Adult onset Still's disease (AOSD) is a systemic inflammatory disorder of unknown etiology. AOSD is generally a mild and self-limiting disease, but it could progress to become chronic. The anemia of chronic diseases may occur in patients with acute or chronic immune activation, and is associated with the production of pro-inflammatory cytokines.
Case reportA 61-year-old woman with several pharyngitis episodes, spiking fever, evanescent salmon-pink skin rash, normocytic normochromic anemia, leucocytosis, thrombocytopenia, polyarthritis, liver dysfunction, marked elevated erythrocyte sedimentation rate and C-reactive protein and, notably high ferritin levels. AOSD was diagnosed after secondary diseases were ruled out. Despite eight month on treatment with high-dose corticosteroids and methotrexate the clinical course the patient worsened, with significant synovitis, joint deformities leading to a worse quality of life and requiring help with activities of daily living. A rapid response to the anti-TNFα golimumab (50mg/month) was observed from the third month of treatment.
ConclusionGolimumab improved anemia, serum C-reactive protein levels, polyarthritis and quality of life in a refractory AOSD.
La enfermedad de Still del adulto (AOSD, por sus siglas en inglés) es un desorden inflamatorio sistémico de etiología desconocida que puede progresar a un curso crónico. La anemia de enfermedades crónicas puede ocurrir en pacientes con alteraciones inmunes agudas o crónicas, y se asocia con la producción de citoquinas proinflamatorias.
Caso clínicoSe presenta el caso de una mujer de 61 años con varios episodios de faringitis, fiebre aguda, lesiones en piel salmón-rosadas evanescentes, anemia normocítica normocrómica, leucocitosis, trombocitopenia, poliartritis, disfunción hepática, aumento de la velocidad de eritrosedimentación y proteína C-reactiva y niveles notablemente altos de ferritina. Se diagnostica como enfermedad de Still del adulto después de descartar enfermedades secundarias. A pesar de los 8 meses de tratamiento con altas dosis de corticosteroides y metotrexato, la paciente empeoró la evolución clínica, con sinovitis importante, deformidades articulares que condujeron a una peor calidad de vida requiriendo ayuda para las actividades de la vida diaria. Luego de recibir golimumab anti-TNFα (50mg/mes), se observó una rápida respuesta a partir del tercer mes de tratamiento.
ConclusiónGolimumab mejoró la anemia, los niveles séricos de proteína C-reactiva, la poliartritis y la calidad de vida en una AOSD refractaria.
Adult onset Still's disease (AOSD) is a systemic inflammatory disorder. The diagnosis needs clinical suspicion and the exclusion of infection, malignancy and systemic disease. The most widely validated criteria are Yamaguchi's criteria. The presence of two or more major criteria has 96.2% sensitivity and 92.1% specificity for AOSD.1 The annual incidence of AOSD is nearly to 0.16–0.4/100.000 adults.2,3
AOSD is generally a mild and self-limiting disease (34%), but it could progress to intermittent course (24%), to a chronic course with relapse (36%) and occasional life-threatening complications in one-third of patients.4 Refractory systemic flares of the disease may potentially cause life-threatening conditions, such as macrophage activation syndrome, hepatic failure, disseminated intravascular coagulation, pericarditis, pleuritis, peritonitis, amyloidosis.5 Anemia could be one of the manifestations in AOSD, which is classified as anemia of chronic disease and it may occur in patients with acute or chronic immune activation associated with the production of proinflammatory cytokines. Chronic inflammation can modify the erythropoiesis, probably mediated by pro-inflammatory cytokines such as interleukin-1 (IL-1), TNFα and interferon-γ.6 It was previously reported the use of biologic agents in refractory AOSD which contributes to improve the course of the disease.7–10
Case reportA previously healthy 61-year-old female patient started with several pharyngitis episodes. The last one was accompanied with spiking fever once a day to 39–40°C, usually in the evening or night, with concomitant salmon-colored rash of the trunk and extremities and severe polyarthritis with impaired activities of daily living. At physical examination the patient had polyarthritis in carpometacarpal, proximal and distal interfalangical joints, elbows, shoulders, hips, knees, ankles and metatarsophalangeal (Fig. 1 left). Hepatomegaly was also detected. Positive laboratory findings: white blood cell count 16.500mm3 (neutrophil 85%), hemoglobin 8.7g/dl, hematocrit 33.3%, platelet count 80000mm3, aspartate aminotransferase 180mU/ml (normal range: <37mU/ml), alanine aminotransferase 250mU/ml (normal range: <65mU/ml) and ferritin levels of 40000ng/ml (normal range: 10–277ng/ml). The serological findings were: CRP 60mg/dl (normal range <5.0), ESR: 120mm 1/hour, rheumatoid factor: negative. Antinuclear antibodies, antideoxyribonucleic acid antibodies, myeloperoxidase antineutrophil cytoplasmic antibodies, proteinase 3 antineutrophil cytoplasmic antibodies, anti-cyclic citrullinated peptide antibodies and extractable nuclear antigens were negative. Serum protein electrophoresis and complement factor 3 (C3), C4 and CH50 were in normal range. Other autoimmune, infectious and neoplastic diseases were excluded. Chest X-ray, electrocardiogram and echocardiogram were normal. Thorax, abdominal and pelvis computed tomography scan were negative for a primary disease. Joint radiographs showed juxta-articular osteopenia. Accordingly, the patient was diagnosed as AOSD.
