The SARS-CoV-2 pandemic has been characterized by a steady accumulation of cases of acute respiratory distress syndrome (ARDS) in intensive care units (ICU).1 In the literature, the combined use of high-flow nasal cannula (HFNC) and prone positioning (PP) has only been described in isolated cases or small series.2,3
We briefly describe and discuss 2 patients with ARDS who were treated with the combination of both therapies in our ICU. The first case was a 47-year-old, hypertensive, obese man admitted to the ICU with a week-long history of progressive SARS-CoV-2 pneumonia. On admission, peripheral blood oxygen (SpO2) measured by pulse oximetry was 88%–90%, with well-tolerated tachypnoea and no sensation of dyspnoea at rest. The second case was a 74-year-old hypertensive man admitted to the ICU with SpO2 92% with Ventimask® at FiO2 50% (15 L) due to SARS-CoV-2 pneumonia.
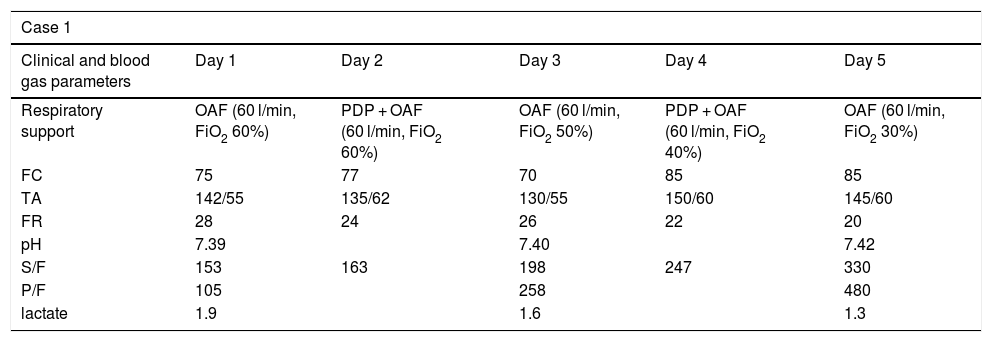
In both situations, progressive respiratory impairment and increased tachypnoea prompted us to start HFNC therapy at 60 l/min and an FiO2 of 60%. Despite initial improvement, neither symptoms nor blood oxygen levels improved over the following hours, so we decided to pronate the patients and combine spontaneous ventilation with HFNC. This produced an immediate change in respiratory rate and blood gas parameters, as shown in Table 1. Neither patient received sedation, and over the following 3 days both were pronated intermittently (morning and afternoon) for between 3 and 8 h per day, depending on the patient's tolerance. Oxygen supply decreased progressively during their ICU stay. The first patient remained in the ICU for 7 days, and the second for 5 days.
Evolution of parameters during the first 5 days in the ICU in which combination HFNC and PP therapy was administered.
| Case 1 | |||||
|---|---|---|---|---|---|
| Clinical and blood gas parameters | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 |
| Respiratory support | OAF (60 l/min, FiO2 60%) | PDP + OAF (60 l/min, FiO2 60%) | OAF (60 l/min, FiO2 50%) | PDP + OAF (60 l/min, FiO2 40%) | OAF (60 l/min, FiO2 30%) |
| FC | 75 | 77 | 70 | 85 | 85 |
| TA | 142/55 | 135/62 | 130/55 | 150/60 | 145/60 |
| FR | 28 | 24 | 26 | 22 | 20 |
| pH | 7.39 | 7.40 | 7.42 | ||
| S/F | 153 | 163 | 198 | 247 | 330 |
| P/F | 105 | 258 | 480 | ||
| lactate | 1.9 | 1.6 | 1.3 | ||
| Case 2 | |||||
|---|---|---|---|---|---|
| Clinical and blood gas parameters | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 |
| Respiratory support | HFO (60 l/min, FiO2 60%) | PP + HFO (60 l/min, FiO2 60%) | PP + HFO (60 l/min, FiO2 60%) | HFO (60 l/min, FiO2 25%) | |
| HR | 72 | 65 | 64 | 70 | |
| BP | 120/62 | 128/58 | 132/55 | 125/55 | |
| RR | 26 | 22 | 26 | 20 | |
| pH | 7.5 | 7.47 | 7.46 | ||
| S/F | 156 | 162.5 | 164 | 412 | |
| P/F | 106 | 181 | |||
| lactate | 1 | 1.2 | 1 | ||
BP: blood pressure; HFO: high-flow oxygen therapy; HR: heart rate; P/F: PaO2/Fraction of inspired oxygen ratio; PP: prone positioning; RR: respiratory rate; S/F: SpO2/Fraction of inspired oxygen ratio.
Evidence emerging several years ago showed that non-invasive HFNC increases end-expiratory lung impedance in healthy subjects, suggesting that it also increases functional residual capacity. This increase is significantly greater in ventral lung regions when the subject is breathing in the supine position, and more homogeneous when breathing in PP.4
Based on these potentially beneficial mechanisms, a recent prospective observational study concluded that early PP with HFNC, particularly in patients with moderate ARDS and baseline SpO2 > 95%, can help prevent intubation. In this study, PP was well tolerated and improved the efficacy on PaO2/FiO2 of the different support strategies studied.3
In this regard, the PP protocol in awake patients with SARS-CoV-2 pneumonia that significantly improved oxygenation and pulmonary heterogeneity showed a Jiangsu rate of invasive mechanical ventilation below 1%,5 one of the best reported.
It is important to mention that when performing this therapy, all the equipment needed for advanced airway management must be prepared in advance. In addition, there is currently no ideal length of time for PP, but the main consideration is to avoid patient fatigue.
At present there is insufficient evidence to recommend prone positioning in patients under spontaneous ventilation, and it could theoretically put patients at risk by, for example, delaying the start of mechanical ventilation. On the other hand, there is no evidence to discredit its use.
Please cite this article as: González-Castro A, Escudero-Acha P, Arnaiz F, Ferrer D. Oxigenoterapia de alto flujo y posición de prono con respiración espontánea en neumonía por SARS-CoV-2. Rev Esp Anestesiol Reanim. 2020. https://doi.org/10.1016/j.redar.2020.05.014