Systemic lupus erythematosus is a multisystemic disease that is associated with an increase in morbidity. Several classification criteria, with a variable performance, have been published in the last few years. The Systemic Lupus International Collaborating Clinics (SLICC) recently developed a new version that has been validated in children and adults. The performance of these criteria in Colombian juvenile lupus patients is unknown.
ObjectivesTo evaluate the sensitivity and specificity of the SLICC criteria in a group of patients with juvenile systemic lupus erythematosus in Bogotá, Colombia.
Materials and methodsRetrospective evaluation of clinical and laboratory data during the first month of disease in patients with juvenile systemic lupus erythematosus and in control patients followed-up in a paediatric rheumatology clinic.
ResultsThe study subjects (n=110), with a mean age of 11.1 years (2–16 years), were divided equally into cases and controls. The gender ratio in cases was F:M 5.4:1 and in controls 1.8:1. The ACR 1997 and SLICC criteria were analysed in both groups of patients. The sensitivity and specificity of ACR criteria were 78% and 96%, respectively, and in SLICC criteria were 89% and 87%, respectively.
ConclusionsIn this group of paediatric patients, the sensitivity of SLICC criteria during the first month of diagnosis was higher than the ACR 1997 criteria. This was associated with a lower specificity. These results are similar to those of previous studies.
El lupus eritematoso sistémico es una enfermedad multisistémica que se acompaña de importante morbilidad. A través de los años se han publicado diversos criterios de clasificación con un desempeño variable. Recientemente el grupo de Clínicas de Colaboración del Lupus Eritematoso Sistémico (SLICC) propone una versión que ha sido validada en niños y adultos. No se conoce el desempeño de estos criterios en la población juvenil colombiana con lupus eritematoso sistémico.
ObjetivosEvaluar la sensibilidad y la especificidad de los criterios SLICC en una población pediátrica con lupus eritematoso sistémico juvenil en la ciudad de Bogotá, Colombia.
Materiales y métodosEvaluación retrospectiva de datos clínicos y paraclínicos durante el primer mes de enfermedad en los pacientes con lupus eritematoso sistémico juvenil y en los pacientes controles valorados en una consulta de reumatología pediátrica.
ResultadosN=110, 55 casos y 55 controles. La edad promedio de inicio en los casos fue de 12,8 años (7-15 años) y en controles 11,1 años (2-15 años). La distribución por sexo en los casos fue de F:M 5,4:1 y en los controles F:M 1,8:1. Se aplicaron los criterios ACR 1997 y SLICC a ambos grupos de pacientes. La sensibilidad y la especificidad de los criterios ACR fue del 78 y 96% y de los criterios SLICC fue del 89 y 87%, respectivamente.
ConclusionesEn este grupo de pacientes pediátricos la sensibilidad de los criterios SLICC en el primer mes de diagnóstico fue mayor al compararla con los criterios ACR 1997. Esto se acompañó de una menor especificidad. Estos hallazgos concuerdan con estudios previos.
Systemic lupus erythematosus (SLE) is a multiorgan disease. About 20% of the cases begin before the age of 16 years, being classified as juvenile-onset systemic lupus erythematosus (jSLE). This disease is more common in women and has a significant morbidity and mortality. Timely diagnosis and treatment impact the short- and long-term prognosis.
The classification criteria, in addition of being frequently used in clinical practice, provide homogeneity in the field of research. Over the years, several proposals have been published. In 1971 Cohen et al.1 published the preliminary criteria consisting of 14 items, which were later reviewed and updated in 1982 and in 1997 by the American College of Rheumatology (ACR) for adult patients. In this last review, the LE cells were eliminated and the immunological criteria were modified including the antiphospholipid antibodies. In 1994 Ferraz et al.2 assessed the 1982 criteria for the pediatric population finding that with the presence of 4 or more criteria, the sensitivity was 96.1% and the specificity was 100%.
