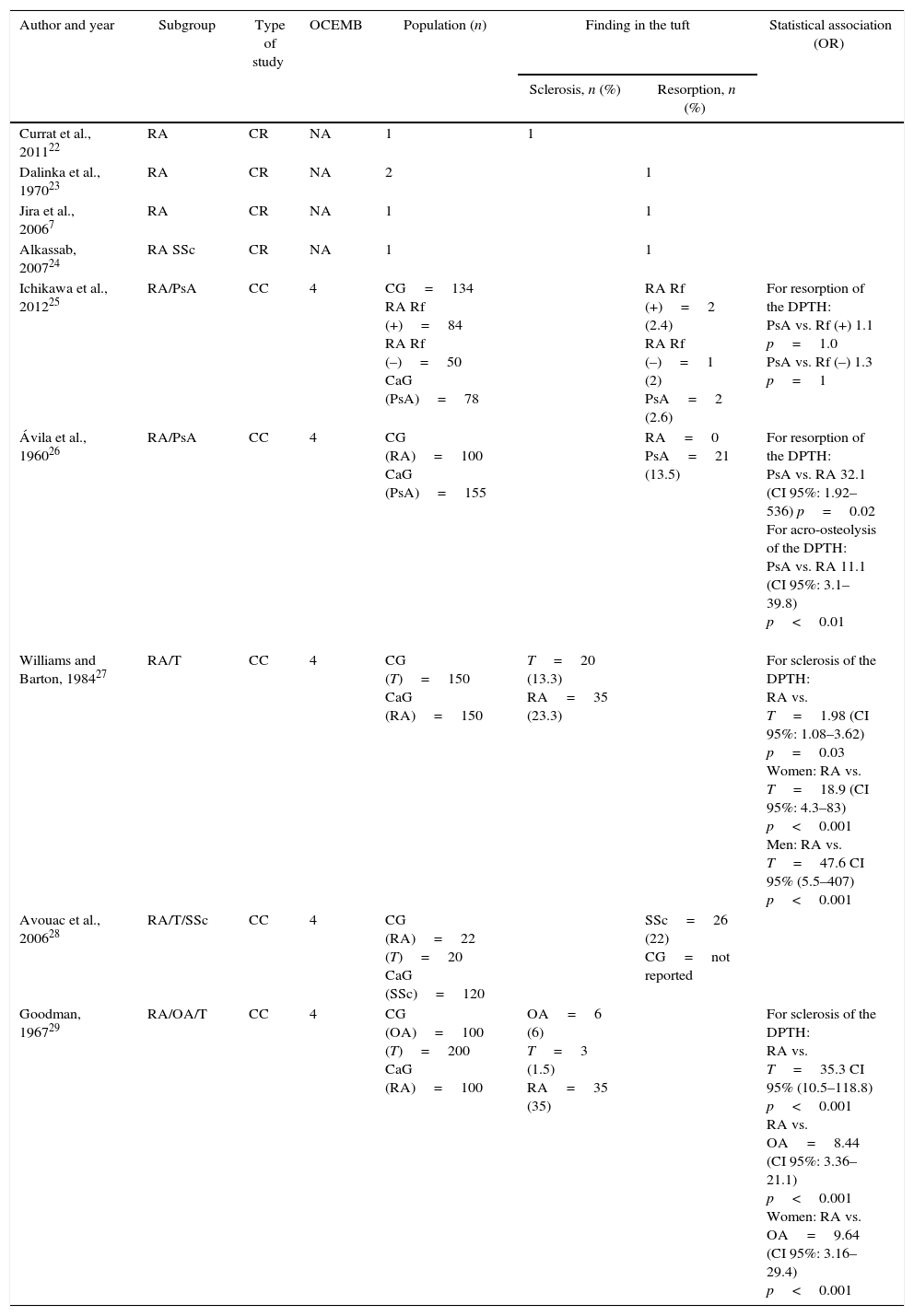
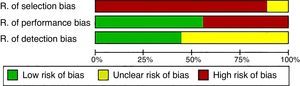
In relation to the risk of selection bias, more than 90% of the investigations were considered as of “high risk” due to the inclusion of individuals with a history of trauma or to the non-specification of the diagnostic criteria used. Four articles were cataloged as of “high risk” of performance bias because they did not specify the time of evolution of the disease or the age of the patients. Five studies were categorized as with an “unclear” detection risk given that the authors did not point out whether the radiological evaluation was blinded or they did not establish the interobserver variability. The results of the evaluation of risk of bias are summarized in Figs. 3 and 4. Regarding the Oxford levels of evidence, 5 texts were located at level 4, and the remaining did not be applied to the classification because they were case reports (Table 1).
