To determine the cardiovascular risk and the prevalence of cardiovascular risk (CVR) factors in patients with rheumatoid arthritis.
Material and methodsObservational, descriptive and cross-sectional study performed in the General Hospital of Ciudad Real from June 2013 to May 2014. A complete laboratory analysis was performed, a clinical profile was prepared, the Systematic COronary Risk Evaluation (SCOREm) was calculated, and the CVR was stratified. Finally, the presence of sub-clinical atherosclerosis was determined by performing a carotid ultrasound.
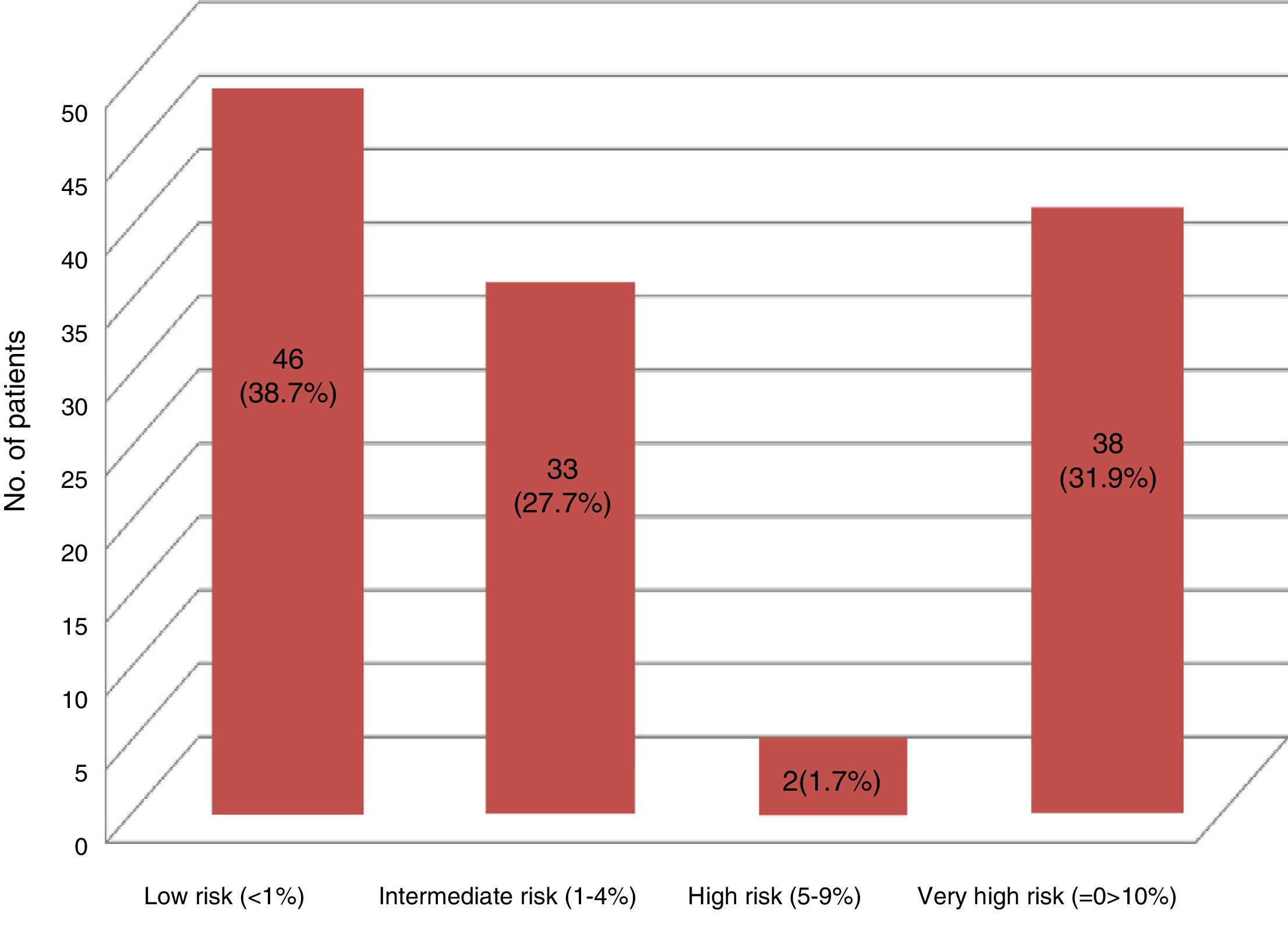
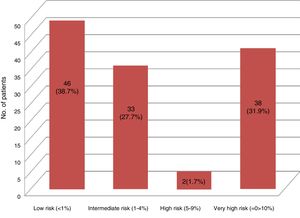
Results119 patients accepted to participate in the study. There was a prevalence of 73.1% of traditional risk factors; 6.72% having had a cardiovascular event at the time of the study, and 22.68% had an underdiagnosis of diabetes mellitus and/or nephropathy. The final distribution of the CVR was: Low risk 46 (38.7%), intermediate risk 33 (27.7%), high risk 2 (1.7%), very high risk 38 (31.9%).
