We report retrospectively a series of four cases involving the successful use of the recently described parascapular sub-iliocostalis plane block (PSIP), for lateral-posterior rib fractures.
The efficacy of the PSIP block may potentially depend on different mechanisms of action: (1) direct action in the fracture site by craniocaudal myofascial spread underneath the erector spinae muscle (ESM); (2) spread to deep layers through tissue disruption caused by trauma, to reach the proximal intercostal nerves; (3) medial spread below the ESM, to reach the posterior spinal nerves; and (4) lateral spread in the sub-serratus (SS) plane to reach the lateral cutaneous branches of the intercostal nerves; while avoiding significant negative hemodynamic effects and other possible complications associated to other techniques leading that the PSIP may be considered an alternative in some clinical scenarios to the erector spinae plane block or the paravertebral block.
Presentamos retrospectivamente una serie de 4 casos en los que se utilizó con éxito el bloqueo paraescapular del plano subiliocostal (PSIP), descrito recientemente, para fracturas costales laterales-posteriores.
La eficacia del bloqueo PSIP puede depender potencialmente de diferentes mecanismos de acción: (1) acción directa en las fractura por la extensión miofascial craneocaudal por debajo del músculo erector de la columna, (2) diseminación a capas profundas a través de la disrupción tisular causada por el traumatismo, para alcanzar los nervios intercostales proximales, (3) extensión medial por debajo del músculo erector de la columna, para alcanzar los nervios espinales posteriores y (4) extensión lateral en el plano subserrato para alcanzar las ramas cutáneas laterales de los nervios intercostales, evitando al mismo tiempo efectos hemodinámicos negativos y otras posibles complicaciones asociados a otras técnicas, lo que hace que el bloqueo PSIP pueda considerarse en algunos escenarios clínicos una alternativa al bloqueo del plano erector de la columna vertebral o al bloqueo paravertebral.
Herein, we describe a series of cases involving an alternative analgesic technique, the parascapular sub-iliocostalis plane (PSIP) block for patients suffering from posterior rib fractures.
The PSIP block was previously described only as single case report1 being this report the first case series in posterior rib fracture patients. The PSIP block may be an alternative whenever contraindications for erector spinae plane (ESP) block or paravertebral block (PVB) are present, due to its less action in the anterior spinal nerves or to its less risk of inadvertent neuraxial involvement.1
To date there are no studies, neither cadaveric nor clinical, related to mechanism of action and local anesthetic (LA) spread of the PSIP block.
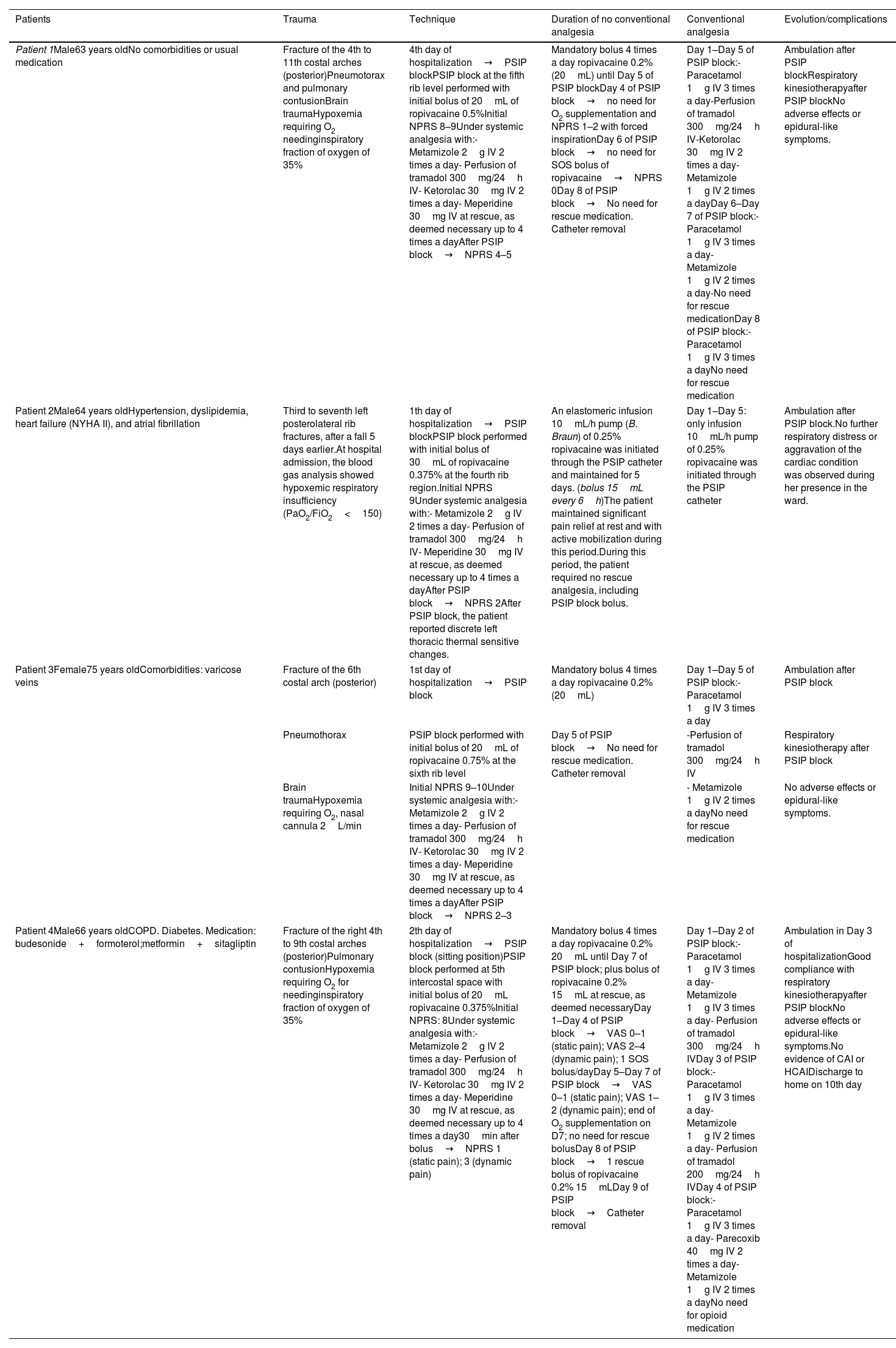
Materials and methodsDetails about the patients and about patients’ condition, comorbidities, analgesia approach, clinical scenario, progression of the case and outcome are described in Table 1.