Recently, the Systemic Lupus International Collaborating Clinics (SLICC) group conducted the review of the ACR criteria.3 In the adult population it was found with this proposal a higher sensitivity with respect to the 1997 ACR criteria (97 vs. 83%), but a lower specificity (84 vs. 96%); in 2017 Aberle et al.4 reported, similarly, a higher sensitivity of the criteria of the SLICC group and observed a greater heterogeneity of the disease that includes a greater potential for organ involvement in the patients who fulfilled the criteria of the SLICC group and not those of the ACR.
In 2014, Sag et al.5 carried out the validation of these classification criteria in the pediatric population, finding results similar to those previously described in adults. The sensitivity observed was higher when compared with the 1997 ACR criteria (98.7 vs. 76.6%), but with a lower specificity (85.3 vs. 93.4%).
It has been documented not only a greater severity of SLE in the pediatric population when compared with adults, but also differences in the clinical presentation depending on the geographical location. The performance of the SLICC group criteria in the Colombian population is not known so far.
The objective of this study was to evaluate the sensitivity and specificity of the criteria of the SLICC group in a pediatric population with jSLE from the city of Bogota, Colombia.
MethodsA retrospective evaluation of the findings present in the first month of diagnosis was carried out in patients with jSLE evaluated in a pediatric rheumatology clinic in the city of Bogotá, Colombia, during the period between May 2007 and March 2016. Control patients with different diagnoses who attended the pediatric rheumatology clinic during the same period were included. A single data collection format was used to collect the information on the patients