Wrist involvement is common in patients with rheumatoid arthritis.
Patients with persistent pain and swelling despite medical therapy are candidates for surgery.
The aim of this paper is to describe medical aspects and indications and types of surgeries in a rheumatoid wrist.
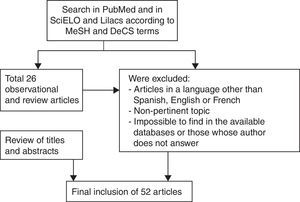
Materials and methodsThe keywords chosen in Spanish and English were rheumatoid hand or wrist, rheumatoid arthritis and hand or wrist rheumatoid arthritis, radiosynovectomy in rheumatoid arthritis or arthritis. Finally 52 articles were selected.
ResultsWhen there is not good response to medical treatment before going to surgery, local infiltration of corticosteroids and radiosynovectomy can be used.
The synovectomy and tenosynovectomy give symptomatic relief and improve function in the short term. Extensor and flexor tendons may rupture due to synovial infiltration and irritation caused by bone prominences, such as ulnar head subluxation.
When tendon ruptures occur, tendon grafts or tendon transfers are the solution. Carpal instability, severe arthritis and joint damage often require stabilization surgery on the bones.
The distal radioulnar joint often initially affected, procedures like Sauvé–Kapandji technique or Darrach go great in this joint.
The partial arthrodesis radio-carpal offers stability in the involved joint, respecting and preserving in the medio-carpal joint some mobility. When there is already a global osteoarthritis, total wrist fusion provides good results in relieving pain and stability.
Total wrist arthroplasty is an alternative that preserves the movement; however the long-term results remain to be seen.
El compromiso de la muñeca es común en la artritis reumatoide. Pacientes con persistencia de dolor e inflamación, a pesar de tratamiento farmacológico, son candidatos para cirugía. El objetivo de este artículo es mostrar aspectos médico-quirúrgicos e indicaciones y tipos de cirugías, en una muñeca reumatoidea.
Materiales y métodosLas palabras clave escogidas en español e inglés fueron: mano o muñeca reumática, artritis reumatoidea y mano, artritis reumatoidea y muñeca, radiosinovectomía-artritis reumatoidea y en artritis. Finalmente, se escogieron 52 artículos.
ResultadosCuando no hay buena respuesta al tratamiento farmacológico antes de pasar al tratamiento quirúrgico, la infiltración local de corticoides y la radiosinovectomía pueden ser usadas.
Las sinovectomías y tenosinovectomías dan alivio sintomático y mejoran la función a corto plazo. Los tendones extensores y flexores pueden romperse por la infiltración sinovial y la irritación ocasionada por protuberancias óseas, como la subluxación dorsal del cúbito.
Cuando hay roturas tendinosas se recurre a injertos o transferencias tendinosas. Inestabilidades del carpo, artritis severa y daño articular a menudo requieren cirugías óseas. La articulación radiocubital distal suele verse afectada inicialmente y los procedimientos de Sauvé-Kapandji o la técnica de Darrach funcionan bien en esta articulación.
La artrodesis parcial radiocarpiana da estabilidad a la articulación más comprometida, respetando la mediocarpiana y conservando cierta movilidad. Cuando hay una artrosis global, la artrodesis total de muñeca brinda buenos resultados en cuanto al alivio del dolor y estabilidad.
La artroplastia total de muñeca es una alternativa que preserva el movimiento; sus resultados a largo plazo están por verse.
Rheumatoid arthritis (RA) is a progressive and destructive disease, whose systemic manifestations can become serious. More than 70% of patients develop alterations in the hands that generate pain and functional limitation. The gradual loss of hand function can affect the self-care, the productivity at work or in daily life, and the patient can be socially stigmatized because of the deformities.
The patient with RA seeks help from a surgeon to relieve pain, to achieve functional gain and, finally and sometimes most important, seeks an improvement in the esthetic appearance.1,2 Whether surgeries help or not is sometimes controversial, and the lack of rigorous studies determining the effectiveness of some hand surgeries, has led to many disagreements between rheumatologists and hand surgeons regarding the recommendations to undertake the reconstruction of a rheumatoid hand,3 however, the main surgeries in which there is almost no discussion are the repairs of extensor tendon ruptures, wrist surgeries and some metacarpophalangeal arthroplasties.
RA is a chronic condition and its activity may change over time.4 The knowledge of the disease and its possible course, as well as of the different therapeutic tools, is important to be able to give the patient the best possible treatment. The purpose of this review is to show the surgical aspects that take place in the treatment of a rheumatic wrist.