Serie of cases of PSIP block.
| Patients | Trauma | Technique | Duration of no conventional analgesia | Conventional analgesia | Evolution/complications |
|---|---|---|---|---|---|
| Patient 1Male63 years oldNo comorbidities or usual medication | Fracture of the 4th to 11th costal arches (posterior)Pneumotorax and pulmonary contusionBrain traumaHypoxemia requiring O2 needinginspiratory fraction of oxygen of 35% | 4th day of hospitalization→PSIP blockPSIP block at the fifth rib level performed with initial bolus of 20mL of ropivacaine 0.5%Initial NPRS 8–9Under systemic analgesia with:- Metamizole 2g IV 2 times a day- Perfusion of tramadol 300mg/24h IV- Ketorolac 30mg IV 2 times a day- Meperidine 30mg IV at rescue, as deemed necessary up to 4 times a dayAfter PSIP block→NPRS 4–5 | Mandatory bolus 4 times a day ropivacaine 0.2% (20mL) until Day 5 of PSIP blockDay 4 of PSIP block→no need for O2 supplementation and NPRS 1–2 with forced inspirationDay 6 of PSIP block→no need for SOS bolus of ropivacaine→NPRS 0Day 8 of PSIP block→No need for rescue medication. Catheter removal | Day 1–Day 5 of PSIP block:-Paracetamol 1g IV 3 times a day-Perfusion of tramadol 300mg/24h IV-Ketorolac 30mg IV 2 times a day-Metamizole 1g IV 2 times a dayDay 6–Day 7 of PSIP block:-Paracetamol 1g IV 3 times a day-Metamizole 1g IV 2 times a day-No need for rescue medicationDay 8 of PSIP block:-Paracetamol 1g IV 3 times a dayNo need for rescue medication | Ambulation after PSIP blockRespiratory kinesiotherapyafter PSIP blockNo adverse effects or epidural-like symptoms. |
| Patient 2Male64 years oldHypertension, dyslipidemia, heart failure (NYHA II), and atrial fibrillation | Third to seventh left posterolateral rib fractures, after a fall 5 days earlier.At hospital admission, the blood gas analysis showed hypoxemic respiratory insufficiency (PaO2/FiO2<150) | 1th day of hospitalization→PSIP blockPSIP block performed with initial bolus of 30mL of ropivacaine 0.375% at the fourth rib region.Initial NPRS 9Under systemic analgesia with:- Metamizole 2g IV 2 times a day- Perfusion of tramadol 300mg/24h IV- Meperidine 30mg IV at rescue, as deemed necessary up to 4 times a dayAfter PSIP block→NPRS 2After PSIP block, the patient reported discrete left thoracic thermal sensitive changes. | An elastomeric infusion 10mL/h pump (B. Braun) of 0.25% ropivacaine was initiated through the PSIP catheter and maintained for 5 days. (bolus 15mL every 6h)The patient maintained significant pain relief at rest and with active mobilization during this period.During this period, the patient required no rescue analgesia, including PSIP block bolus. | Day 1–Day 5: only infusion 10mL/h pump of 0.25% ropivacaine was initiated through the PSIP catheter | Ambulation after PSIP block.No further respiratory distress or aggravation of the cardiac condition was observed during her presence in the ward. |