with lupus and the controls. The opinion of the expert of the center was used as the gold standard for the diagnosis of lupus. The sensitivity of the criteria of the ACR and the SLICC group was evaluated during the first month of onset of the symptoms. The specificity of each group of criteria was assessed against the control patients. The sensitivity and specificity of the criteria of the ACR 1997 and the SLICC group 2012 were evaluated in the patients with jSLE.
ResultsA total of 110 patients were included. Half corresponded to cases. The control patients had the following diagnoses: juvenile idiopathic arthritis (n=24), dermatomyositis (n=7), autoimmune hematologic diseases (n=6), antiphospholipid syndrome (n=6), systemic vasculitis (n=5), overlapping syndromes (n=4), poorly differentiated autoimmune disease (n=2) and autoimmune hepatitis (n=1). The average age of onset in the cases was 12.8 years (7–15 years) and in the controls 11.1 years (2–15 years). The distribution by gender in the cases was F:M 5.4:1 and in controls F:M 1.8:1.
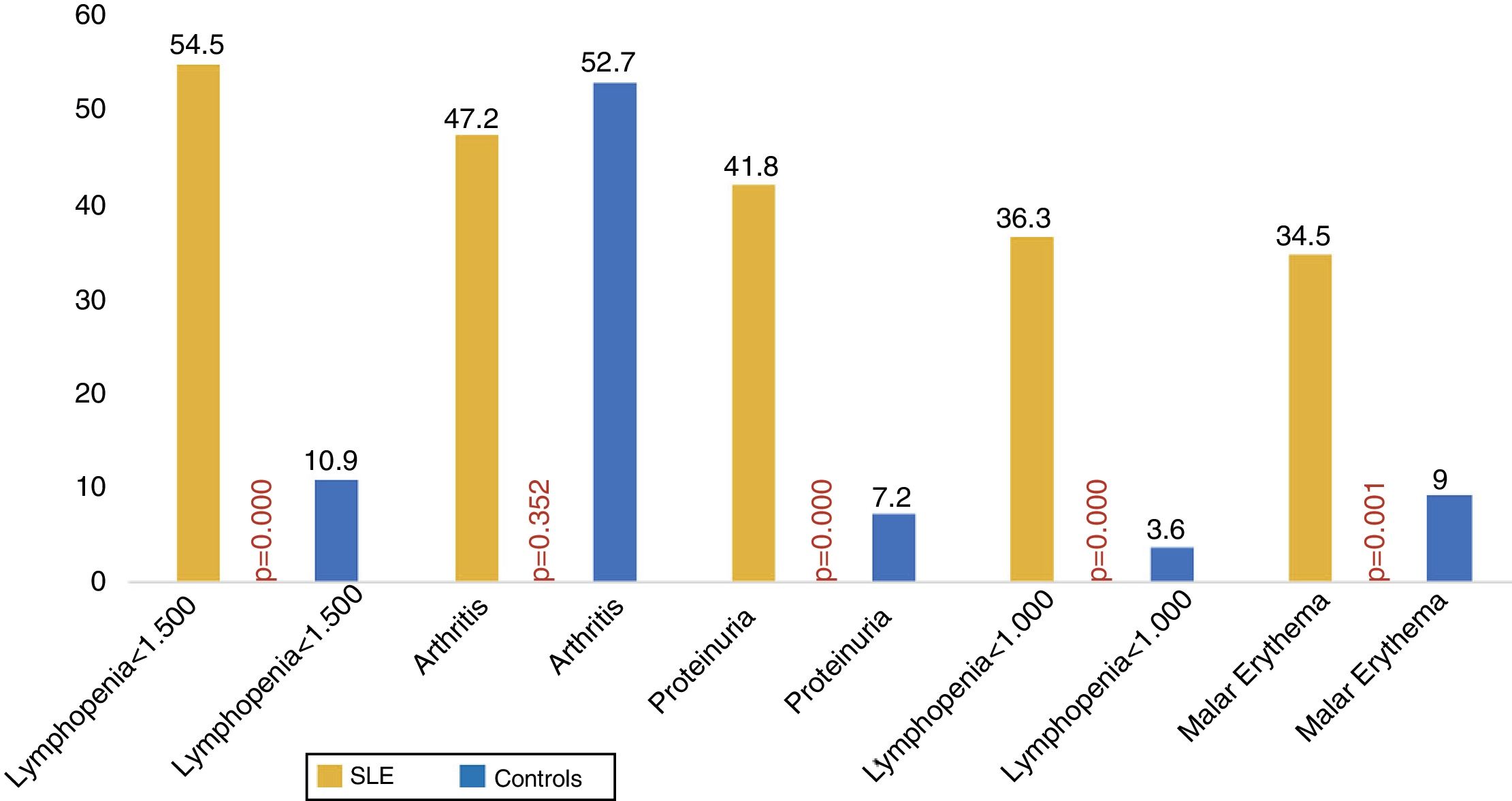
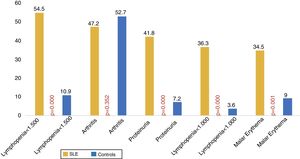
The most prevalent clinical manifestations during the first month of disease in the patients with jSLE were: lymphopenia less than 1500, arthritis, proteinuria, lymphopenia less than 1000 and malar erythema (Fig. 1).
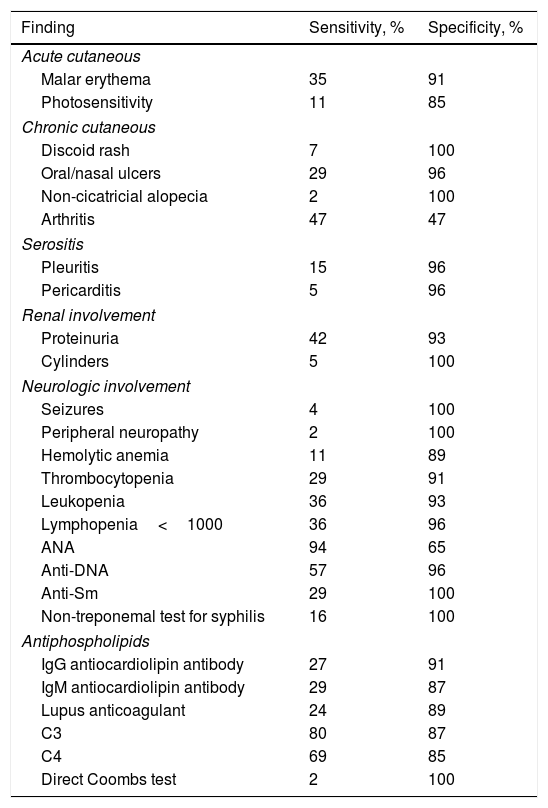
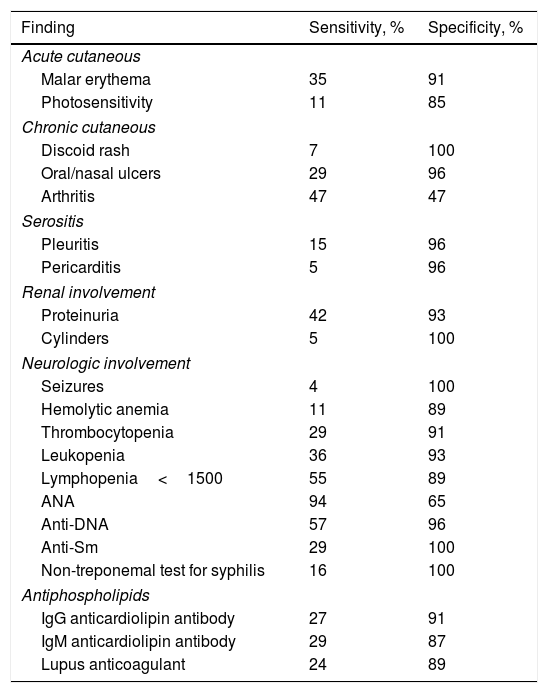
The sensitivity and specificity of each criterion of the SLICC group and of the ACR 1997 in patients with jSLE are detailed in Tables 1 and 2, respectively.
Sensitivity and specificity of each SLICC criterion in patients with jSLE.
| Finding | Sensitivity, % | Specificity, % |
|---|---|---|
| Acute cutaneous | ||
| Malar erythema | 35 | 91 |
| Photosensitivity | 11 | 85 |
| Chronic cutaneous | ||
