The most frequent oral lesions are those expressed by reactive gingival growth1,2 and they usually present an indolent behavior. However, there is a great variety of different lesions which are clinically similar, and it is what makes the diagnosis difficult.3 For instance, we could mention peripheral ossifying fibroma which has a complex diagnosis as it shares clinical and histological characteristics which are common to other conditions.4
Basically, ossifying fibromas may be divided into two types: central and peripheral.5 Reports of intraoral peripheral ossifying fibroma started in the late 40's,2 and nowadays it is a relatively common lesion corresponding to 9.6% of gingival biopsies.6 As regards to pathogenesis, it seems to be related to periodontal ligament,7 once it exclusively develops in the gingival portion of the maxilla, because of proximity of periodontal ligament and gum, and because of the presence of oxytalan fibers inside the mineralization of some lesions.3–8 In addition, the presence of trauma or chronic irritation is especially related to the etiology of these gingival conditions, for instance, presence of calculus, plaque, orthodontic braces, restorations and maladjusted prosthesis.1 In the specific case of peripheral ossifying fibroma, many authors consider it as a focal, reactive, non-neoplastic lesion of soft tissue2–9 which usually develops from interdental papilla.4–7
Regarding clinical aspects, peripheral ossifying fibroma is usually presented as a single sessile- or pedunculated-based nodule covered by mucosa which has a color that ranges from pink to red,6 and its surface may be ulcerated or not, flat or uneven.2–7 The most frequent location of this lesion is the portion of upper incisor teeth4 and the size of most lesions does not exceed 1.5cm.5,6,10 However, when we are dealing with gingival lesions, clinical characteristics are insufficient for a final diagnosis once they are common to several lesions, therefore, histopathological examination is always necessary to determine the diagnosis.3
Despite peripheral ossifying fibroma corresponding to a common gingival lesion, case reports describing it are scarce.9 Thus, due to the large size of the lesion that causes the destruction of tissues supporting the teeth involved, associated with its rarity in the mandible, the description of the authors who conducted this clinical case is relevant and important.
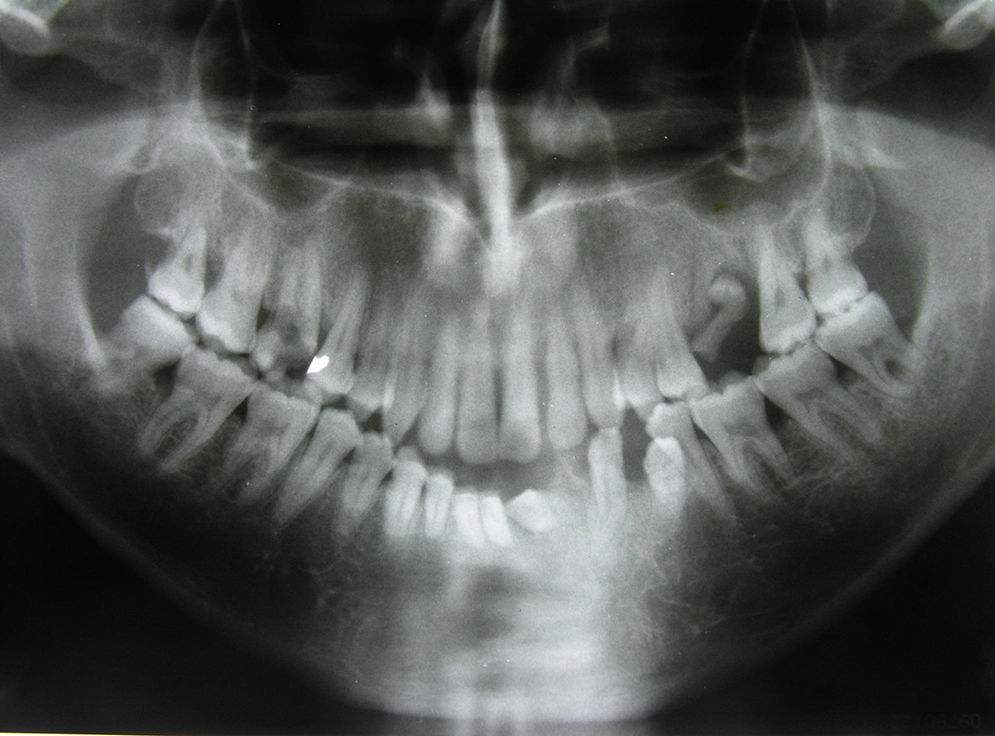
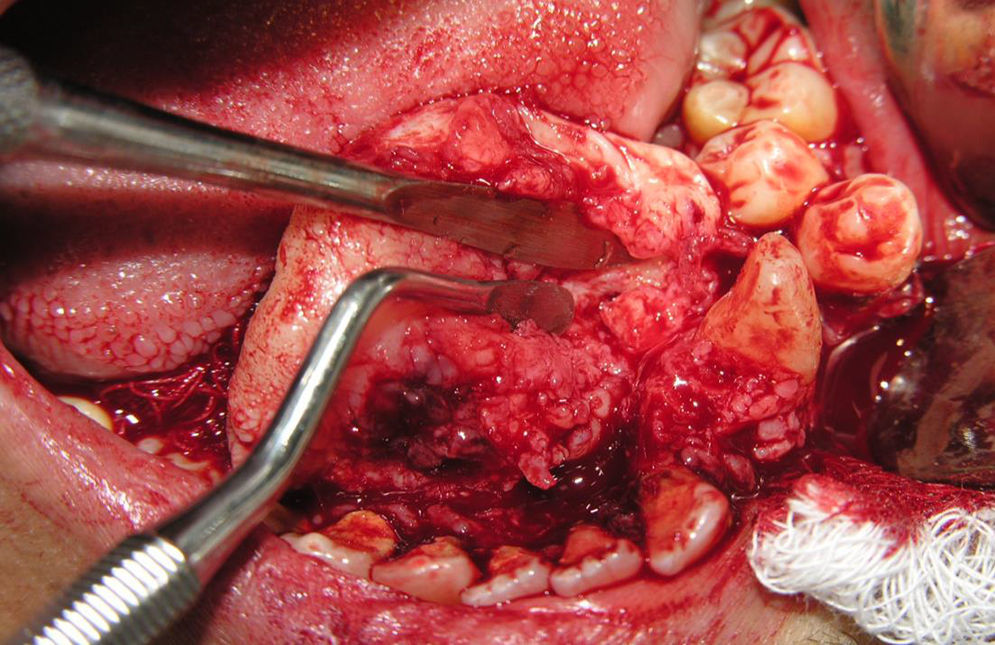
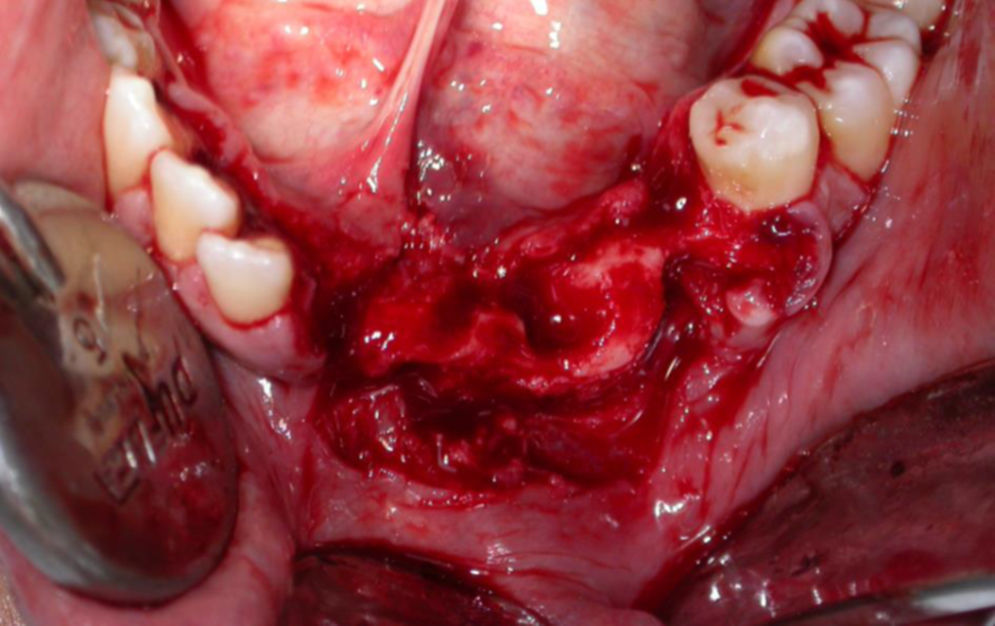
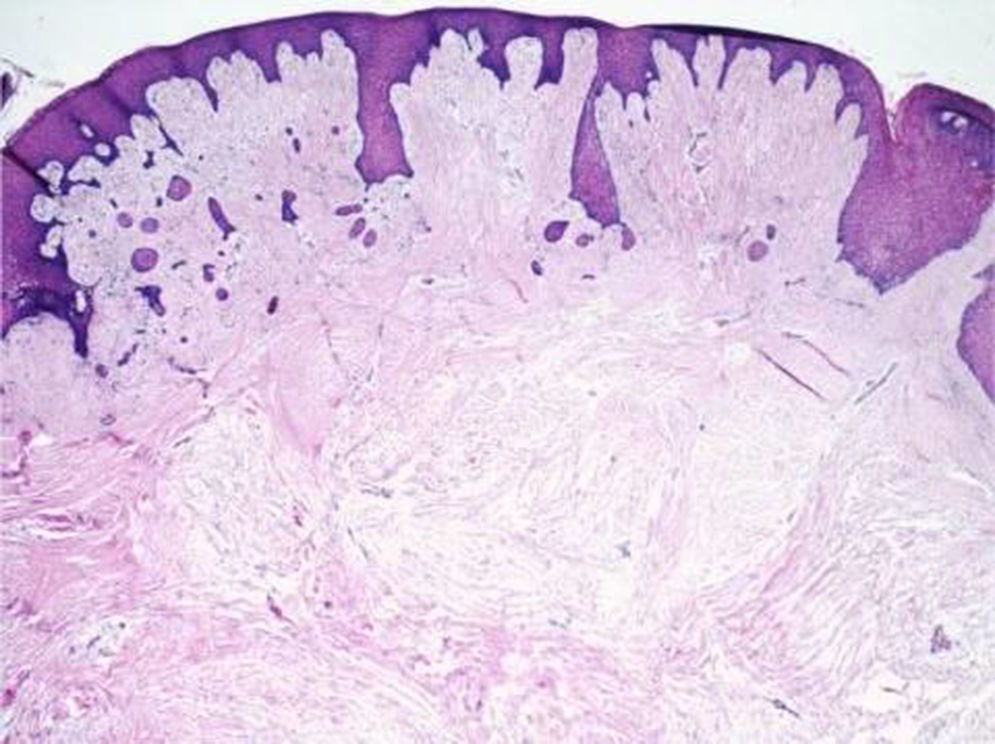
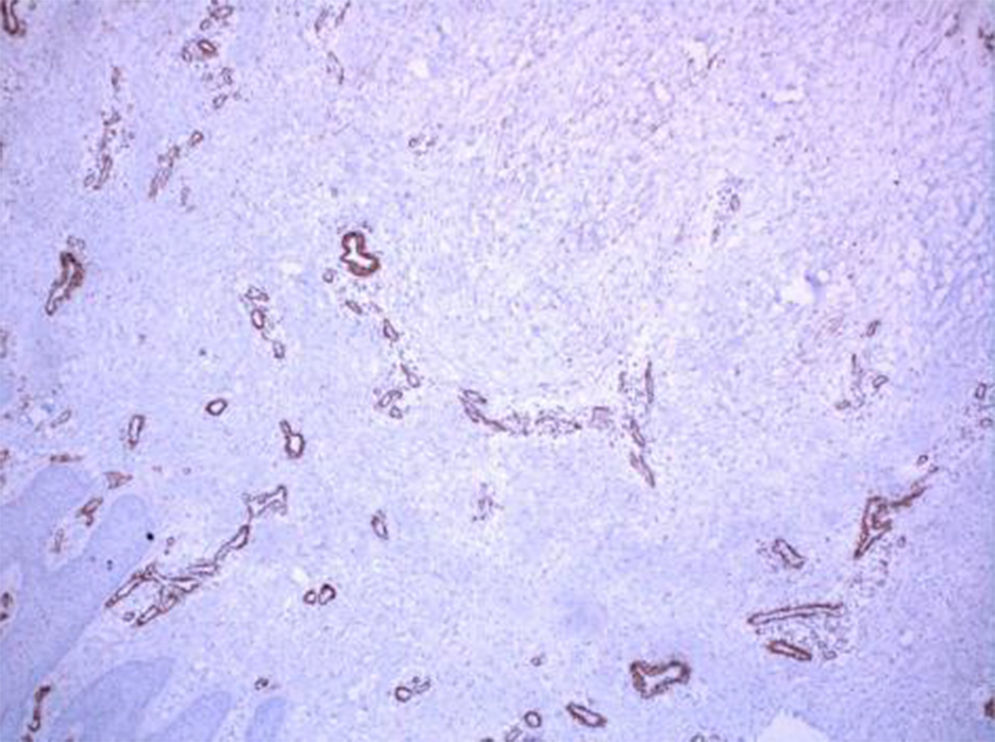
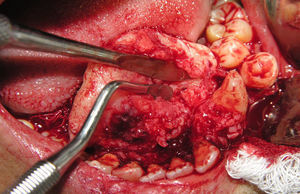
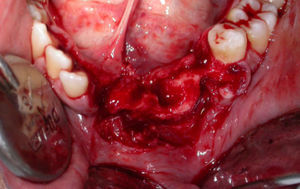
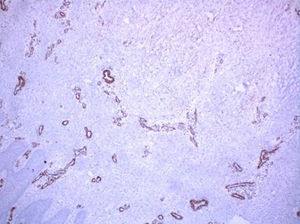
Case reportJ.L.O., a 38-year-old patient was referred to treatment experiencing an extensive lesion involving anterior portion of lower alveolar border with a 10-year progress history. Upon extraoral examination, patient's difficult labial sealing was noticeable by virtue of change in the lower third of the face due to intraoral growth of the lesion. Intraoral clinical evaluation revealed a large-sized lesion involving the anterior portion of the mandible, promoting displacement of teeth 41, 31, 32, 33 and 34 (Fig. 1). Similarly, dental displacement was radiographically