| Patient 3Female75 years oldComorbidities: varicose veins | Fracture of the 6th costal arch (posterior) | 1st day of hospitalization→PSIP block | Mandatory bolus 4 times a day ropivacaine 0.2% (20mL) | Day 1–Day 5 of PSIP block:-Paracetamol 1g IV 3 times a day | Ambulation after PSIP block |
| Pneumothorax | PSIP block performed with initial bolus of 20mL of ropivacaine 0.75% at the sixth rib level | Day 5 of PSIP block→No need for rescue medication. Catheter removal | -Perfusion of tramadol 300mg/24h IV | Respiratory kinesiotherapy after PSIP block | |
| Brain traumaHypoxemia requiring O2, nasal cannula 2L/min | Initial NPRS 9–10Under systemic analgesia with:- Metamizole 2g IV 2 times a day- Perfusion of tramadol 300mg/24h IV- Ketorolac 30mg IV 2 times a day- Meperidine 30mg IV at rescue, as deemed necessary up to 4 times a dayAfter PSIP block→NPRS 2–3 | - Metamizole 1g IV 2 times a dayNo need for rescue medication | No adverse effects or epidural-like symptoms. | ||
| Patient 4Male66 years oldCOPD. Diabetes. Medication: budesonide+formoterol;metformin+sitagliptin | Fracture of the right 4th to 9th costal arches (posterior)Pulmonary contusionHypoxemia requiring O2 for needinginspiratory fraction of oxygen of 35% | 2th day of hospitalization→PSIP block (sitting position)PSIP block performed at 5th intercostal space with initial bolus of 20mL ropivacaine 0.375%Initial NPRS: 8Under systemic analgesia with:- Metamizole 2g IV 2 times a day- Perfusion of tramadol 300mg/24h IV- Ketorolac 30mg IV 2 times a day- Meperidine 30mg IV at rescue, as deemed necessary up to 4 times a day30min after bolus→NPRS 1 (static pain); 3 (dynamic pain) | Mandatory bolus 4 times a day ropivacaine 0.2% 20mL until Day 7 of PSIP block; plus bolus of ropivacaine 0.2% 15mL at rescue, as deemed necessaryDay 1–Day 4 of PSIP block→VAS 0–1 (static pain); VAS 2–4 (dynamic pain); 1 SOS bolus/dayDay 5–Day 7 of PSIP block→VAS 0–1 (static pain); VAS 1–2 (dynamic pain); end of O2 supplementation on D7; no need for rescue bolusDay 8 of PSIP block→1 rescue bolus of ropivacaine 0.2% 15mLDay 9 of PSIP block→Catheter removal | Day 1–Day 2 of PSIP block:- Paracetamol 1g IV 3 times a day- Metamizole 1g IV 3 times a day- Perfusion of tramadol 300mg/24h IVDay 3 of PSIP block:- Paracetamol 1g IV 3 times a day- Metamizole 1g IV 2 times a day- Perfusion of tramadol 200mg/24h IVDay 4 of PSIP block:- Paracetamol 1g IV 3 times a day- Parecoxib 40mg IV 2 times a day- Metamizole 1g IV 2 times a dayNo need for opioid medication | Ambulation in Day 3 of hospitalizationGood compliance with respiratory kinesiotherapyafter PSIP blockNo adverse effects or epidural-like symptoms.No evidence of CAI or HCAIDischarge to home on 10th day |
Abbreviations: PSIP: parascapular sub-iliocostalis plane; NPRS: Numeric Pain Rating Scale; IV: intravenously; NYHA: New York Heart Association; COPD: chronic obstructive pulmonary disease; CAI: community acquired infection; HCAI: healthcare-associated infection.