ConclusionsThere is a high prevalence of CVR factors and an elevated risk of underdiagnosis in the rheumatoid arthritis population. Therefore, although rheumatoid arthritis manifests itself more in the joints, it should be considered a systemic disease associated with a higher incidence of cardiovascular events.
Determinar el riesgo cardiovascular y la prevalencia de factores de riesgo cardiovascular (RCV) en los pacientes con artritis reumatoide.
Materiales y métodosEstudio observacional, descriptivo y transversal, realizado en el Hospital General de Ciudad Real, entre junio de 2013 y mayo de 2014. Se realizó una analítica completa, se elaboró un perfil clínico, se calculó el SCOREm y se estratificó el RCV. Finalmente, se determinó la presencia de aterosclerosis subclínica mediante la realización de una ecografía carotídea.
Resultados119 pacientes aceptaron participar en el estudio. Hubo una prevalencia del 73,1% de los factores de riesgo tradicionales, 6,72% había presentado un evento cardiovascular al momento del estudio, 22,68% poseía un infradiagnóstico de diabetes mellitus o nefropatía. La distribución final del RCV fue: riesgo bajo 46 (38,7%), riesgo intermedio 33 (27,7%), riesgo alto 2 (1,7%), riesgo muy alto 38 (31,9%).
ConclusionesExiste una alta prevalencia de factores de RCV y riesgo elevado infradiagnosticado en esta población. Por lo que si bien la artritis reumatoide se manifiesta de forma más aparente a nivel articular, ha de considerarse una enfermedad sistémica asociada a una mayor incidencia de eventos cardiovasculares.
Rheumatoid arthritis (RA) is an inflammatory systemic chronic disease that affects 0.5–1% of the population. It causes a decrease in the life expectancy of the population and has a mortality 1.3 to 3-fold higher than in the general population, standing out the mortality of cardiovascular origin (40–50%).1–3
Numerous studies have revealed the increased risk of acute myocardial infarction (RR: 2.07–3.17) and cerebrovascular accident (RR: 1.48) in patients with RA,4,5 comparable with that described in diabetes mellitus type 2 (OR: 2.7–3.11).6,7
Even though the classical cardiovascular risk (CVR) factors are important in the pathogenesis of atherosclerosis in this population, they could be underdiagnosed and even not fully explain this increase in cardiovascular events.8–10 Being described as nontraditional risk factors the time of evolution, the presence of positive serology (rheumatoid factor, anti-CCP), genetic factors such as the presence of HLA-DRB1*0401 and HLA-DRB1*0404 alleles, markers of chronic inflammation (CRP, ESR, serum amyloid, etc.), disease activity state (DAS28, SDAI, etc.), extra-articular manifestations, chronic treatment with NSAIDs and corticosteroids, etc. For all this reasons, many authors suggest to consider the cardiovascular disease as an extra-articular manifestation of RA.11–15
Because of this, the “European League Against Rheumatism” (EULAR), proposed by consensus for the estimation of the CVR (low <1%, moderate 1–4%, high 5–9% and very high ≥10%) the use of the modified SCORE (SCOREm), which consists in multiplying by a conversion factor of 1.5 the result obtained with the SCORE of the patients who meet 2 of the following 3 criteria: duration of the disease longer than or equal to 10 years, positive rheumatoid factor (RF) or anti-cyclic citrullinated peptide (anti-CCP) and the presence of extra-articular manifestations.16 However, it has been observed how this tool and the factors taken into account underestimate this risk; objectifying up to 12–30% of subclinical atherosclerosis by carotid ultrasound and the development of cardiovascular events in the short-medium term in the patients classified as low/intermediate risk.17–22
Objective. To determine the cardiovascular risk and the prevalence of cardiovascular risk factors in patients with RA.