| Discoid rash | 7 | 100 |
| Oral/nasal ulcers | 29 | 96 |
| Non-cicatricial alopecia | 2 | 100 |
| Arthritis | 47 | 47 |
| Serositis | ||
| Pleuritis | 15 | 96 |
| Pericarditis | 5 | 96 |
| Renal involvement | ||
| Proteinuria | 42 | 93 |
| Cylinders | 5 | 100 |
| Neurologic involvement | ||
| Seizures | 4 | 100 |
| Peripheral neuropathy | 2 | 100 |
| Hemolytic anemia | 11 | 89 |
| Thrombocytopenia | 29 | 91 |
| Leukopenia | 36 | 93 |
| Lymphopenia<1000 | 36 | 96 |
| ANA | 94 | 65 |
| Anti-DNA | 57 | 96 |
| Anti-Sm | 29 | 100 |
| Non-treponemal test for syphilis | 16 | 100 |
| Antiphospholipids | ||
| IgG antiocardiolipin antibody | 27 | 91 |
| IgM antiocardiolipin antibody | 29 | 87 |
| Lupus anticoagulant | 24 | 89 |
| C3 | 80 | 87 |
| C4 | 69 | 85 |
| Direct Coombs test | 2 | 100 |
jSLE: juvenile-onset systemic lupus erythematosus; SLICC: Systemic Lupus International Collaborating Clinics.
Sensitivity and specificity of each ACR 1997 criterion in patients with jSLE.
| Finding | Sensitivity, % | Specificity, % |
|---|---|---|
| Acute cutaneous | ||
| Malar erythema | 35 | 91 |
| Photosensitivity | 11 | 85 |
| Chronic cutaneous | ||
| Discoid rash | 7 | 100 |
| Oral/nasal ulcers | 29 | 96 |
| Arthritis | 47 | 47 |
| Serositis | ||
| Pleuritis | 15 | 96 |
| Pericarditis | 5 | 96 |
| Renal involvement | ||
| Proteinuria | 42 | 93 |
| Cylinders | 5 | 100 |
| Neurologic involvement | ||
| Seizures | 4 | 100 |
| Hemolytic anemia | 11 | 89 |
| Thrombocytopenia | 29 | 91 |
| Leukopenia | 36 | 93 |
| Lymphopenia<1500 | 55 | 89 |
| ANA | 94 | 65 |
| Anti-DNA | 57 | 96 |
| Anti-Sm | 29 | 100 |
| Non-treponemal test for syphilis | 16 | 100 |
| Antiphospholipids | ||
| IgG anticardiolipin antibody | 27 | 91 |
| IgM anticardiolipin antibody | 29 | 87 |
| Lupus anticoagulant | 24 | 89 |
jSLE: juvenile-onset systemic lupus erythematosus.