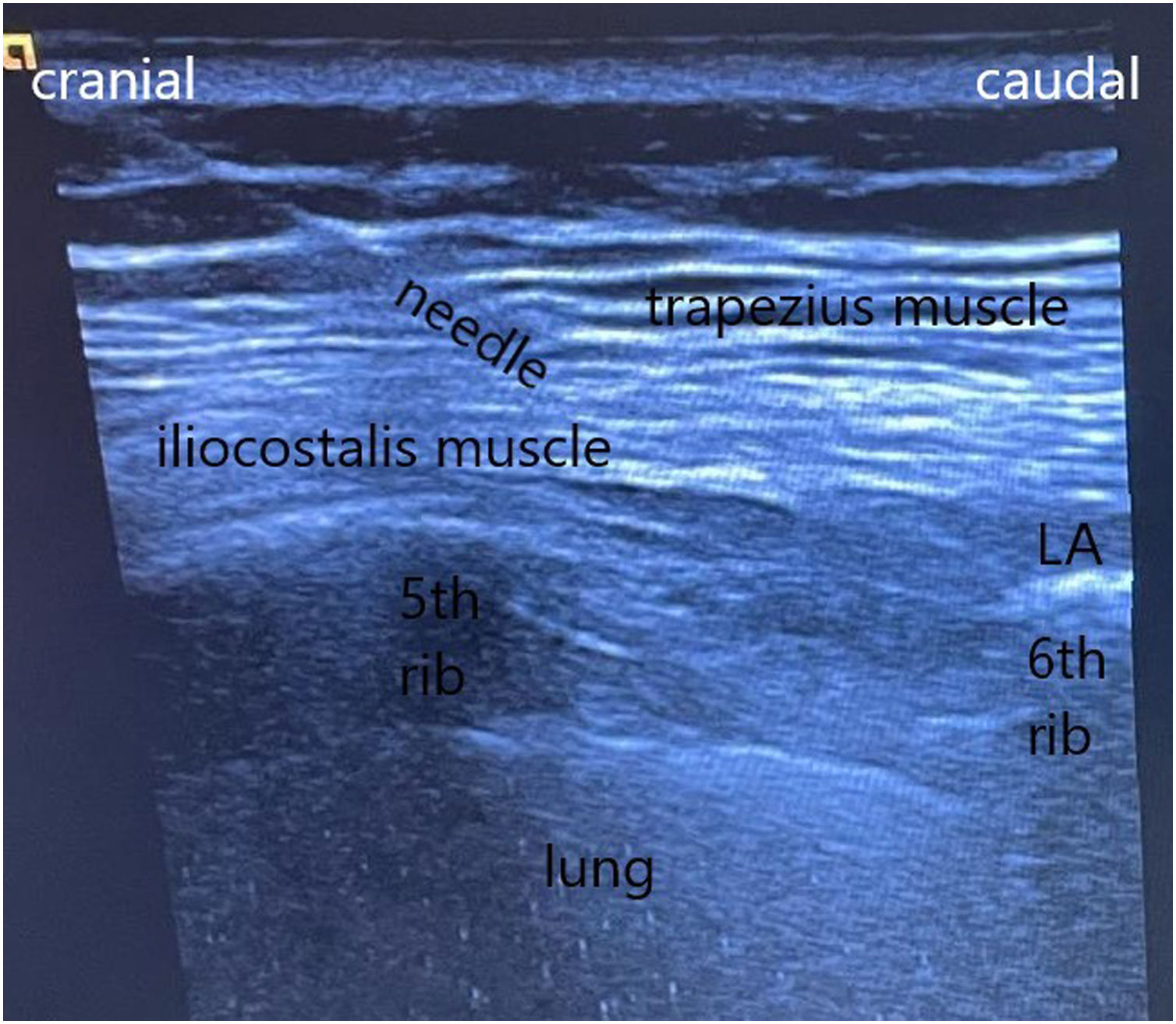
The PSIP blocks were performed with the patient lateral decubitus under American Society of Anesthesiologists standard monitoring. A high-frequency linear ultrasound probe (Acuson 300; Siemens, Munich, Germany) was placed in a parasagittal plane orientation to 2cm from the medial scapular border at the level of the edge of the scapula spine under sterile conditions (between the fourth rib level and sixth rib level depending on the location of the posterior rib fractures) (Fig. 1). The trapezius, rhomboid major, iliocostal, and intercostal muscles were visualized from the superficial to deep muscular layers cranial to 5th rib; distal to 5th rib only trapezius and iliocostalis muscles are observed (Fig. 1). A sonovisible 100mm 18G needle (Contiplex S ultra; B. Braun, Melsungen, Germany) was inserted with a cranial to caudal orientation using an in-plane technique and advanced in the iliocostal-intercostal myofascial plane in the vicinity of the rib (Fig. 1). The needle location was confirmed with a 2mL saline solution, after which ropivacaine (Fresenius Kabi Pharma, Santiago de Besteiros, Portugal) was administered (Table 1). A catheter was then inserted 6cm beyond the needle tip and tunneled under the skin. No sensitive alterations were noted in all the patients.