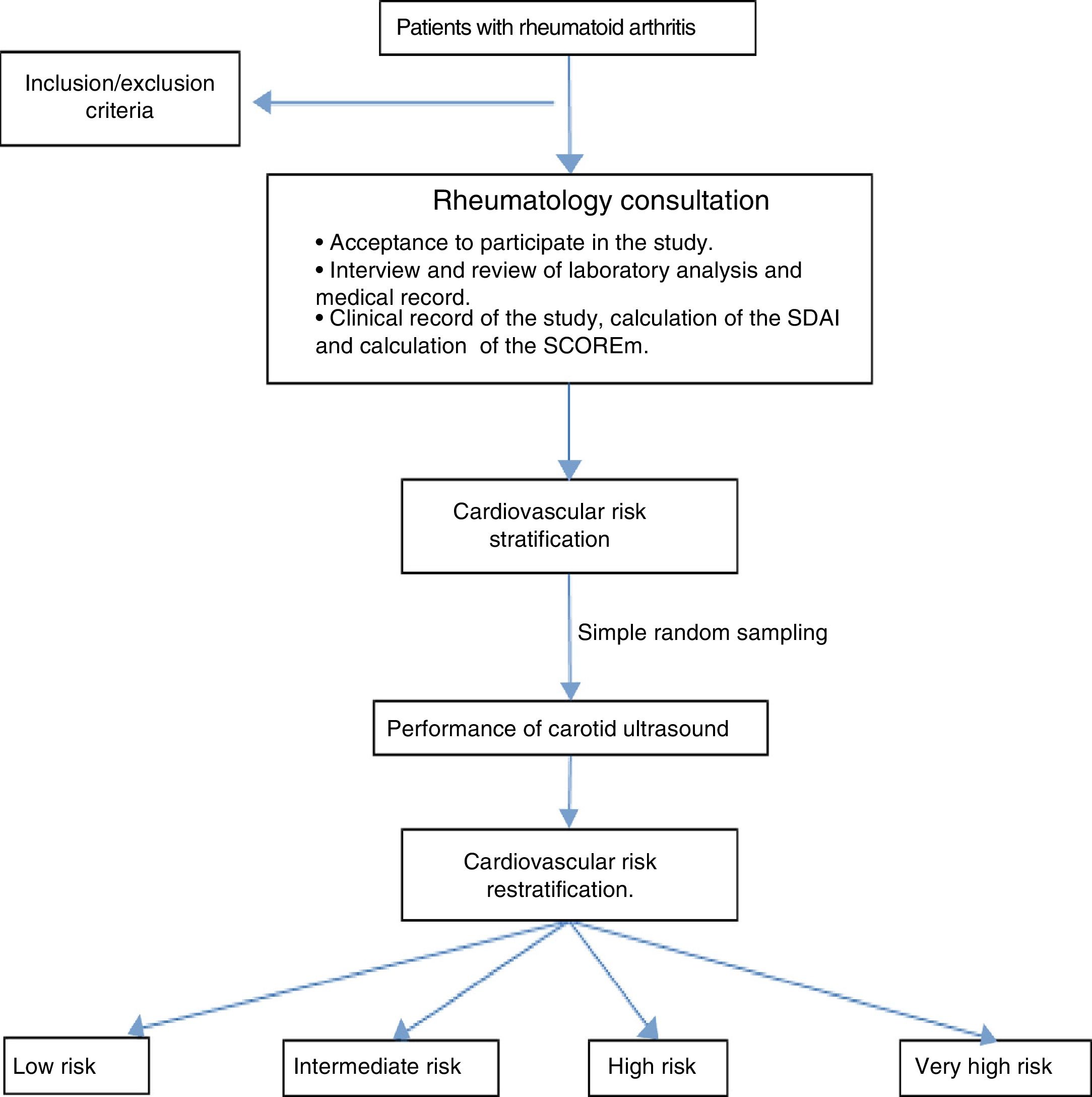
Materials and methodsAn observational, descriptive and cross-sectional study was developed in patients older than 18 years who met the international criteria validated by the ACR/EULAR 201023 who were seen in the outpatient consultation of the General University Hospital of Ciudad Real (HGUCR) from June 2013 to May 2014 and who agreed to participate in the study by signing the informed consent. Overlapping syndromes and those who could not perform the laboratory analysis for the calculation of the SCORE were excluded (Fig. 1). Given the small population, the study was conducted in all patients who agreed to participate therein. The information was obtained through clinical interview in the consultation, the medical history and recent analysis that included serological and activity markers (erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor and anti-citrullinated peptide antibodies) as well as a metabolic study for the assessment of the CVR (basal glycemia, glycated hemoglobin, uric acid, and renal, lipid and thyroid profiles). With the results, a clinical profile was elaborated, the SCOREm (age, gender, blood pressure, total cholesterol/HDL levels, smoking habit and CVR factors of RA) was calculated and the CVR was stratified.