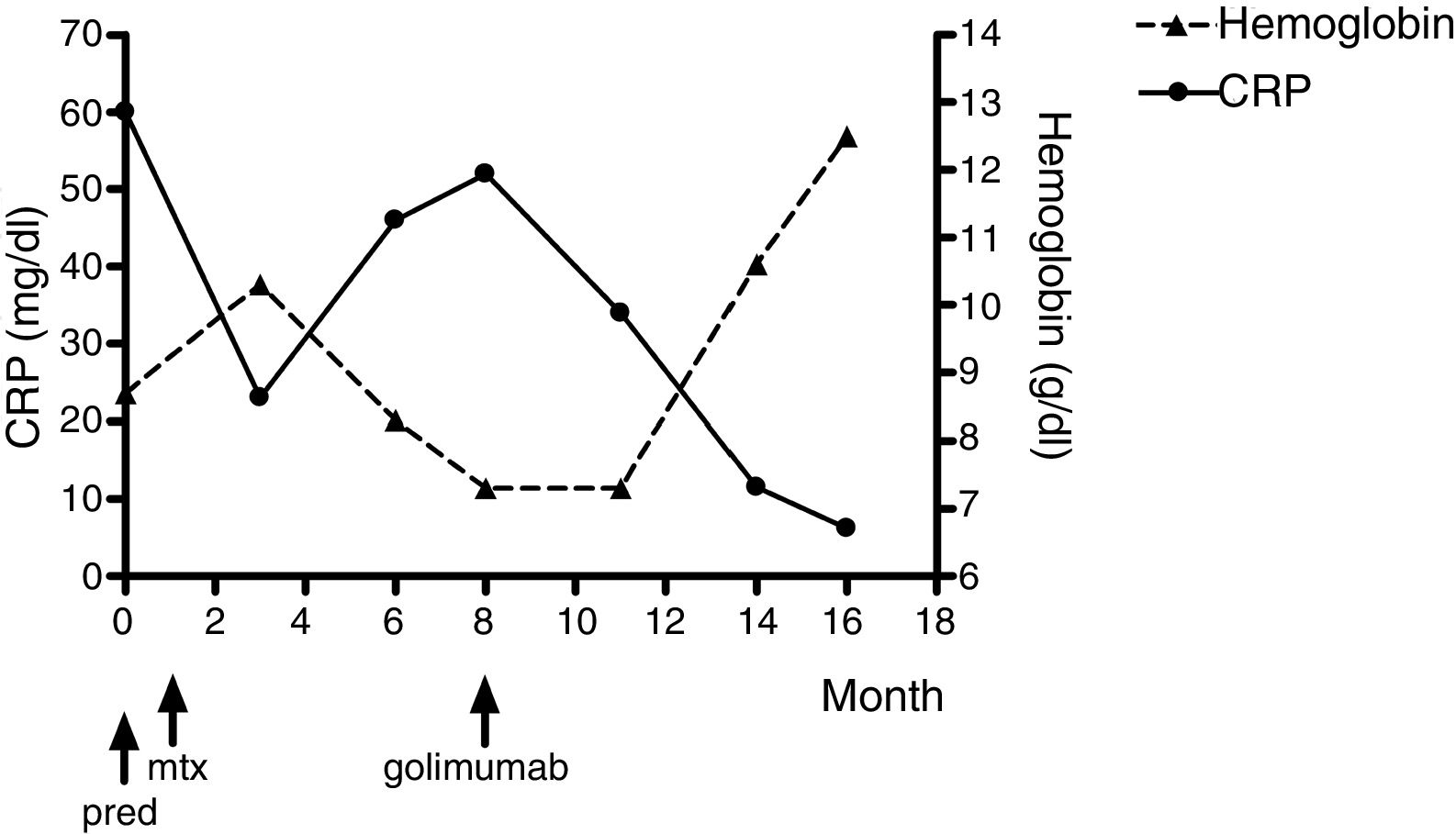
Prednisone 50mg/day improved significantly and rapidly the liver test functions, leucocytosis, thrombocytopenia and arthralgias. Steroid dose was reduced progressively to 20mg/day but disease recurrence occurred. The recurrence was characterized by severe arthritis which needed higher doses of prednisone. The patient also need pain medications at high doses: diclofenac, indomethacin and ibuprofen were indicated when each one failed. Methotrexate was also initiated because the aggressive course of the disease and the high dose of steroid required. Despite treatment with methotrexate 25mg/week and prednisone 30mg/day an improvement was not observed. Persistent anemia, polyarthritis, and fever were observed. The patient could not walk and could not perform activities of daily living. Therefore golimumab 50mg/monthly was indicated. After three month of golimumab treatment an improved in pain, synovitis (Fig. 1 right), anemia and daily activities was observed. The laboratory findings after eight month of golimumab treatment were: white blood cell count 6.000mm3, hemoglobin 12.5g/dl, hematocrit 40%, platelet count 245.000mm3. The liver function tests, serum electrolytes and renal function were in normal range. ESR rate was 10mm/1st hour and CRP was 6.2mg/l. The hemoglobin and CRP changes over time are shown in Fig. 2. Joint radiographs performed at the follow-up evaluation had not join destruction.