Description of the parascapular sub-iliocostalis plane block performed in patient 3.
With the patient in a lateral position, with both arms along the body, a high-frequency linear ultrasound probe was placed with a parasagittal orientation, immediately adjacent to the medial scapular border at the level of the edge of the sixth rib level. Identification of the lateral border of the iliocostalis muscle and performance of the parascapular sub-iliocostalis plane block. The tendinous insertion of the ILCM at the rib is in the superolateral direction (it should not be confounded with the insertion of the levatore costarum muscles whose insertion is in the inferior-lateral direction). The rhomboid major or minor muscle and the posterior superior serratus muscles are observed between the trapezius muscle and the iliocostalis muscles at upper levels. Abbreviation: LA, local anesthetic spreading.
During this period, all the patients maintained intravenous conventional analgesia. The patient remained under continuous monitoring of the vital signs in an intermediated care unit.
DiscussionThe PVB and ESP block may promote a central sympathetic blockade that can be associated with significant hypotension and bradycardia, affect ventricular function, and decrease cardiac output, which can increase pulmonary edema and result in worsened dyspnea. Additionally, significant chest wall weakness can arise from these techniques, affecting thoracic expansion and, indirectly, venous return.1–5
These features may put patients at risk of aggravation of preexisting cardiovascular disease, such as in patient 1 case, or aggravate respiratory distress resulting from concomitant pulmonary contusion, post-traumatic atelectasis, undrained pneumothorax, diaphragmatic paralysis or rupture or when there is a preexisting lung disease, such as in the case of patients 1–4, due to the neuromuscular block that may arise from the ESP block or PVB (the thoracic expansion is less likely to be affected with the PSIP block mainly due to the reduced risk of bilateral block and to the limited action of the PISP block on the spinal nerves in opposition to the ESP block or PVB).1,10
The ESP block and the PVB may be hazardous whenever concomitant brain trauma is present, such as in the case of patient 1 and 3. The presence of sepsis or hemostasis alterations may turn out preferable the placement of a catheter away of the vicinity or the neuraxial region.10
Indeed, some studies failed to demonstrate that the ESP block spreads to the paravertebral space,6 whereas others concluded that, beyond the paravertebral compartment, epidural spread is the main component of its analgesic properties.4
It has been reported a circumferential epidural spread of LA after an ESP block, which can worsen cardiac condition in high-risk patients.2
Potentially, the PSIP block would provoke less epidural-like effects compared with the ESP block due to a lateral injection point, which lowers the risk of massive epidural/paravertebral spread or bilateral block.1,10 On the other hand, the epidural spread of LA epidurally or the inadvertent dural puncture or direct epidural injection may affect the intracranial pressure when an ESP or PVB are used.10
Rhomboid intercostal blocks have been successfully performed in patients with multiple lateral-posterior rib fractures and other causes of chest wall pain.7
However, in the study by Elsharkawy et al., the staining stopped at the lateral edge of the ESM (iliocostalis muscle) in one-third of the specimens, and in cadavers, no staining was observed to the erector spinae muscle (ESM).7
Therefore, this block may have limited action at the fracture sites medial to the lateral border of the iliocostalis muscle (ILCM), as this muscle may represent an obstacle for the LA present in the sub-rhomboid plane or lateral to the ILCM, preventing its spread to the fractured rib plane below the ESM.
