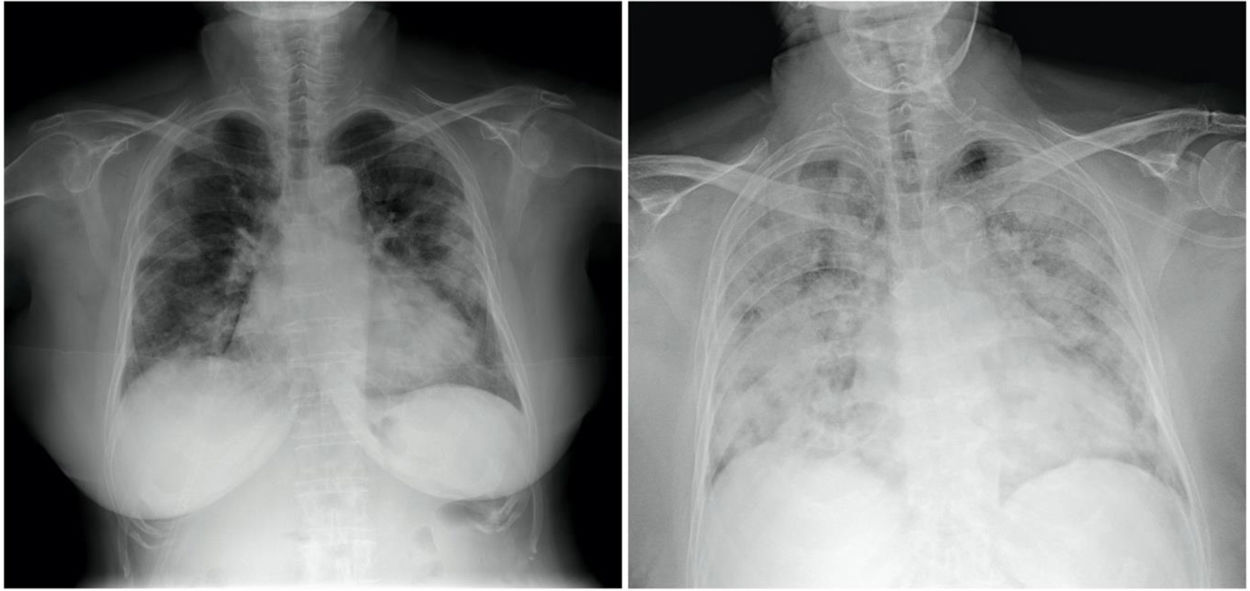
A 77-year-old patient weighing 70 kg and with hypertension and dyslipidaemia was admitted due to bilateral pneumonia (Fig. 1), with PCR positive for SARS-CoV-2. He was transferred to the Intensive Care Unit (ICU) due to refractory hypoxaemia that required orotracheal intubation and mechanic ventilation.
On the left, posteroanterior chest radiograph on admission, showing bilateral peripheral consolidations in upper, middle and lower fields, with no pleural effusion - findings suggestive of infection by COVID-19.
On the right, anteroposterior chest X-ray in decubitus 3 days after admission, prior to orotracheal intubation, showing radiological evolution of the disease.