All patients received general recommendations for healthy lifestyles and treatment was started to those with high/very high risk according to their CVR profile, with subsequent follow-up by their primary care physician.
Finally, a simple random sampling (95.5% confidence level and 5% sampling error) was carried out to perform a carotid ultrasound by a radiologist who at all times was unaware of the clinical profile of the patient. A Toshiba Aplio XG ultrasound scanner, model Ssa-790A, linear transducer of 7–10MHz) was used, emphasizing the measurement of the intima-media thickness (IMT), considering as pathological an IMT>0.9mm, the presence of atheromatous plaque, and focal thickening >1.5mm, according to the usual protocol.24–27
The information obtained was entered into a Microsoft Excel database, the evaluated variables were described using measures of frequency and measures of central tendency/dispersion. All the analyses were carried out with a confidence level of 95% using STATA 12.0. The study protocol was approved by the clinical research ethics committee of the HGUCR.
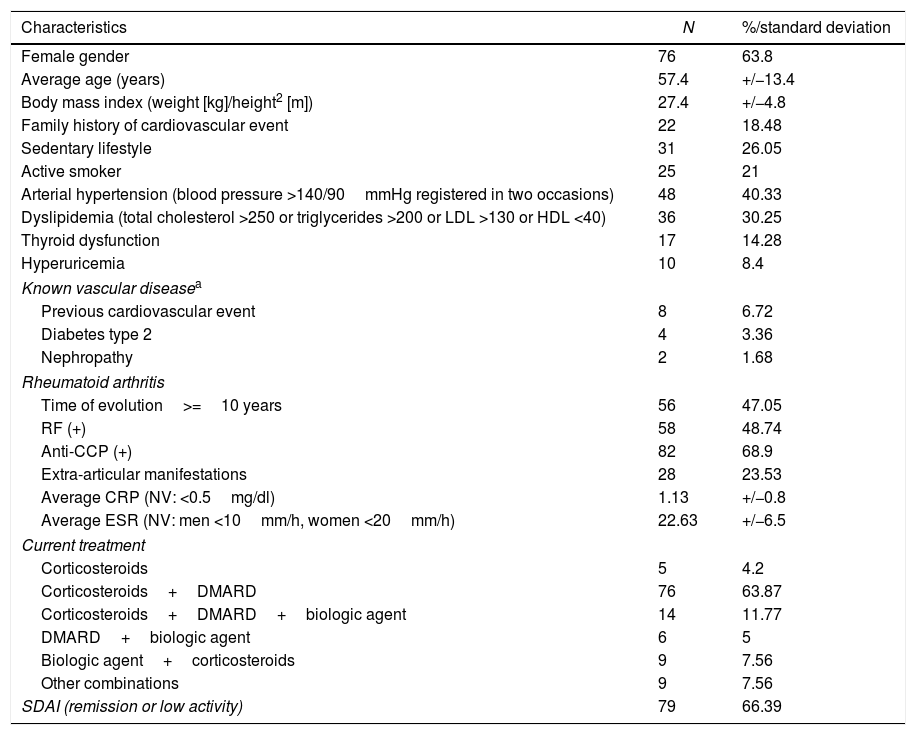
ResultsDuring the study period, a total of 119 patients with RA (63.87% female, 36.13% male) accepted to participate (Table 1).