The eventual criticism to this novel technique may be hypothetically related to its nomenclature, nevertheless an Expert Consensus in 2021 (ASRA-ESRA Delphi Consensus)8 stablished the retrolaminar (RL) block as an independent entity from the ESP block: in the RL block the injection is done between the laminae and the ESM, in the latter the injection is done between the transverse process and the ESM; on the other hand, in the PSIP block, the injection is done between the most lateral component of the ESM and the ribs, which lead to completely different properties in terms of dispersion pattern, mode of action, contraindications, benefits and complications comparing to the RL and ESP blocks. Of note, the PSIP block is the only block of this group that does not have any component of the vertebrae as a sono-anatomical reference, which makes it a complete novel technique, as the retrolaminar block is when compared to the ESP block.1,10
The PSIP block has also potential benefit for thoracic spine surgery or trauma, as it was shown in a recent report by Almeida et al.,9 due to its action in the posterior rami of the spinal nerves, with less direct action in the anterior spinal nerves, as such, when concomitant thoracic spinal fractures are present the PSIP block can be an interesting alternative to limit neuroaxial LA spread because meningeal membranes or dura-mater can be disrupted, which can be hazardous and complicate neurological check when the ESP or PVB are used.
In the PSIP block the catheter is placed underneath the ILCM, enhancing the craniocaudal LA spread across the longitudinal myofascial sub-ILCM plane and the deeper spread of LA through the disrupted tissue. The observed significant reduction of pain with motion may be related to the LA spread to deep intercostal layers in the fracture sites, direct infiltration of the fractured bone, and action in the proximal intercostal nerves.1
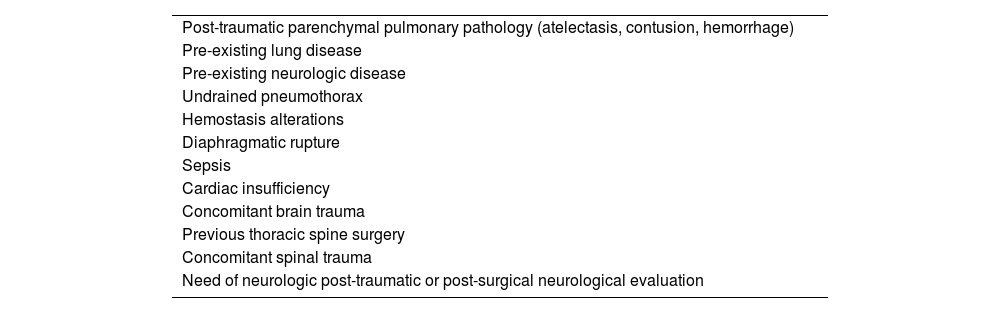
The additional spread along the deep intercostal layers is likely, but LA would not reach easily the paravertebral space. The PSIP block could also spread medially below the ESM to block mainly the posterior spinal nerves, contributing to vertebrae analgesia as it was described by Almeida et al. in a case of thoracic spine fixation surgery.9 It should be emphasized than if concomitant anterior-lateral fractures are present the PSIP block should not be a reliable alternative to the ESP block or the PVB. The clinical scenarios in which the PSIP block, despite lacking significant direct action in the ventral spinal rami, could be preferable to the ESP block or PVB for posterior rib fractures, are expressed in Table 2.
Patients’ conditions in which the PSIP block could be less hazardous than the ESP block or the PVB for posterior rib fractures analgesia.
| Post-traumatic parenchymal pulmonary pathology (atelectasis, contusion, hemorrhage) |
| Pre-existing lung disease |
| Pre-existing neurologic disease |
| Undrained pneumothorax |
| Hemostasis alterations |
| Diaphragmatic rupture |
| Sepsis |
| Cardiac insufficiency |
| Concomitant brain trauma |
| Previous thoracic spine surgery |
| Concomitant spinal trauma |
| Need of neurologic post-traumatic or post-surgical neurological evaluation |
The PSIP block has now revealed its potential in the small series of cases, further large studies are necessary to confirm our results, but we are very convinced of its merits based on our experience.
FundingNone declared.
Conflicts of interestThe authors declare that they have no conflicts of interest.