Third molar extraction is a common procedure and it is rarely associated with complications. One complication that may be associated with this procedure is displacement of the tooth into the infratemporal fossa, an anatomical structure that contains the temporalis muscle, medial and lateral pterygoid muscles, the pterygoid plexus, the maxillary artery and its branches, the mandibular nerve and its branches, and the chorda tympani. The present case report illustrates delayed surgical removal of a maxillary third molar that was displaced into the infratemporal fossa, via the intraoral access and under local anesthesia. Despite the rarity of this complication, oral and maxillofacial surgeons should be aware of its management and able to choose the optimal technique, taking into account the patient's signs and symptoms as well as the knowledge and experience of the surgeon.
La extracción del tercer molar es un procedimiento habitual que pocas veces se asocia a complicaciones. Una posible complicación asociada es el desplazamiento de la pieza dental a la fosa infratemporal, una estructura anatómica que contiene el músculo temporal, el músculo pterigoideo interno y externo, el plexo pterigoideo, la arteria maxilar y sus ramas, el nervio mandibular y sus ramas y la cuerda del tímpano (una rama del nervio facial). El caso descrito en este manuscrito ilustra la extracción quirúrgica diferida de un tercer molar maxilar que se había desplazado a la fosa infratemporal, a través de un acceso intraoral y con anestesia local. A pesar de que es una complicación excepcional, el cirujano experto en cirugía oral y maxilofacial debe conocer su tratamiento y seleccionar la técnica óptima, teniendo en cuenta los signos y síntomas manifestados por el paciente, y en función de sus conocimientos y experiencia.
The most common procedure in oral and maxillofacial surgery is extraction of the third molar.1 The complication rate associated with this procedure ranges from 2.6% to 30.9%.2,3
Common complications of mandibular third molar surgery include alveolar osteitis (dry socket), secondary infection, nerve dysfunction, and hemorrhage.4 When manipulation of a maxillary third molar is required, other types of complication may arise, such as tuberosity and root fracture, oroantral communication, and displacement of the tooth into adjacent structures,1,5 including displacement into the infratemporal fossa.
The infratemporal fossa is an irregularly shaped space located below the greater wing of the sphenoid bone (containing the foramen ovale), lateral to the ramus of the mandible and the gap between the zygomatic arch and temporal bone (forming the communication to the temporal fossa). The lateral pterygoid plate forms the medial margin while the maxilla forms the medial aspect of this space. The temporalis muscle, medial and lateral pterygoid muscles, pterygoid venous plexus, mandibular nerve and its branches, maxillary artery and its branches, and the chorda tympani nerve are all contained in the infratemporal fossa.6 The parapharyngeal space lies medially and communicates with the mediastinum.
There is no consensus in the literature or established management approach for displacement of the third molar into the infratemporal fossa. Surgical and conservative approaches have been reported7–9; the surgeon is expected to select the most appropriate strategy for each case.
Recommended management steps include immediate surgical removal if possible, initial watchful waiting and delayed removal, or observation alone. Complications associated with the presence of the tooth in the infratemporal fossa include infection, limitation of mandibular movement, and psychological discomfort. Sometimes, the displaced tooth may migrate inferiorly spontaneously and become accessible via the intraoral access.10
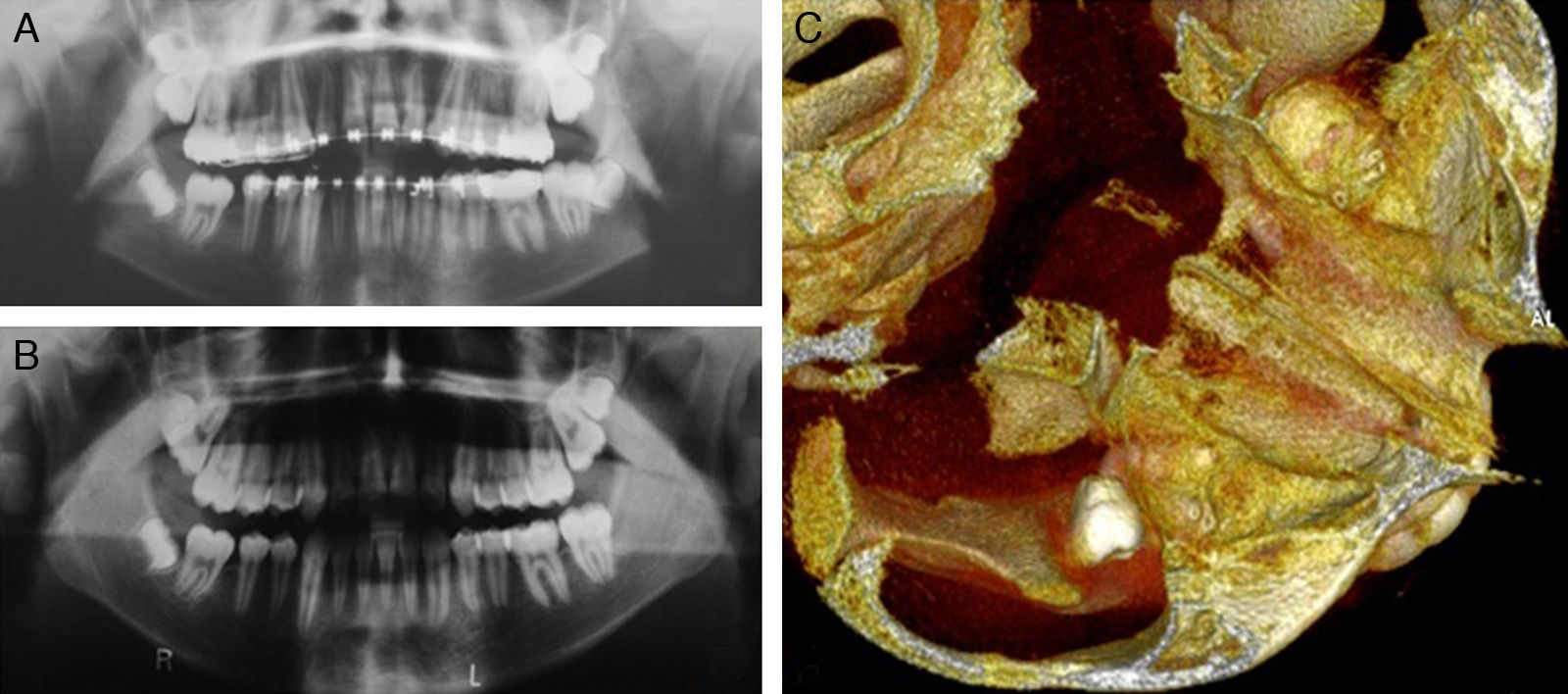
Case reportA 14-year-old girl was referred by her orthodontist to oral and maxillofacial surgery service for third molar extraction. After anamnesis, clinical and radiographic examinations (Fig. 1a), the left mandibular third molar (38) was removed uneventfully. One year later, extraction of the right maxillary third molar (18) was attempted. During the procedure, this tooth was accidentally displaced into the adjacent anatomical space.