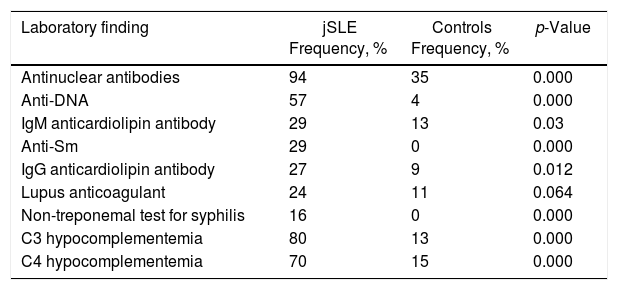
The most frequent laboratory findings in patients with jSLE were the presence of antinuclear antibodies, followed by C3 and C4 hypocomplementemia, respectively. Their frequency in patients with jSLE and controls is described in Table 3.
Frequency of antibodies and other laboratory findings in patients with jSLE and in controls.
| Laboratory finding | jSLE Frequency, % | Controls Frequency, % | p-Value |
|---|---|---|---|
| Antinuclear antibodies | 94 | 35 | 0.000 |
| Anti-DNA | 57 | 4 | 0.000 |
| IgM anticardiolipin antibody | 29 | 13 | 0.03 |
| Anti-Sm | 29 | 0 | 0.000 |
| IgG anticardiolipin antibody | 27 | 9 | 0.012 |
| Lupus anticoagulant | 24 | 11 | 0.064 |
| Non-treponemal test for syphilis | 16 | 0 | 0.000 |
| C3 hypocomplementemia | 80 | 13 | 0.000 |
| C4 hypocomplementemia | 70 | 15 | 0.000 |
jSLE: juvenile-onset systemic lupus erythematosus.
Most of the criteria showed high specificity, but not sensitivity. The presence of antinuclear antibodies, C3 or C4 hypocomplementemia, anti-DNA, lymphopenia of less than 1500, arthritis, proteinuria and malar erythema were associated with a greater sensitivity. Some of the items present in the classification criteria of the SLICC group were not observed in this group of patients (mononeuritis multiplex, myelitis and acute confusional state). One patient presented peripheral neuropathy. Anti-β2-glycoprotein and IgA anticardiolipin antibodies, as well as the CH50 complement protein were not measured in the majority of patients.
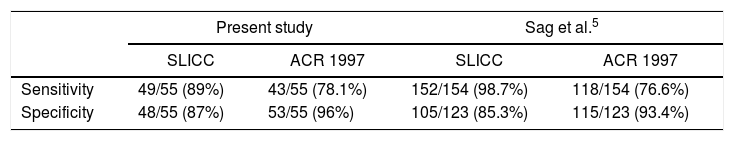
During the first month of diagnosis, 78.1% of the cases met the criteria of the ACR and 89.1% fulfilled the criteria of the SLICC group. The sensitivity of the SLICC group criteria was higher than in the ACR criteria, with lower specificity (Table 4).
Sensitivity and specificity of the SLICC and ACR 1997 criteria in the diagnosis of jSLE in the present study and in the series of Sag et al.5
| Present study | Sag et al.5 | |||
|---|---|---|---|---|
| SLICC | ACR 1997 | SLICC | ACR 1997 | |
| Sensitivity | 49/55 (89%) | 43/55 (78.1%) | 152/154 (98.7%) | 118/154 (76.6%) |
| Specificity | 48/55 (87%) | 53/55 (96%) | 105/123 (85.3%) | 115/123 (93.4%) |
jSLE: juvenile-onset systemic lupus erythematosus; SLICC: Systemic Lupus International Collaborating Clinics.