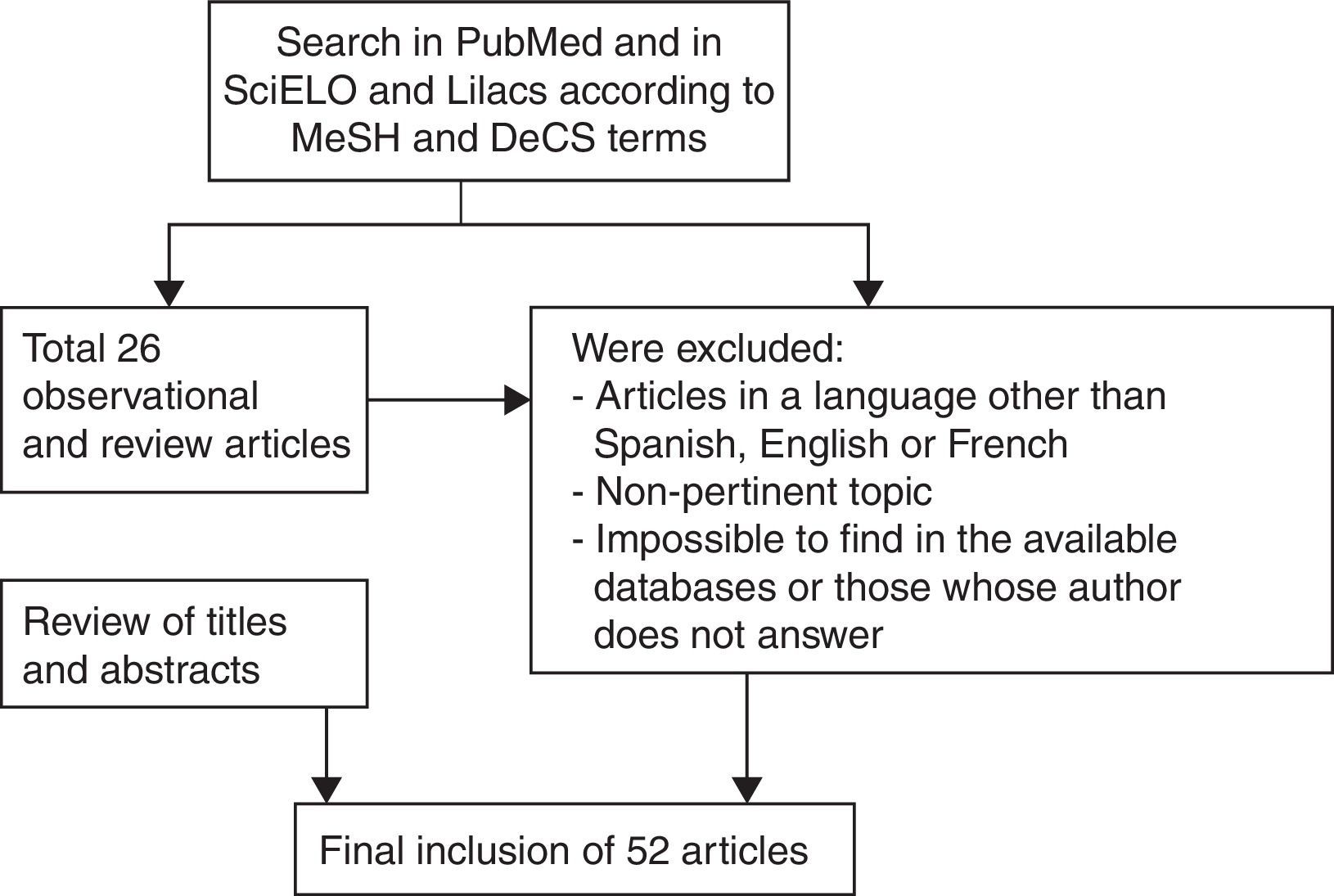
Materials and methodsIn order to carry out a review of the role of surgery in the treatment of an affected wrist in RA; the following keywords were chosen: mano reumática, muñeca reumática, artritis reumatoidea y mano, artritis reumatoidea y muñeca, and artritis reumatoidea y sinovectomía. Radiosinovectomía en artritis reumatoidea and radiosinovectomia en artritis were also searched. The same was done in English with the keywords: rheumatoid hand, rheumatoid hand surgery, rheumatoid wrist, and rheumatoid wrist surgery. “Radiosynovectomy and rheumatoid arthritis” and “radiosynovectomy and arthritis” were also used.
Only were taken the reviews published in the last 10 years.
It was conducted a bibliographic search in the Medline Pubmed database for articles published in English and in the Scielo and Lilacs databases for articles published in Spanish and Portuguese. All observational studies, systematic reviews and reviews were searched.
We also resorted to 3 classical texts, which are consulted very often in the area of hand surgery: Hand surgery (Merle), Operative hand surgery (Green) and The hand (Tubiana).
On rheumatoid hand surgery were found 16 articles and 2 reviews, on rheumatoid wrist surgery were found 130 articles and 47 reviews.
For “radiosynovectomy and rheumatoid arthritis” we found 5 reviews and observational studies, of which 4 were reviews. For “radiosynovectomy and arthritis” only 10 articles were found.