clear and the lesion presented slight radiopacity (Fig. 2). Despite the lesion being covered by intact mucosa of normal color, during planning we chose to perform an incisional biopsy prior to definite surgical treatment, by which diagnosis was of inflammatory fibrous hyperplasia. Surgical Access occurred through a wedge incision surrounding the lesion, associated with intrasulcular incision in involved teeth and tissue displacement was performed with the aid of a Molt separator (Fig. 3). Following complete removal of the lesion, dental extraction of involved teeth was performed since they presented compromise of supporting periodontium (Fig. 4). Tissue was repositioned using 5-0 Polypropylene wire and the piece was sent to histopathological examination. Lesion was microscopically described by the presence of dense fibrous connective tissue with multiple vital bone trabeculae, surrounded by uneven pavimentous epithelium (Fig. 5). The presence of mixed inflammatory infiltrate was also seen. In addition to routine HE staining, immunohistochemistry was performed for actin in smooth muscle tissue, in which positivity to HHF-35 was observed (Fig. 6), thus confirming myofibroblastic characteristic of the lesion. Therefore, the diagnosis of excisional biopsy was peripheral ossifying fibroma. The patient recovered with no incidents and clinical and radiographic 12-month follow-up revealed absence of relapses (Figs. 7 and 8).
Reactive or inflammatory gingival lesions are commonly found in oral cavity, corresponding to over 90% of gingival biopsies.1 The most mentioned ones are inflammatory fibrous hyperplasia, pyogenic granuloma, peripheral ossifying fibroma, and giant-cell granuloma.2 Among them, peripheral ossifying fibroma stands out due to its relapsing characteristic.4 Ossifying fibromas are rare lesions affecting especially the craniofacial area11 and the first descriptions were made by Menzel in 1872.12 They are classified into two types, central and peripheral. The first one develops from endosteum or periodontal ligament from radicular apex and grows at the cost of medular bone expansion. On the other hand, peripheral type develops in a continuous manner with periodontal ligament, involving only gingival portion.5 In this article, the authors describe a case of large peripheral fibroma affecting the anterior portion of the mandible.
Gingival lesions, of the classification in which peripheral ossifying fibroma is placed, seem to share the same etiology, which corresponds to the presence of trauma and local irritating factor.2,7 In this regard, the participation of biofilm is clear in this clinical case since the patient had unsatisfactory hygiene with the presence of plaque and calculus throughout his oral cavity mainly in the area of the lesion, where bone loss was significant. Besides, some authors connect the appearance of peripheral ossifying fibroma with hormone changes,4–8 as it is 2–4 times more prevalent in females6–10 and because the most commonly affected age group is the second decade of life.3,9 However, in this work, the lesion was diagnosed in a 38-year-old male patient. Regarding the race in which the lesion is more frequent, Caucasians seem to be more affected than Blacks.2 In spite of it, in this clinical case, the lesion was diagnosed in a Pardo patient.