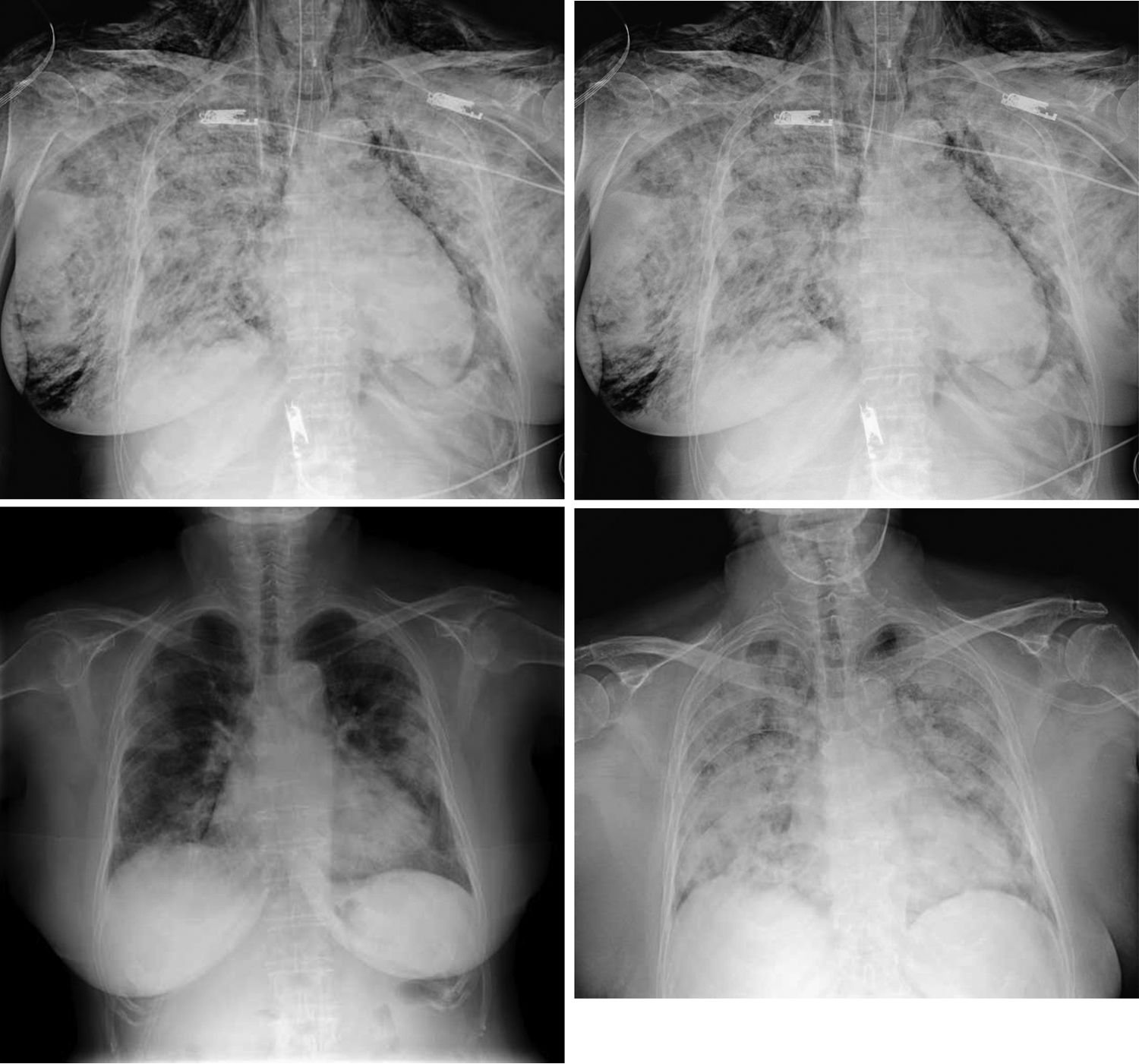
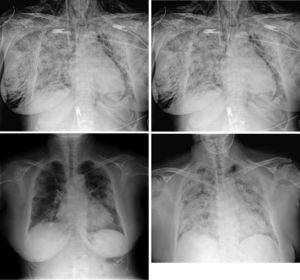
Two hours later, he presented blood oxygen desaturation with significant subcutaneous emphysema, mainly in the cervical spine and right hemithorax, with crepitus during palpation (Fig. 2), that could have been secondary to traumatic orotracheal intubation associated with bag mask ventilation during his transfer to the ICU. The patient presented multiple organ failure, and died.
Anteroposterior chest X-ray, in decubitus. Extensive subcutaneous emphysema that extends through the supraclavicular fossae, shoulders, dissects the left pectoral muscle and the right breast. Note the presence of air in the left paratracheal line at the mediastinal level, which surrounds the aortic knob and to a lesser extent the left cardiac margin - findings compatible with pneumomediastinum, with no associated pneumothorax.
Please cite this article as: Amador Penco FB, Villalonga D, Hermoso Martínez JI, Smith Vielma LG. Enfisema subcutáneo masivo en paciente con infección por SARS-CoV-2. Rev Esp Anestesiol Reanim. 2020. https://doi.org/10.1016/j.redar.2020.06.011