When crossing in the databases in Spanish AR and cirugía de mano we did not find any article on this subject, between AR and sinovectomía we found 5 articles which did not conform to our work, and for radiosinovectomía en artritis we only found one article.
After reviewing the abstracts of all articles, 52 articles and reviews that were the basis of this review article were chosen (Fig. 1).
ResultsEpidemiologyThe global prevalence of clinical RA is estimated at 1%, however, there is evidence that supports its variability in time and place.4–6 Regarding the incidence of RA in Latin America, studies in Colombia and Peru determine a variable incidence between 0.1 and 0.5%, respectively; however, the Colombian study is not a COPCORD (Community oriented program for the control of rheumatic diseases) study.7,8
The wrist joint is frequently affected in patients with RA, being considered that 2/3 of patients with RA have at least one symptom associated with the wrist in the first 2 years after diagnosis, and this number increases to above 90% at 10 years.4,9
EtiologyThe etiology of RA is still subject to research. It has been demonstrated the association between RA and a group of membrane receptors of the major histocompatibility complex (MHC class II) encoded by alleles of the HLA-DR locus on chromosome 6.10–12
This particular set of alleles is highly predictive of the potential of the carrier to develop RA; however, other studies have demonstrated that genetic factors are not the only determinants of RA.13
It has been suggested that certain infections predispose to RA or might trigger it; however, the causal agents have only been implicated in a circumstantial way and a specific pathogen generator of RA has not been isolated.13–15
Tobacco has also been found as an etiological factor for RA, being considered, at present, as one of the multiple environmental factors involved in the pathogenesis of RA and even it has been suggested that it may be a risk factor.16
The current hypotheses are based on the following principles: RA develops in individuals as a response to an environmental stimulus or to a stimulus experienced by genetically susceptible subjects; the identity and the origin of these stimuli are not fully known, and the different types of stimuli could be important in the subtypes of patients affected by RA.13
PathogenesisThe pathological process that involves the wrist includes: cartilage degradation, ligamentous laxity and synovial thickening with bone erosion. The rheumatoid synovia produces matrix metalloproteinases, enzymes that are capable of degrading all components of the connective tissue. The tumor necrosis factor alpha and multiple interleukins induce the expression of matrix metalloproteinases that, in turn, degrade the components of bone, cartilage and tendons.9
There are important factors that determine the pathological process of wrist deformities in RA: the cartilaginous thinning is caused by the cytochemical effect, which degrades and inhibits the synthesis of new cartilage; and the synovitis of the wrist, that occurs more often in the dorsal than in the palmar aspect, due to the more superficial position of the synovial membrane in the dorsum. The synovial expansion and pannus formation cause bone erosion, particularly in the site of penetration of the vessels into the bone. These erosions generate sharp bone edges that can cause tendon ruptures; in addition, the synovial expansion causes loosening of the intrinsic and extrinsic ligaments of the wrist, which produces wrist supination and ulnar translation. A dorsal or volar carpal intercalated segmental instability may develop, leading to a collapse thereof, where the proximal row of the carpus moves to palmar, ulnar, and in supination, and the carpus leans to the radial side. This deformity of the wrist allows the fingers to drift toward the ulna in the metacarpophalangeal joints that, being with synovitis, had already drift to the ulna by themselves. These 2 phenomena are those which make the fingers move toward the ulnar side, producing the typical deformity of the hand (Fig. 2).
Clinical and radiological aspect of a rheumatic hand. (A) It can be seen the dorsal protrusion of the ulnar head (arrow). (B) In the X-rays can be appreciated the displacement of the carpus to the ulnar side (long arrow), displacement of the metacarpals to the radial side (short arrow) and finally the deviation of the fingers toward the ulnar side with some metacarpophalangeal dislocations.
The progression of the disease leads to a collapse of the carpus secondary to the displacement, ligamentous injuries (such as the radioscapho-lunate ligament) and bone destruction.
The collapse of the carpus explains the “goose-neck” deformities, together with the distention of the flexor and extensor tendons, with a predominance of the interosseous muscle system.
The ulnar aspect of the wrist is usually the first site involved by a significant synovitis; however, the long-term progression is determined by the radiocarpal involvement.9
In the distal radioulnar joint, the ulnar prestyloid recess is a hypervascular area and is commonly affected in RA. The formed synovitis produces a deep excavation in the ulnar surface of the radius, with significant erosion and, in addition, attenuation of the ligaments that stabilize the joint, which leads to a dorsal displacement of the ulnar head, known as caput ulnae (Fig. 2). This degraded and unstable joint causes significant pain to the patient, especially in the prono-supination movements.