Clinical profile of the 119 patients with rheumatoid arthritis of the HGUCR.
| Characteristics | N | %/standard deviation |
|---|---|---|
| Female gender | 76 | 63.8 |
| Average age (years) | 57.4 | +/−13.4 |
| Body mass index (weight [kg]/height2 [m]) | 27.4 | +/−4.8 |
| Family history of cardiovascular event | 22 | 18.48 |
| Sedentary lifestyle | 31 | 26.05 |
| Active smoker | 25 | 21 |
| Arterial hypertension (blood pressure >140/90mmHg registered in two occasions) | 48 | 40.33 |
| Dyslipidemia (total cholesterol >250 or triglycerides >200 or LDL >130 or HDL <40) | 36 | 30.25 |
| Thyroid dysfunction | 17 | 14.28 |
| Hyperuricemia | 10 | 8.4 |
| Known vascular diseasea | ||
| Previous cardiovascular event | 8 | 6.72 |
| Diabetes type 2 | 4 | 3.36 |
| Nephropathy | 2 | 1.68 |
| Rheumatoid arthritis | ||
| Time of evolution>=10 years | 56 | 47.05 |
| RF (+) | 58 | 48.74 |
| Anti-CCP (+) | 82 | 68.9 |
| Extra-articular manifestations | 28 | 23.53 |
| Average CRP (NV: <0.5mg/dl) | 1.13 | +/−0.8 |
| Average ESR (NV: men <10mm/h, women <20mm/h) | 22.63 | +/−6.5 |
| Current treatment | ||
| Corticosteroids | 5 | 4.2 |
| Corticosteroids+DMARD | 76 | 63.87 |
| Corticosteroids+DMARD+biologic agent | 14 | 11.77 |
| DMARD+biologic agent | 6 | 5 |
| Biologic agent+corticosteroids | 9 | 7.56 |
| Other combinations | 9 | 7.56 |
| SDAI (remission or low activity) | 79 | 66.39 |
Anti-CCP: anti-cyclic citrullinated peptide; DMARD: disease modifying antirheumatic drug; RF: rheumatoid factor; kg: kilograms; m: meters; CRP: C-reactive protein; SDAI: simplified disease activity index; NV: normal value; ESR: erythrocyte sedimentation rate.