Characteristics of the included studies.
| Author and year | Subgroup | Type of study | OCEMB | Population (n) | Finding in the tuft | Statistical association (OR) | |
|---|---|---|---|---|---|---|---|
| Sclerosis, n (%) | Resorption, n (%) | ||||||
| Currat et al., 201122 | RA | CR | NA | 1 | 1 | ||
| Dalinka et al., 197023 | RA | CR | NA | 2 | 1 | ||
| Jira et al., 20067 | RA | CR | NA | 1 | 1 | ||
| Alkassab, 200724 | RA SSc | CR | NA | 1 | 1 | ||
| Ichikawa et al., 201225 | RA/PsA | CC | 4 | CG=134 RA Rf (+)=84 RA Rf (–)=50 CaG (PsA)=78 | RA Rf (+)=2 (2.4) RA Rf (–)=1 (2) PsA=2 (2.6) | For resorption of the DPTH: PsA vs. Rf (+) 1.1 p=1.0 PsA vs. Rf (–) 1.3 p=1 | |
| Ávila et al., 196026 | RA/PsA | CC | 4 | CG (RA)=100 CaG (PsA)=155 | RA=0 PsA=21 (13.5) | For resorption of the DPTH: PsA vs. RA 32.1 (CI 95%: 1.92–536) p=0.02 For acro-osteolysis of the DPTH: PsA vs. RA 11.1 (CI 95%: 3.1–39.8) p<0.01 | |
| Williams and Barton, 198427 | RA/T | CC | 4 | CG (T)=150 CaG (RA)=150 | T=20 (13.3) RA=35 (23.3) | For sclerosis of the DPTH: RA vs. T=1.98 (CI 95%: 1.08–3.62) p=0.03 Women: RA vs. T=18.9 (CI 95%: 4.3–83) p<0.001 Men: RA vs. T=47.6 CI 95% (5.5–407) p<0.001 | |
| Avouac et al., 200628 | RA/T/SSc | CC | 4 | CG (RA)=22 (T)=20 CaG (SSc)=120 | SSc=26 (22) CG=not reported | ||
| Goodman, 196729 | RA/OA/T | CC | 4 | CG (OA)=100 (T)=200 CaG (RA)=100 | OA=6 (6) T=3 (1.5) RA=35 (35) | For sclerosis of the DPTH: RA vs. T=35.3 CI 95% (10.5–118.8) p<0.001 RA vs. OA=8.44 (CI 95%: 3.36–21.1) p<0.001 Women: RA vs. OA=9.64 (CI 95%: 3.16–29.4) p<0.001 | |
PsA: psoriatic arthritis; RA: rheumatoid arthritis; CC: case control; SSc: systemic sclerosis; CG: control group; CaG: case groups; CI: confidence interval; NA: not applicable; OA: osteoarthrosis; OCEMB: levels of evidence of the Oxford Center for Evidence-based Medicine; OR: odds ratio; DPTH: distal phalanx tuft of the hands; CE: case report; Rf: rheumatoid factor; T: trauma; vs.: versus.
The study of Halim et al.15 was not taken into account for the qualitative synthesis, since it only reported the mean of the score of osteosclerosis of the distal phalanx, but not the number or the percentage of subjects with involvement of the DPTH.
None of the studies found proliferation or erosions of the DPTH as radiographic findings in patients with RA. 75% of the case reports informed resorption of the DPTH as a characteristic finding; in contrast, the analytical studies reported as the main finding the sclerosis of the DPTH with a prevalence of 28.3% (CI 95%: 0.23–0.34; p<0.001), with a high heterogeneity I2=75% and a prevalence of resorption of the DPTH of 1.8% (CI 95%: 0.006–0.05; p<0.001), with low heterogeneity I2=0%.