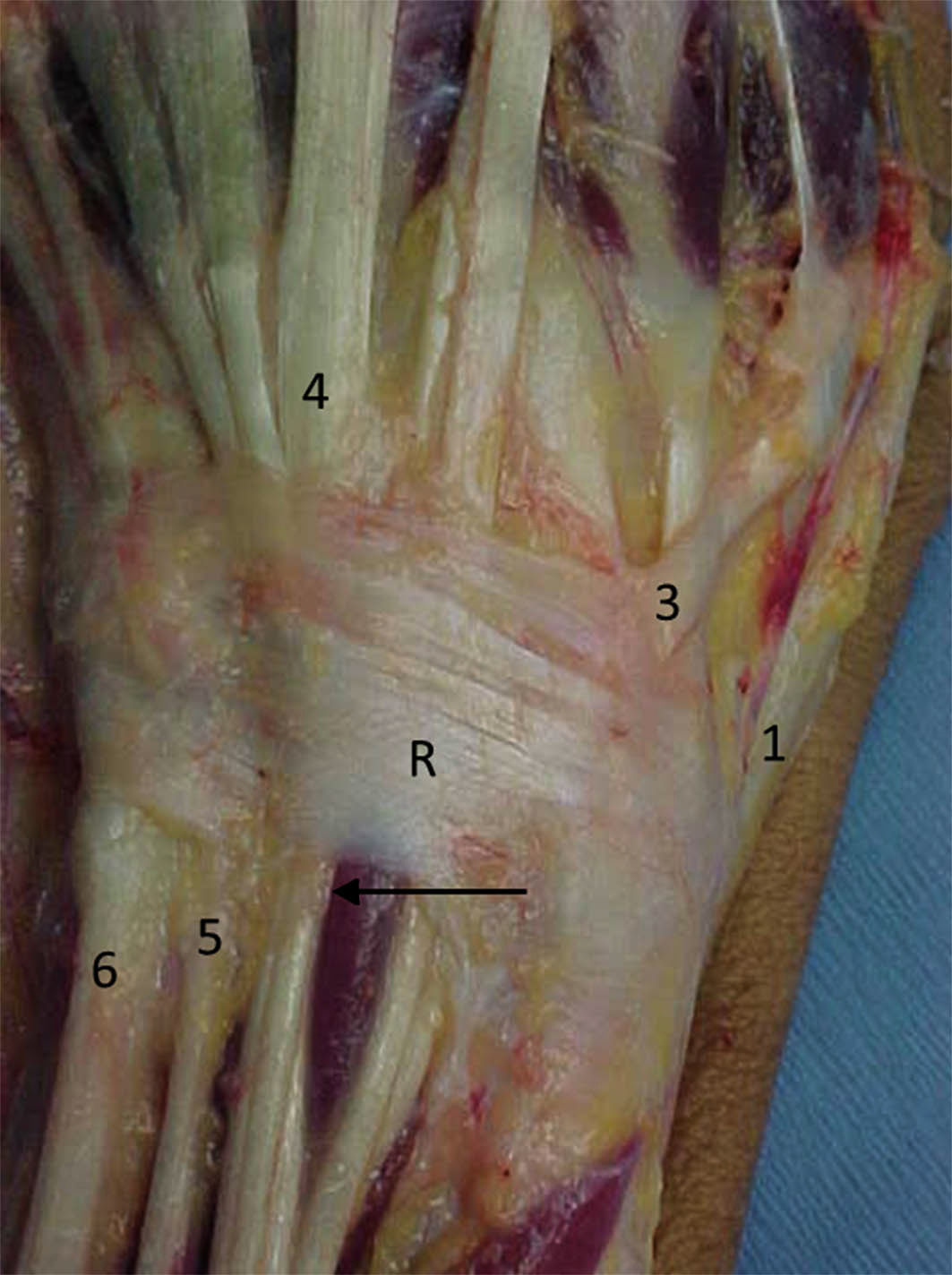
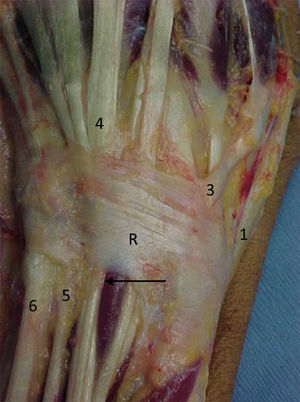
The affection of the wrist is not an isolated event; it is almost always accompanied by a commitment of the flexor and extensor tendons. The tenosynovitis of the extensors is greater where it is surrounded by synovial, which is precisely in their trajectory below the dorsal retinacular ligament. A bulge distal and proximal to it is produced, with a camel's hump shaped pseudotumoral deformity. This tenosynovitis is greater in the 5th, 4th and 3rd extensor compartments, which are the three latest extensor compartments located in the ulnar side of the wrist (of the extensor carpi ulnaris, of the extensor of the fifth finger and of the extensor digitorum communis) (Fig. 3).