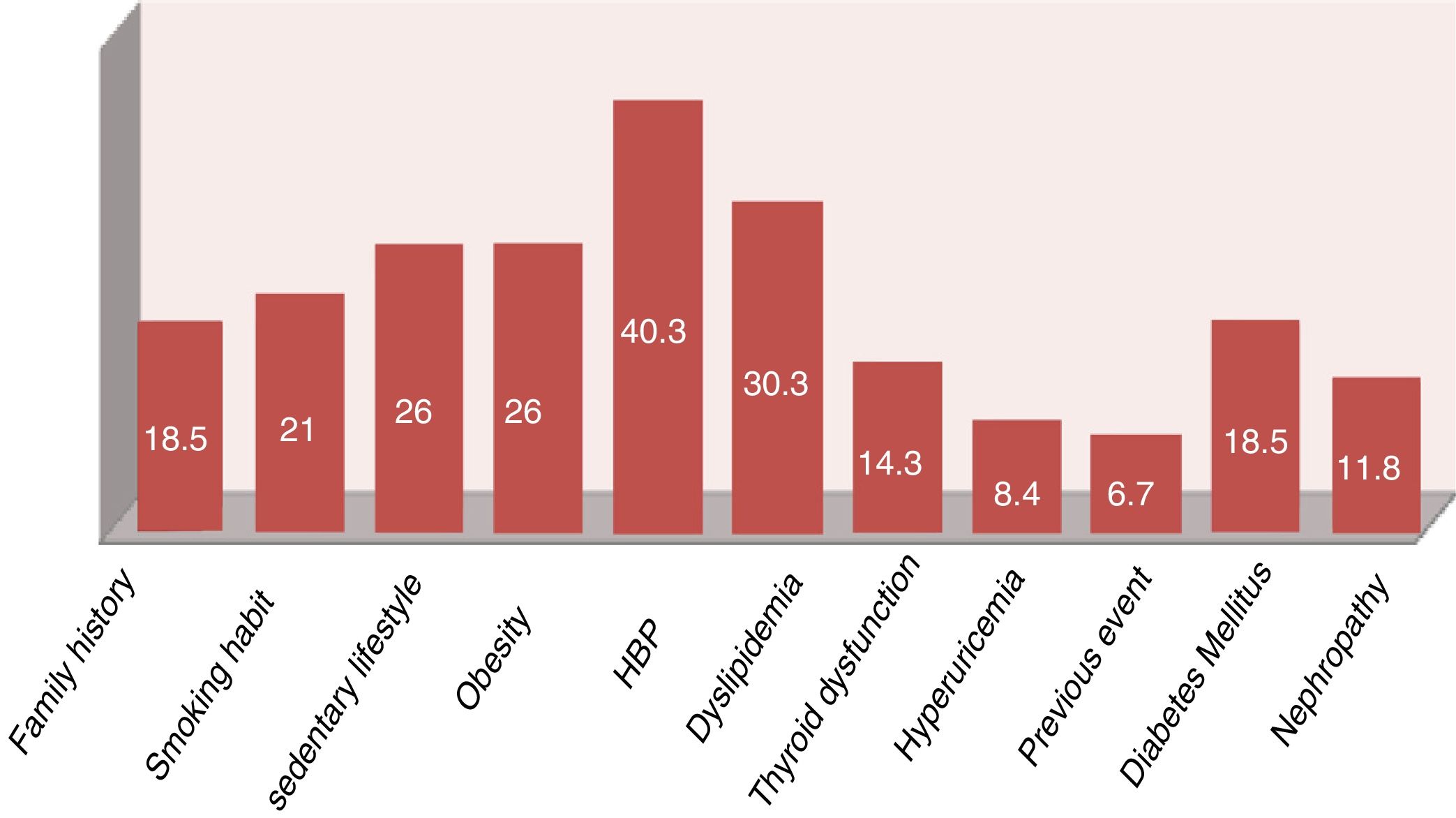
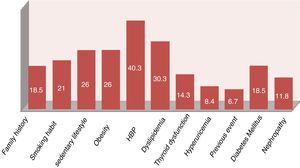
In the studied population stood out a high prevalence of 84.87% for the presence of some CVR factor and of 73.1% for the classical factors (some patients had more than one factor). Likewise, 6.72% had suffered a cardiovascular event at the time of the study.