Remission has been maintained for 36 months with prednisone 5mg/day, methotrexate 15mg/week and golimumab 50mg/month and pain medication is not required. The patient can do activities of daily living, walk and also ride a bike.
Informed consent was obtained from the patient reported in this article.
DiscussionAOSD is a disease of young adults but can affect patients older than 60 years of age.11 Pathogenesis of AOSD remains partially unknown but a major role has been recently attributed to proinflammatory Th1 cytokines, including TNF-α, IL-1, IL-6 and IL-18.6
AOSD is generally a mild and self-limiting disease but it could progress to a chronic course in 36% of the cases. The elevated ESR and corticosteroids refractoriness were associated with poor prognosis.4
Kim et al.5 studied 54 Korean patients with AOSD. Fourty two percent of these patients were resistant to corticosteroids while methotrexate was the most commonly used disease modifying anti-rheumatic drugs (50%). The corticosteroid requirements were lower in the methotrexate responsive patients. Disease refractory to conventional treatment has led to the use of biologic therapy including anti-TNF-α (etanercept, infliximab and adalimumab), anakinra, tocilizumab, abatacept and rituximab.6–9
This case report had all the Yamaguchi's criteria diagnostic; other inmunologic, infectious and cancer were ruled out. Because of refractory and aggressive joint disease golimumab – a humanized monoclonal anti-TNFα – was indicated as other biological agents were previously reported.
Multiple clinical cases using etanercept have been reported which are summarized by Kiyonaga et al.12 Among them there are three case series with 12, 10 and 4 patients.13–15 Infliximab was used as anti-TNFα in AOSD 14–18 and also in aggressive cases with good response.19,20 The use of adalimumab in AOSD has been reported in two cases: one patient with favorable response21 and another patient without favorable response.22 No data were found about golimumab.
Besides anti-TNF-α agents, other immunosuppressive treatments were also reported. Anakinra also showed good response in case series of AOSD resistant to conventional immunosuppressive treatment.23–30 A multicenter study of 41 patients showed that anakinra is associated with rapid and sustained clinical and laboratory improvement, even in non-responders to other biologic agents, but joint manifestations were more refractory than the systemic manifestations.30
The efficacy of tocilizumab in patients with AOSD with inadequate response to corticosteroids and standard synthetic immunosuppressive drug or anti-TNF-α has been reported. Tocilizumab was associated with a rapid improvement in refractory AOSD but joint manifestations seem to be more refractory than systemic manifestations.31,15,32,33,34,35
Limited data about abatacept and rituximab in refractory AOSD are available. A few patients have been reported. Abatacept was reported in one patient resistant to DMARDs36 and in other one resistant to DMARDs, anti-IL-1 and anti-TNF-α therapies.37 Rituximab has also shown efficacy in AOSD.38,39
Due to severe joint involvement an anti-TNF agent was used. Among them golimumab was selected since it is administered subcutaneously monthly as the patient lived in a small village without possibility of intravenous administration. Also, the patient had severe anemia and golimumab had been shown to improve hemoglobin levels as described below. Anemia of chronic disease may occur in patients with acute or chronic immune activation and is associated with the production of proinflammatory cytokines.5 It has been reported that lower hemoglobin levels were associated with increased disease activity and anemia contributed independently to physical disability in patients with rheumatoid arthritis.40,41 The anemia improvement requires a treatment of the underlying inflammatory cause. Patients under golimumab treatment significantly improved hemoglobin levels. In patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis (n=2303) treated with golimumab hemoglobin levels increase from baseline to week 14, 0.9g/dl in anemic patients and 0.3g/dl in control subjects. This increased was higher when anemia was due to inflammatory cause (1.4g/dl).42
In this case report, during the first three month of golimumab treatment the hemoglobin levels were in a plateau and after that an increase in an average of 0.86g/dl/month was observed (5.2g/dl in five months).
ConclusionGolimumab treatment improved the course of the disease, polyarthritis and quality of live in a refractory AOSD.
Conflict of interestMaría Lorena Brance declare that she has no conflict of interest.