Anatomy of the retinaculum of the extensor tendons (R) with its compartments. 1: first extensor compartment; 2: compartment for the long and short radial extensor carpi; 3: for the long extensor of the thumb; 4: for the extensor digitorum communis and for the extensor of the 2nd finger; 5: for the extensor of the 5th finger; 6: for the extensor carpi ulnaris. The synovial that surrounds the tendons is pointed with an arrow.
The synovial proliferation around the tendons, allows the synovial to infiltrate and invade the tendons with production of adhesions. This synovial disease predisposes to the luxation of the extensor tendons and rupture of some of them. These phenomena and the caput ulnae that we already described, predispose, finally, to the rupture of the extensor tendons that run through there, in the first instance the extensor of the 5th finger, and then the extensors of the 4th and 3rd fingers (Fig. 4). The extensor tendons of the radial edge have less risk of rupture.
Flexor tenosynovitis produces painful morning stiffness with decrease of the active flexion arches, but the passive arches usually remain. On the exploration is easy to appreciate the crepitation of the flexors when palpation is done on the A1 flexor pulley in the palm of the hand and it occasionally produces trigger fingers. A carpal tunnel syndrome can be found because of the flowery tenosynovitis of the flexors within the carpal channel. The ruptures of the flexor tendons are rarer than those of the extensors, but their repair is more delicate and has more complications. These ruptures are due to 2 mechanisms: the proliferation and infiltration of the synovial of the tendons leads to their weakening and adhesion, and the second cause is the attrition of the tendons caused by the bone spicules that have been formed. The most affected tendon is that of the long thumb flexor by osteophytes formed in the radio-scaphoid-trapezium complex.
ImagingThe extent of the damage generated by RA is adequately determined with conventional X-rays of the wrist; anteroposterior and lateral projections can show the bone erosions produced by the synovial proliferation, as well as the formation of geodes, which indicate the development of a synovial pannus with osseous infiltration. When surgical management is considered as an option, is mandatory to know the type of damage and destruction of the wrist.
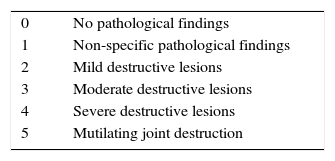
In 1975, Larsen detailed 6 stages to describe radiologically the damage of a joint17,18 (Table 1).
In addition to categorizing the disease, this classification allows to give recommendations for treatment. In stage 1 where there is osteoporosis, with cysts and erosions, the recommended treatment is synovectomy. In stage 2 of the disease, the radiographs show carpal instability; in this case the recommended treatment is stabilization of the soft tissues or partial wrist arthrodesis. In stage 3, the wrist shows an evident destruction and subluxation, and it will probably require a prosthesis (arthroplasty) or arthrodesis. In stage 4 there is great radiocarpal destruction, and the only possibility is a total wrist arthrodesis.
Stanley et al., published the universal classification of the types and stages of the inflammatory arthropathy of the wrist, which aims to integrate multiple published classifications and stages and to condense them in types of slow or advancing progression and in early or late stages.19
Musculoskeletal ultrasonography is a very useful tool in the early stages of the disease, when the clinical manifestations and the radiological findings may not be so evident.20–22 This technique can detect synovial proliferation, joint effusion and bone erosions. The semiquantitative quantification system is currently the method most commonly used for the intra-articular evaluation using Power Doppler Ultrasound; it is not used fully in medical practice due to the limitation of software; however, it easily determines the degrees of synovitis which a joint may exhibit.
MRI allows to improve and define the diagnosis, since it evaluates the synovitis, joint effusion, bone lesions and the status of the tendons; and it also allows to show the locations and the volume of the synovial pannus. It is also a good indicator of the efficiency of medical treatments and of the outcome of synoviorthesis or surgeries.
Non-surgical treatmentIt is important to highlight that the cornerstone of the treatment of RA is pharmacological, which is established by the rheumatologist.
Immobilization with static or dynamic splints is an established procedure in the initial cases of RA, to improve pain, function and to try to prevent deformities. A Cochrane review in 2010, showed that there was no benefit in the use of splints regarding pain and range of motion, but patients did prefer to use them.23
Some authors speak of benefits to reduce pain in short-term immobilizations, especially in an acute phase, not exceeding 4 weeks. In the case of the wrist, a static splint with the wrist in dorsiflexion of 20 to 30 degrees, which provides temporary rest to the wrist is sufficient, providing that the patient is receiving a good pharmacological treatment.