Regarding the RA, it was observed a prevalence of 79.83% of positive serological markers (RF and/or anti-CCP), as well as a time of evolution longer than 10 years in almost 50% of our population. Likewise, 66% had an adequate control of the disease, both globally by the SDAI as well as by the presence of biological markers of inflammatory activity. The most frequent treatment was the use of corticosteroid therapy at doses of 5–10mg/day of prednisone or equivalent, and disease modifying drugs (DMARDs) (mainly methotrexate).
The 11 patients with known vascular disease (previous events, diabetes mellitus or nephropathies) were cataloged in the very high CVR according to the indications of the clinical guidelines.28 The calculation of the SCOREm was made to the 108 remaining patients, being stratified as follows: 48 low risk, 54 intermediate risk, 6 high risk and none of very high risk. However, with the results of the specific analytical study (basal glucose, lipid and thyroid profile, creatinine, glomerular filtration rate, glycated hemoglobin, uric acid, acute phase reactants, RF, anti-CCP, etc.) a recent diagnosis of diabetes mellitus or nephropathy was made in 27 patients (18 with altered glycated hemoglobin and 12 with glomerular filtration rate <60ml/min, 3 patients with both findings), which increased the prevalence of CVR factors (Fig. 2). The final stratification of the CVR in our studied population is shown in Fig. 3.
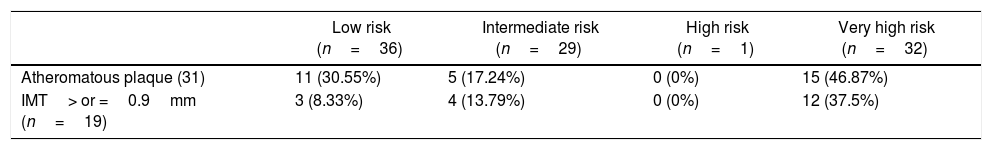
A simple random sampling of the 119 patients was carried out (95.5% confidence level and sampling error of 5%) to perform a carotid ultrasound (n=92), which is why a carotid ultrasound was performed finally to a total of 98 patients. 31 (31.63%) patients with presence of atheromatous plaque and 19 (19.39%) patients with an IMT ≥0.90 were found, both considered as data of subclinical atherosclerosis. The distribution of the echographic findings according to the risk stratification by SCOREm is described in Table 2.
Distribution of the ultrasound findings according to the stratification by SCOREm.
| Low risk (n=36) | Intermediate risk (n=29) | High risk (n=1) | Very high risk (n=32) | |
|---|---|---|---|---|
| Atheromatous plaque (31) | 11 (30.55%) | 5 (17.24%) | 0 (0%) | 15 (46.87%) |
| IMT> or =0.9mm (n=19) | 3 (8.33%) | 4 (13.79%) | 0 (0%) | 12 (37.5%) |
IMT: intima-media thickness.
In our study, a prevalence of 84.87% for the CVR factors (classical factors 73.1%) and of 6.72% of previous events (myocardial infarction, peripheral arteriopathy, etc.) was observed in the studied population. Being the final result for the stratification, 33.6% of high and very high risk. This high prevalence of factors and CVR has been described in other studies conducted on the population with RA.8–11,15 It has even been compared with that described in patients with diabetes mellitus type 2.6,7 For all these reasons, the involvement of the rheumatologist in the recognition of this important commitment and its assessment is becoming increasingly necessary. This compels us to take an active role and to be the starting point and the cornerstone in the cardiovascular prevention of this population. Despite this, it is observed that in the current clinical practice, the assessment and estimation of the CVR of the patients with RA is not carried out or underestimated.29,30 In some countries, there have been created units of cooperation between Rheumatology and Cardiology such as the Preventive Cardio-Rheuma Clinic of the Department of Rheumatology of the Diakonhjemmet Hospital (Norway) and the Cardio-Rheuma Clinic of the Division of Cardiovascular Diseases of the Mayo Clinic (United States of North America)31,32 that provide an integral approach to the patient with RA. Likewise, strategies have been proposed with good results, such as incorporating the participation of other types of healthcare personnel to carry out the estimation of the CVR through predetermined programs and tables and thus optimize the rheumatological consultation.33,34
Despite the EULAR recommends an annual assessment of the CVR in the patients with RA, it is observed that this is not carried out adequately, being closer to that of the population without RA and up to 12-fold less frequent than that conducted in patients with diabetes mellitus35; underestimating the determination of the basal glucose in 27% and the lipid profile in 14%, which can be determinant in up to 30% of the population for an unknown or under-treated diagnosis.36,37 In our series, 22.68% had an underdiagnosis of diabetes mellitus or nephropathy.