The patient and her legal guardian were notified of the situation as soon as possible, and the decision was made to carry out further imaging to support case planning. Movement of the tooth was visible on pantomography (Fig. 1b). Cone bean tomography (Fig. 1c) revealed displacement of the tooth into the infratemporal fossa.
As the patient was asymptomatic, watchful waiting was chosen as the initial course of management. After 4 months, the tooth could be felt during palpation in the region of the second molar.
All possible treatment options, whether conservative or surgical, were discussed with the patient and her family. Extraction of the tooth under local anesthesia was chosen. The procedure was performed under local anesthesia, through an incision made with an electrocautery at the point of palpation (Fig. 2a). After tissue dissection, the tooth was visualized (Fig. 2b) and extracted (Fig. 2c). The patient had no functional complaints on 14-day follow-up. A follow-up pantomogram confirmed complete extraction of the tooth (Fig. 2d).
DiscussionPreoperative planning, use of proper technique, and adherence to basic surgical principles are essential to achievement of treatment success in oral surgery. Inadequate clinical and radiographic examinations, use of excessive or uncontrolled force during extraction, incorrect technique, thickness of the cortical bone in the third molar region, fashioning an inadequate flap that permits only limited visualization during surgery, and third molar crown above the level of the apex of the adjacent tooth are risk factors for displacement of the maxillary third molars into the adjacent anatomical spaces.9,11
In this particular case, observation of preoperative radiographs shows that the tooth was not above the apex of the adjacent second molar, insofar as this tooth was also impacted. The third molar was located at an extremely superior position, making extraction challenging due to limited surgical access and proximity to neighboring anatomical spaces. In addition to the young age of the patient, we can speculate that the distal wall of the third molar was extremely fragile. Moreover, the absence of root formation makes it very difficult to secure a foothold for extraction, contributing to the risk of displacement. Displacement into the infratemporal fossa usually occurs through the periosteum, leaving the tooth at the lateral wall of the pterygoid process of the sphenoid, under the lateral pterygoid muscle.12
Computed tomography is the imaging modality of choice for precise determination of the position of the displaced tooth and surgical planning. If tomography is not available, plain radiographs—including occlusal, panoramic, lateral and waters views—can be used, bearing in mind the limitations of each projection.13
The literature shows that surgical management options for extraction of third molars displaced into the infratemporal fossa are varied, including local or general anesthesia, intraoral access with Caldwell-Luc technique or resection of the coronoid process,13 combined or exclusively extraoral access (hemicoronal approach),7 or the Gillies approach.5
When choosing a management approach, the surgeon must be aware of the potential risk of injuring important anatomical structures, such as the branches of the mandibular nerve, otic ganglion, chorda tympani, maxillary artery, and pterygoid venous plexus.14 In the case reported herein, extraction was performed under local anesthesia using an exclusively intraoral approach similar to that described by Sverzut et al.,9 Gómez-Oliveira et al.,10 and Selvi et al.11
A notable procedural complication of extraction of a third molar displaced into the infratemporal fossa is bleeding of the pterygoid plexus, which can make visualization of the tooth very difficult. Moreover, the surgeon must carefully control the strength applied during dissection and attempted extraction, so as to prevent even greater displacement of the tooth into the skull base.13 To avoid further posterior displacement, the surgeon should protect the distal tissues with a blunt instrument, as described by Patel and Down.13
If, during third molar extraction surgery, the operator suspects that the tooth may displace into an adjacent space, it is advisable to extend the flap and attempt to remove the tooth in order to avoid a second procedure, thus reducing morbidity. When the tooth is displaced into the infratemporal fossa, some authors propose removal be performed as soon as possible due to the risks of infection, foreign body reaction, or trismus.9 If the surgeon cannot visualize the tooth or believes immediate extraction is not possible, it is prudent to abort the procedure and place sutures for hemostasis. In this particular case, our approach was to deliberately delay extraction, waiting for the formation of scar tissue around the tooth to facilitate localization and removal, as described by Sverzut et al.,9 Gómez-Oliveira et al.,10 and Selvi et al.11
Despite the fact that displacement of a maxillary third molar into the infratemporal fossa is a rare occurrence, the oral and maxillofacial surgeon is expected to know the surgical techniques available for management of this complication. Selection of the most appropriate technique should take into account the signs and symptoms of the patient as well as the knowledge and experience of the surgeon.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors declare that they have no conflict of interest.
None.