There is also the use of infiltrations of corticosteroids. The available evidence regarding the effectiveness of the local application of glucocorticoids is conflicting, but in general it shows short-term benefits for pain relief.24–26
However, Dean et al.,1 in a systematic review of the literature, analyzed 50 studies and concluded that glucocorticoids have a significant negative effect on the tendon cells in vitro, which includes reduction in cell viability, in cell proliferation and in the synthesis of collagen. The disorganization of the collagen fibers and the necrosis also increase as evidenced by in vivo studies, and the mechanical properties of the tendon are also significantly reduced.27,28
Therefore, the progressive degeneration to rupture, which is an associated complex pathological event, in the long term, with the application of corticosteroids should be seen in the light of a potential short-term pain control and other interventions that affect the resolution of symptoms and that do not increase the risk of having again an injury or rupture should be taken into account.29
Radiosynovectomy is a well-established technique in arthritis as an alternative in the management of synovitis resistant to pharmacological treatments or to local steroid injection, a technique in which an intraarticular injection of small radioactive particles emitting beta particles is applied. It has been widely used in hemophilic arthropathy, being indicated when there are chronic synovitis and recurrent hemarthrosis.30–32
The colloidal solution of rhenium-186 is indicated for the treatment in medium-sized joints like the ankle, shoulder and wrist, since the penetration depth is good for proper irradiation of the synovial membrane, without affecting the subchondral bone.30
There are absolute contraindications for the procedure such as pregnancy, lactation and local infection of the skin; and some relative contraindications such as in patients younger than 20 years, when there is joint instability and extensive destruction of cartilage and subchondral bone.33,34
Radiosynovectomy can be repeated up to 3 times, with a time interval of 3 months, if the first treatment showed an insufficient effect. Repeated treatments are more effective than single treatments.34
Radiosynovectomy is a safe procedure in expert hands, which offers a long-term symptomatic relief, especially in patients with oligoarticular involvement and insufficient response to systemic therapy.
Surgical treatmentA patient with RA who has deformities in the hand is not necessarily a candidate for reconstruction. Many patients with RA may have become accustomed to the disease despite the deformities maintaining an acceptable function. An experienced hand surgeon should strive to understand the needs and expectations of the patient regarding his improvement and must know the surgical options available.
The purposes of the surgeries are: relieve or eliminate pain, improve mobility and restore the stability, protect or repair the flexor and extensor tendons, protect against the degeneration of the joints and, finally, improve the esthetics of the hands.1,2,35–37
The indications for surgical treatment may be influenced by multiple factors, such as the general condition of the patient, his needs and the social and medical environment. There are some rules to take into account when choosing a procedure for the rheumatic patient: the lower limb before the upper limb, correction of the proximal joints before the distal, the painful joint first, prophylaxis versus reconstruction versus salvage, and considering combinations such as elbow-wrist and wrist-metacarpophalangeal joints.36–38
The surgical procedures are targeted to the soft tissues and the joints. These include synovectomies of the extensor tendons, of the flexor tendons, synovectomies of the distal radioulnar, radiocarpal and midcarpal joints, associated or not with repairs of ligaments or capsulorraphies.35–38
For advanced joint commitments, we must resource to distal radioulnar resection arthroplasties or arthrodesis of that joint and the radiocarpal joint, or to total carpal arthrodesis. There is almost no place for carpal prosthesis as there is for metacarpophalangeal or proximal interphalangeal.
SurgeriesSurgeries can be summarized in 2 indications: prophylactic and therapeutic.1,2 The prophylactic surgeries are the synovectomies and the tenosynovectomies.
The therapeutic surgeries are the resection arthroplasties, arthrodesis and joint replacements. The management of tendon ruptures is also considered here.
Prophylactic surgery on the wrist is performed in order to stop or delay the progression of the disease and prevent the complications that may occur.1,2,35 For example, in the synovectomy of the wrist the surgical removal of the synovitis reduces the pressure on the joint, avoids the progressive elongation of the adjacent structures and, it is supposed that it produces some degree of denervation; therefore, its main effect is the relief of pain; however, this relief is often at the expense of the loss of the wrist joint mobility, especially of flexion. To reduce this possibility, arthroscopic synovectomy may be considered. Adolfsson39,40 describes as an indication for arthroscopic synovectomy the patients with RA, in whom the pharmacological therapy has not been well tolerated or enough effective to reduce the synovitis, who have had at least one intraarticular injection of corticosteroids and those with persistent synovitis for more than 6 months. He recommends to use this procedure only in patients with radiographic changes from 0 to 2 according to the Larsen index.
Arthroscopic synovectomy has demonstrated to reduce pain, improve the range of motion, functionality and grip strength in the short and medium term follow-ups, in wrists with RA without radiographic changes or with mild radiographic changes.39,40
The indication for prophylactic synovectomy in the wrist is more precise when a reconstruction of the distal radioulnar joint will be done or in a persistent and painful tenosynovitis of the extensors; in this case is preferable an open synovectomy of the wrist.36,41
Synovectomy of the flexor and extensor tendonsThere are two main indications for the flexors synovectomy alone, the first is when a persistent carpal tunnel syndrome is present, after conservative treatment and infiltration of the carpal tunnel; and the second are the tendon ruptures, where the resection of osseous prominences is mandatory, since it prevents further damage to the tendon.