Recently, a panel of experts has proposed a series of modifications and new recommendations based on the EULAR 2010 recommendations for the approach and management of CVR in patients with RA, highlighting the following38:
- •
Annual cardiovascular assessment should be made to all RA patients without evidence of known CVD, mainly to: seropositives, RF (+) or anti-CCP (+), extra-articular manifestations, metabolic syndrome or time of evolution >10 years.
- •
Perform, according to the experience and equipment of each center, a complementary assessment by carotid ultrasound or ankle/brachial index to the patients with low/intermediate risk (SCOREm 0–4%).
- •
Maintain healthy lifestyles. Treatment with statins for primary prevention of cardiovascular events and maintain adequate levels of LDL in the patients at high risk (very high risk (SCOREm >10%): LDL<70mg/dl, high risk (SCOREm 5–9%): LDL<100mg/dl).
- •
The control of the disease activity and the inflammatory burden with DMARDs is directly related with a decrease in the CVR.
- •
Use of NSAIDs the shortest time possible and of corticoids at the lowest possible doses.
During the last years, different algorithms have been used, modified and developed for an adequate stratification of the CVR risk in the population with RA (Framingham, PROCAM, SCORE, Reynolds, QRISK 2)22; incorporating biochemical markers of inflammation as well as clinical and serological characteristics of the disease (Reynolds, QRISK 2 and SCOREm), however, it has been observed that none of them classifies the patients adequately into risk groups, presenting a sensitivity and specificity lower than expected (68–87% and 55–76%, respectively),22,39 which causes that up to 32% of the CV events can occur in the population classified as low risk according to these tools.40–42 In our study we observed the presence of atheromatous plaques in 30% of the population cataloged as low risk according to the SCOREm; which determines that a non-negligible percentage of patients classified as low risk by SCOREm present subclinical atherosclerosis. All of this expresses a limitation in the capacity that these classification algorithms have to detect those who do not have the condition sought (true negatives). For this reason, as in the study of González-Gay et al.,43 the use of carotid ultrasound is recommended in those patients with low/intermediate risk for their reclassification.
Due to all this, it can be concluded that there is a high prevalence of classical CVR factors in the population with RA and 30% of the patients cataloged as low risk by SCOREm exhibit data of subclinical atherosclerosis by carotid ultrasound. That is why we recommend a greater participation of the rheumatologist in the recognition of this important and potentially fatal condition for its correct assessment, stratification, treatment and follow-up. As well as the performance of the carotid ultrasound in the patients with RA who initially are not classified as high/very high risk according to the available stratification tables. This would allow us to reclassify the patients and change our clinical, therapeutic and follow-up attitude.
Finally, even though RA manifests itself more apparently in the joints, it should be considered a systemic disease associated with a higher incidence of cardiovascular events.
The main limitation of the study is the sample size. However, the effect of low power has not been definitive since we have obtained relevant results that reinforce what has been observed in other studies of similar characteristics and methodology.
Conflict of interestThe authors declare they do not have any conflict of interest.
Our gratitude to the disinterested support of the Services of Rheumatology, Diagnostic Radiology and Clinical Analysis of the University Hospital of Ciudad Real.
Please cite this article as: Huaranga MA, Sánchez MD, Díaz de la Espina MÁ, Rodríguez MR, Díaz JL, Aguilera GR. Artritis reumatoide, una enfermedad sistémica con un riesgo cardiovascular subestimado. Rev Colomb Reumatol. 2018;25:92–98.