No patient without a diagnosis of SLE met the ACR criteria (2 patients with overlapping syndrome who fulfilled the criteria had jSLE), while 2 patients with primary antiphospholipid syndrome, one patient with poorly differentiated autoimmune disease, one patient with autoimmune hepatitis and one patient with Evans syndrome fulfilled the criteria of the SLICC group. Two patients with overlapping syndrome that included SLE also fulfilled the criteria of the SLICC group.
DiscussionIn this group of patients with jSLE, the criteria of the SLICC group showed a better performance by being able to identify a greater number of patients with jSLE, however, similar to that was reported by Petri et al.3 and Sag et al.,5 the specificity is lower when compared with the ACR 1997 criteria. The misclassification of two patients with primary antiphospholipid syndrome and one patient with Evans syndrome using the classification criteria of the SLICC group could be secondary to the separation of the hematological criteria and to the classification of antiphospholipid antibodies as an independent criterion in the immunological criteria.
In this study, the criteria that showed greater sensitivity in the patient with jSLE were positive ANAs, the presence of anti-DNA, arthritis, proteinuria, malar erythema, lymphopenia <1500 and C3 or C4 hypocomplementemia. All of the above are included in both classification criteria, except the last 2 which are part of the criteria of the ACR and of the SLICC group, respectively. It is highlighted that 6% of the patients with jSLE were negative for ANA, similarly to what is reported in the literature.
The inclusion of hypocomplementemia in the criteria of the SLICC group is considered important given its high sensitivity and specificity observed in this group of patients with jSLE. The greater decrease in the lymphocyte count required in the criteria of the SLICC group (from 1500 in the ACR to 1000 in the SLICC group) was associated with a decrease in the sensitivity of this criterion with an increase in the specificity. However, the need for an altered sample compared with at least 2 altered samples in the ACR criteria, could help that this decrease in sensitivity is not so marked.
The broadening of the dermatological criteria in the criteria of the SLICC group (acute, subacute and chronic) allows to identify a greater number of patients with jSLE and, although in this sample of patients only was observed the presence of non-cicatricial alopecia within the new added criteria and its sensitivity was only 2%, its specificity reached 100%. Something similar occurred in the neurological system, although it only was observed the presence of peripheral neuropathy within the new criteria added to the SLICC group (sensitivity of 2%), it also showed a specificity of 100%. No cases of myelitis, acute confusional state, cranial neuropathy and mononeuritis multiplex (included in the criteria of the SLICC group), and of psychosis, included in both classification criteria, were observed.
The separation of the anti-DNA, anti-Sm and antiphospholipid antibodies into independent criteria allows for a greater identification of patients with jSLE by increasing the number of serological criteria present at diagnosis.
Diseases other than SLE or cytopenias could be misclassified as jSLE when using the criteria of the SLICC group. It should be clarified that autoimmune cytopenias can evolve to a jSLE during the follow-up time and in this scenario the criteria of the SLICC group would increase the diagnostic sensitivity.
The clinical judgment of the treating physician prevails over the classification criteria at the time of the diagnosis of the jSLE, and it should not be forgotten that they are classification criteria, but not diagnostic criteria. The patients with overlapping syndromes who fulfilled criteria of the ACR and the SLICC group had the diagnosis of jSLE as one of their rheumatic diseases; therefore, they are not considered a misclassification of jSLE.
The main limitation of this study lies in its retrospective nature that could be associated with information biases when obtaining the data of the patient's clinical history.
ConclusionsIn this group of pediatric patients, the sensitivity of the criteria of the SLICC group in the first month of diagnosis was higher and the specificity was lower than that of the 1997 ACR criteria. These findings are consistent with those reported in other pediatric and adult groups. Given the greater severity of the disease in the pediatric population, early diagnosis allows the timely initiation of treatment. The education and implementation of these new criteria should be promoted taking into account their advantages and disadvantages.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Arango C, Mosquera C. Evaluación de los criterios de clasificación SLICC en pacientes con lupus eritematoso sistémico juvenil seguidos en una clínica pediátrica de Bogotá, Colombia. Rev Colomb Reumatol. 2018;25:99–103.