In the first case, the release of the carpal tunnel syndrome and flexor tenosynovectomy should be performed. As mentioned above, the flexor tendon ruptures involve initially the long flexor of the thumb, then the deep flexor of the second finger and so on, that is, it runs from radial to ulnar, in opposition to the extensor tendons, where the rupture occurs first in those of the ulnar side and then in those which are in the radial side. The rupture of the long flexor of the thumb can be silent and not be noticed by the patient.42
In the case of ruptures, there are 3 options: to make a repair through a tendon graft, a tendon transfer and finally, an arthrodesis of the interphalangeal joint of the thumb. In young patients with greater functional need, the 2 latter surgeries are a good option.36–38,42
If there is involvement of other fingers, you can play with these 3 options.
It is possible to perform in the same surgical act the decompression of the carpal tunnel and the surgery of the back of the wrist.
In general, the commitment of the extensor tendons is more noticeable by the patient.
Treatment of the distal radioulnar jointThe only presence of deformity is not necessarily a surgical indication. The combination of pain, functional alteration and the presence of a large caput ulnae (dorsal protrusion of the ulnar head) justify the indication of surgical treatment. A more aggressive management is recommended in cases where a tendon rupture occurs.
The basic principles include: synovectomy of the distal radioulnar joint, tenosynovectomy of the extensors, partial or total resection of the distal end of the ulna (technique of Darrach) with stabilization of the remaining ulna and stabilization of the radiocarpal joint, if necessary.
In the majority of cases, the treatment of the radiocarpal joint, the extensor tendons and the distal radioulnar joint, is performed during the same surgical act. The general outcomes when wrist synovectomy is performed combined with the resection of the ulnar head show good to excellent results in terms of pain relief and a minimal incidence or recurrent synovitis and residual instability of the distal ulnar stump.36,43
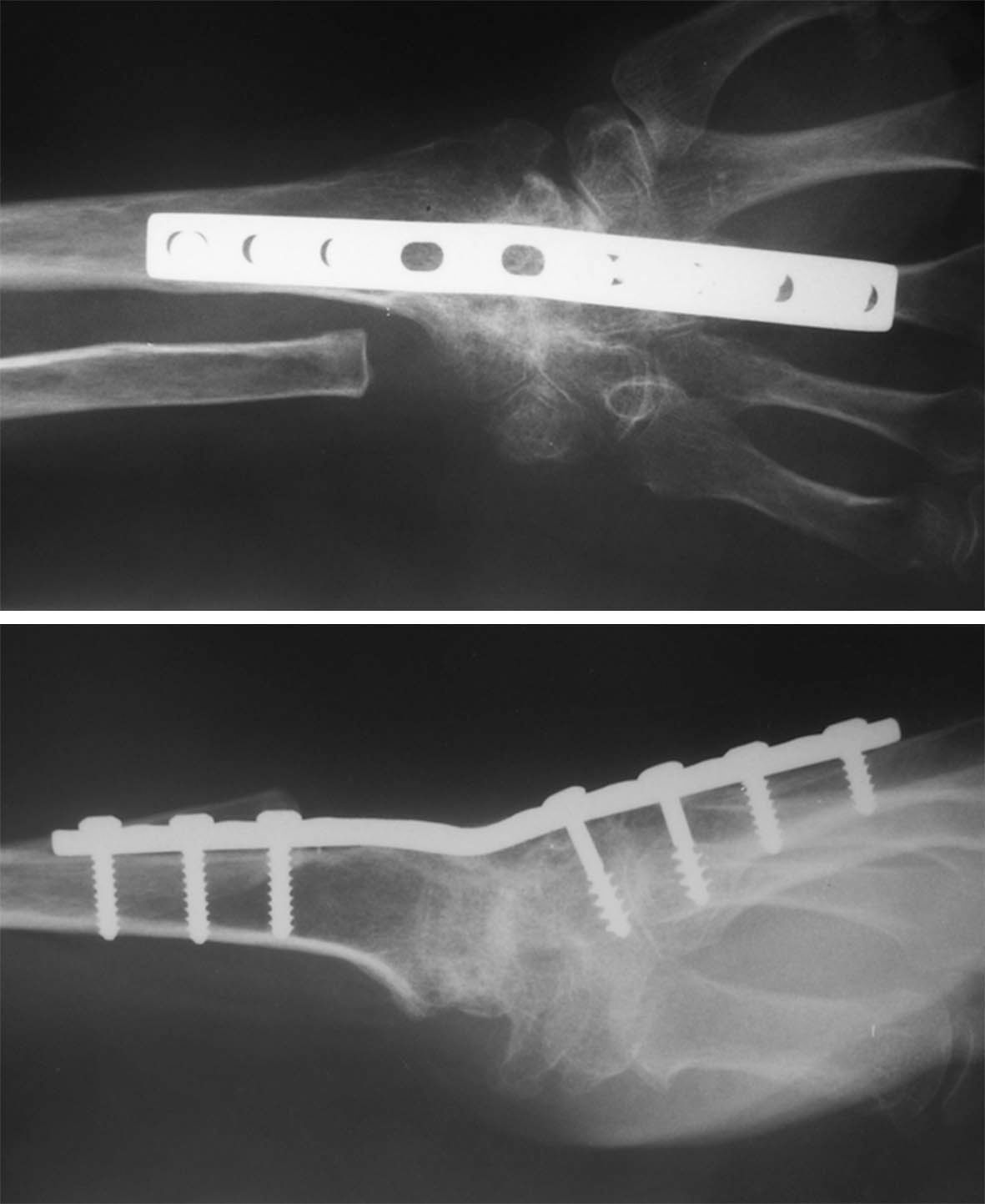
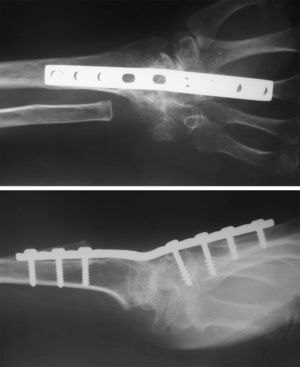
The Sauvé–Kapandji procedure (arthrodesis in the distal radioulnar joint with pseudoarticulation in the diaphysis of the ulna), preserves the stabilizing elements of the ulnar aspect of the wrist, maintaining the pronation-supination range of motion (Figs. 5 and 6). It is a procedure which has shown good results over time,36,43–45 however, once the ulnar translation starts, it is unlikely that this surgical procedure would stop its progression, requiring then a stabilization of the radiocarpal joint.
Clinical outcome of the patient in Fig. 4, full pronation and supination without pain.
With the improvement in the medical treatment of the disease, the unique indications for a synovectomy of the wrist have decreased.36–38,46 A good pharmacological treatment can slow the damage of the joint, leaving some indications for synovectomy when there is persistent synovitis despite a well performed medical treatment or in cases of frequent recurrence of synovitis. Synovectomy is also performed when it is done in combination with other surgeries such as extensors synovectomy or when treating the distal radioulnar joint.
