Behçet's disease is a low prevalence disorder that is difficult to diagnose. Its forms of presentation are often confused with infectious processes that involve multiple treatments and prolonged hospital stays. This article presents the case of a 30-year-old man who consulted with non-specific symptoms that represented a diagnostic challenge for the medical team.
La enfermedad de Behçet es una patología de baja prevalencia y difícil diagnóstico, sus formas clínicas de presentación suelen confundirse con procesos infecciosos que implican múltiples tratamientos y estancias hospitalarias prolongadas. Este artículo presenta el caso de un hombre de 30 años quien consulta de manera repetitiva con síntomas inespecíficos, lo que representa un reto diagnóstico para el equipo médico.
Behçet's disease is an autoinflammatory and autoimmune pathology difficult to diagnose1,2; its clinical forms of presentation on the skin can be confused with pyogenic infectious processes, which makes its diagnosis difficult and implies prolonged hospital stays with increased healthcare costs.
CaseA 30-year-old patient, with a progressive clinical picture of fever and sweating for 2 months, later with a dry cough, moderate pain in the testicles and lower back. Pyelonephritis was diagnosed in the initial care center by means of ultrasound studies and antibiotic management was started. During hospitalization, the patient presented an acneiform rash on the trunk and lower limbs, accompanied by painful ulcers on the penis, testicles, and mouth. Ten days later, the skin lesions improved and the patient was discharged with antibiotic treatment (dicloxacillin) and outpatient control.
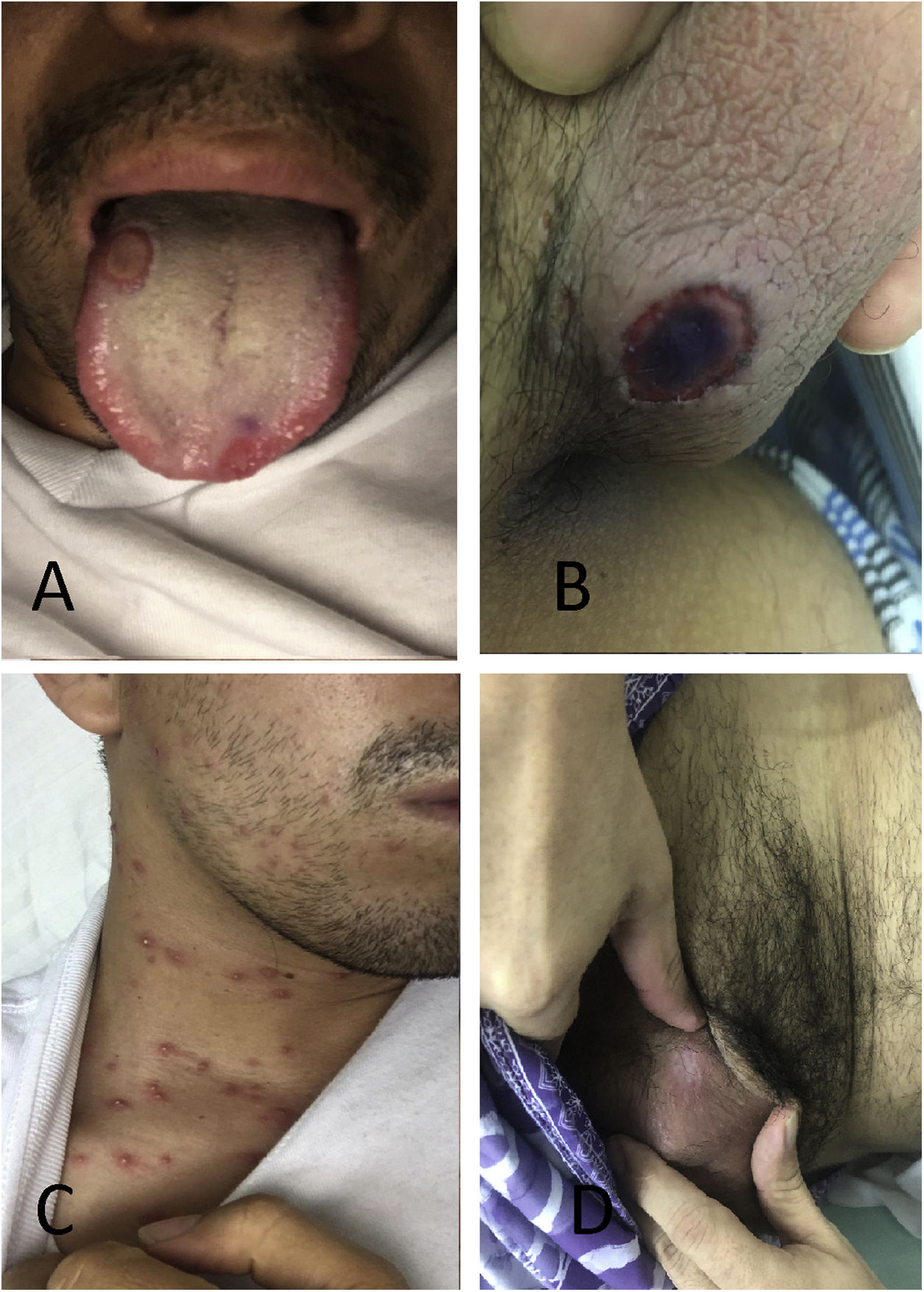
Twenty-two days later, the patient consulted with the same symptoms, nocturnal fever, sweating, and testicular and lumbar pain. He was febrile, and ulcers in the testicles and oral mucosa, with pustular comedo-type lesions in the anterior chest in different stages of vesicular progression were discovered during the physical examination, without joint involvement (see Fig. 1).