It was not possible to carry out a meta-analysis of the results given the small number of studies found (3 articles compared RA populations vs. trauma and 2 articles RA vs. systemic sclerosis [SSc]).
Two studies reported associations related to sclerosis in the DPTH; the work of Williams and Barton27 evaluated subjects with RA comparing them with individuals with a history of de trauma, finding an OR=1.98 (CI 95%: 1.08–3.62; p=0.03), with statistically significant associations when they were discriminated by gender (Table 1). In similar populations, Goodman29 found an OR=35.3 (CI 95%: 10.5–118.8; p<0.001) in favor of subjects with RA; in this study was also compared the DPTH between individuals with RA and patients with osteoarthrosis (OA) finding for sclerosis in DPTH an OR=8.44 (CI 95%: 3.36–21.1; p<0.001) in the general population, and an OR=9.64 (CI 95%: 3.16–29.4; p<0.001) when only women were included.
The results related to resorption of the DPTH are contradictory; Ichikawa et al.25 compared subjects with RA against individuals with psoriatic arthritis (PsA) without finding a statistically significant association (Table 1); however, Ávila et al.26 studied similar populations and reported, in favor of the subjects with PsA, an OR=32.1 (CI 95%: 1.92–536; p=0.02).
Table 1 summarizes in detail the studies included in the synthesis, the evaluated populations and the reported associations.
DiscussionThis study found that DPTH sclerosis is the only radiographic finding associated with individuals with RA, with a prevalence of 28.3% and a statistically significant OR between 1.98 and 35.3, with a high heterogeneity when compared with controls with a history of trauma. The prevalence of resorption of the DPTH in RA was only 1% and its occurrence is apparently related to other IJD such as SSc.30,31
Halim et al.15 published in 1975 a score for osteosclerosis of the distal phalanx of the hands ranging from 0 to 3 points for each finger, being 3 points the involvement of the entire phalanx including the DPTH. When they added up the scores for each finger, excluding the thumb, they found high values for RA, intermediate for OA and low for subjects without antecedents of IJD, however, up to 50% of the population over 44 years of age without IJD presented this finding.
The study by Halim et al.15 did not discriminate whether the individuals included had a history of hand trauma; this fact could condition a bias of confusion given than in another systematic review, conducted by our group (whose results can be consulted in http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015025185), determined that individuals with history of trauma exhibit more frequent alterations in the DPTH compared with individuals with no antecedents of trauma in hands.
This review has several limitations that restrict the importance of the results found; first, only 9 articles were included, and of these, 44% corresponded to case reports; in addition, the populations evaluated exhibited a great diversity and included subjects with SSc, PsA and trauma.
Only the articles of Williams and Barton27 and of Goodman29 reported sclerosis in the DPTH as the most important radiographic finding; it should be clarified that a cluster analysis according to the age of the subjects included was not performed in none of them, and therefore is not possible to establish the association between these 2 variables; likewise, the time of evolution of the RA was unknown, so it is not possible to conclude if the sclerosis of the DPTH is an early or a late finding.
Another element to take into account was the low methodological quality of the primary studies given by the lack of clarity in the diagnostic criteria used or by the form of selection of the patients, reasons that conditioned the high risk of selection bias found.
ConclusionsSclerosis of the DPTH is the most frequent radiographic alteration of this area in patients with RA; however, it is not a pathognomonic finding of this entity, therefore, new studies with greater methodological solidity are necessary to clarify this association.
Finally, the proliferation, erosions or resorption of the DPTH are not typical radiographic lesions in individuals with RA.
Conflict of interestThe authors declare they do not have any conflict of interest.
Oscar Eduardo Guzmán Mendoza: Assistant researcher, medical student, National University of Colombia.
Member of the research hotbed of the Group of investigation in Radiology and Diagnostic Imaging GRID.
Please cite this article as: Izquierdo YE, Calvo Páramo E, Castañeda LM, Gómez SV, Zambrano FS. Cambios radiográficos del penacho de la falange distal de las manos, en pacientes con artritis reumatoide. Revisión sistemática. Rev Colomb Reumatol. 2017;24:32–39.