The experience shows in general that the inflammatory process in the wrist is reduced, but over time the process can return, especially when it is a systemic affection with involvement of multiple joints.
When a joint is already deteriorated, with pain that leads to functional loss, arthrodesis or replacement arthroplasty should be considered.47,48
Long-term follow-up studies have demonstrated that more than 90% of the wrists with RA become symptomatic and the limited carpal arthrodesis are among the options of treatment to control pain and preserve function.
The indications for partial wrist fusion include patients with localized disease, mainly, in the radiocarpal joint without affecting the midcarpal joint. The most commonly used partial arthrodeses are the radio-lunate arthrodesis and the radioscapho-lunate arthrodesis. The contraindications for partial arthrodesis are the presence of midcarpal osteoarthritis and a rapidly progressive inflammatory process. The obvious advantage of the partial arthrodesis of the wrist is that it preserves some mobility in the wrist, however, in the advanced disease remain only two options: total wrist arthrodesis and total wrist arthroplasty.37,38
Arthrodesis is a predictable procedure for pain relief in patients with RA, which has been used for a long time with great acceptability by the surgeon and the patient. Experience has shown that patients who have received a fusion or arthrodesis of the wrist have improved their function in that they are able to have a more effective grip and improvement in strength, and only some little difficulties are found (Fig. 7). The arthrodesis rarely need to be revised, perhaps in the rare cases of lack of union or consolidation, which indeed, is common with a total wrist arthroplasty.
The total wrist arthroplasty was popularized by Swanson in 1960. It was a silicon implant that showed promising short-term results; however, mechanical failures and severe inflammatory reactions appeared and led to its disuse. Based on this, different total wrist implants have been proposed and designed.49–51
In a systematic review, the results for the total wrist fusion were comparable and, possibly, better than those of the total wrist arthroplasty in patients with RA.52
In our opinion, and of many others, the arthrodesis of the wrist is an excellent procedure, which has provided long-term benefits in many patients with RA and is preferable than a total wrist arthroplasty.
ConclusionThe wrist is frequently affected in patients with RA. Pharmacological treatment has proven to be the best alternative for the improvement of the inflammatory phenomenon and therefore, of the joint destruction and it also reduces the need for surgery.
The surgical treatment options are varied and range in accordance with the synovitis and the degree of joint destruction. It is not uncommon to find damage of the extensor and flexor tendons with ruptures that require surgery.
The radioulnar joint is frequently affected, requiring surgeries such as distal radioulnar arthrodesis (Sauvé–Kapandji) or resection of the distal end of the ulna (Darrach). When there is an advanced involvement of the wrist joint, a total wrist arthrodesis or arthroplasty may be required.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Vergara-Amador E, Rojas A. La muñeca reumatoidea. Aspectos esenciales en el tratamiento. Rev Colomb Reumatol. 2016;23:24–33.