Lesions of the patient. A) Surface of the tongue with a rounded well-defined lesion covered by a yellowish pseudomembrane. B) Rounded ulcer with well-defined borders and a necrotic center, at the base of the penis. C) Pustular vesicles with erythematous halo, in the anterior thorax. D) Cicatricial lesion in the testicle after treatment.
Autoimmunity and microbiological studies were reported negative, blood and urine cultures did not isolate any microorganism; however, the acute phase reactants were elevated (see Table 1).
Laboratory studies.
| Test | Result |
|---|---|
| Autoimmunity studies | |
| Complement | Negative |
| Rheumatoid factor | Negative |
| Antinuclear antibodies (ANAS) | Negative |
| Microbiological studies | |
| Blood count | Without alterations |
| Thick blood smear | Negative |
| VDRL | Negative |
| HIV | Negative |
| Hepatotropic viruses | Negative |
| Mycobacterium | Negative |
| Herpes virus | Negative |
| Cytomegalovirus | Negative |
| Epstein-Barr | Negative |
| Blood cultures | Negative |
| Urine culture | Negative |
| Acute phase reactants | |
| CRP | 159.50 mg/dl (0−5 mg/dl) |
| ESR | 111 mL/h (5−20 mL/h) |
| Ferritin | 1920.8 ng/mL (30−400 ng/mL) |
Given the difficulty of the case, the dermatology service was consulted in order to define the diagnosis and management of the patient. Corticosteroids were administered during the hospital-stay and the fever improved 48 h later. The clinic and the subsequent pathology report were compatible with Behçet's disease. The patient was dewormed and treatment with prednisolone, colchicine and azathioprine was started.
DiscussionIn individuals with a genetic predisposition, various exogenous genetic factors can trigger Behçet's disease. Studies demonstrate that the presence of the HLA-B51 allele of chromosome 6p is higher in these patients, while variants of interleukin (IL) 10 and IL-37 have a reduced expression.3 The relationship with infectious agents is based on a cross-reaction by molecular mimicry with the participation of the innate immune system.3,4
Oral ulcers are the first sign of the disease in 80% of cases. These have well-defined borders, with an erythematous halo, are painful, and can leave sequelae such as scars, dysphagia, odynophagia, and dyspnea.5 Genital lesions are another important manifestation of the disease.
Ocular manifestations mainly affect the retina and the uvea in 30–70% of cases and can appear up to 3 years after the onset of symptoms. Only 20% of the cases begin with ocular involvement, which did not occur in our patient. The follow-up of these subjects is very important to avoid sequelae in visual acuity. Neurological involvement occurs in 10% of the patients, especially in men, and can appear up to 5 years after onset, as well as joint manifestations, which can occur in up to 60% of patients, affecting the knees, ankles and wrists.6
Currently, the diagnosis of this disease is clinical, based on the New International Criteria for Behçet's Disease (ICBD). A score higher than 4 is required to confirm the diagnosis. These criteria include skin lesions, oral and genital aphthae, among others. Histopathologic studies are nonspecific but may show perivascular inflammatory infiltrates with associated fibrinoid necrosis.7
The management of the disease varies depending on the compromise of the affected system; colchicine is a first line agent in mucocutaneous involvement. The phosphodiesterase 4 inhibitor, apremilast, and the interleukin-1 receptor antagonist anakinra are effective options for refractory mucocutaneous involvement.8
A case-control study found a significant association between multidimensional fatigue, anxiety, depression, and physical dysfunction; therefore, these symptoms are important to accomplish a diagnostic approach.9
ConclusionIt is essential to identify Behçet's disease in the services, since due to its difficult diagnosis it can be confused with other pathologies of infectious origin, which implies the unnecessary use of multiple treatments and affects the quality of life of patients.
Ethical ConsiderationsFor the study and publication of the case, prior written informed consent was obtained from the patient. The photographs presented here preserve the patient's identity and do not show characters that would facilitate their identification. This is to protect their rights and confidentiality.
FundingThis work has not received specific aids from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestThe authors declare that they have no conflict of interest.
We thank the patient, who allowed us to know his case, review it and learn from it.