In addition to the fact these gingival lesions share the same etiology, the similarity in clinical and histological characteristics is also true. In this context, the diagnosis of peripheral ossifying fibroma generates a little confusion among authors.4–9 Therefore, many expressions have already been used to refer to this lesion, such as: peripheral fibroma with calcification, calcifying fibroma, peripheral cemento-ossifying fibroma, peripheral fibroma with osteogenesis, peripheral fibroma with cementogenesis, among others.3–7 Then, when it concerns gingival conditions, it is necessary to establish a differential diagnosis.2 And despite peripheral ossifying fibromas being described as clinically astonishing due to massive growth, according to Zhang et al. (2007),13 as in this work, carcinoma has been inserted in differential diagnosis in only 2% of the cases. In this clinical case, as stated by Silva et al. (2007),1 the diagnosis hypotheses raised were giant-cell peripheral lesion, inflammatory fibrous hyperplasia, and peripheral odontogenic fibroma.
Regarding time of lesion progress, according to Farquhar et al. (2008),2 it may be present in oral cavity for some months to years, depending on interference with function and discomfort to patient. Strangely, despite the large extension of the lesion diagnosed in the concerned clinical case, causing considerable functional interference and discomfort, and leading to difficult labial sealing, history of progress was 10 years. This situation may be explained by silent growth and symptomatology of the lesion,3,10 which makes it possible that it is present for several years before a patient seeks treatment.2 It results in extensive lesions, with greater tissue and teeth involvement as observed in this work.
Upon clinical examination, the lesion is often described as a pedunculated or sessile nodular mass,3 and sessile-based is the most frequent presence.5 Regarding location, 50% of the lesions affect the region of incisors and more than half of it is located in upper arch (60%).14 Single lesions are the most frequent ones1; despite that Kumar et al. (2006)7 have described a multisite case. In this context, with respect to location, the lesion hereof may be considered as having an atypical location because it affects lower arch. However, regarding positioning in the arch and lonesome appearance, it is in compliance with literature reports because it presented as a single lesion affecting anterior portions of lower border. Other authors have also occasionally described peripheral ossifying fibromas in sites different from the most common ones. Pal et al. (2012),4 for instance, described a lesion affecting the posterior portion of the mandible.
Regarding the extension of the lesion, in most cases, the longest length does not exceed 1.5cm.4,10 On the other hand, in this clinical case, authors described a peripheral ossifying fibroma that outstands for its large size, which is 3.5cm in its longest extension. Similarly, some authors have occasionally described larger lesions, with case reports of peripheral ossifying fibromas from 6 to 9cm.2,15 Sometimes, especially in cases of larger lesions, ectopic eruption, migration, and separation of teeth have been reported, as well as bone destruction.1,6,16 These uncommon aggressive characteristics were seen in this case report, where massive growth of the lesion has caused destruction of tissue supporting the teeth involved, as well as its migration, which did not allow their maintenance after total exeresis of the lesion.
Upon radiographic evaluation, in some cases the presence of radiopaque diffuse calcifications is observed in a shadow of soft tissues and rarely there is associated bone destruction.4,9 Regarding radiographic appearance of tooth migration, it is present only in 5% of the cases, thus constituting a very rare finding, as well as radicular resorption.1 In this work, marked dental displacement associated with slight radiopacity of the lesion was radiographically observed; however radicular resorption was not seen.
As regards to microscopic evaluation, in Bhaskar and Levin's (1973)16 work, 22 peripheral ossifying fibromas were microscopically assessed and 73% of the cases were observed to have mineralized mass surrounded by a stroma of fibrocellular connective tissue. Analyzing mineralized tissue in a separate manner, it was observed that in 50% of the cases the constitution exclusively occurred through bone tissue and 18% were observed to be associated with bone tissue and cementum. In addition, the association between lamellar bone and tissue (13.6%) was observed, as well as formation exclusively by cementum (18%). Regarding epithelial cover, stratified pavement epithelium may be present as intact or ulcerated,6 and the presence of ulcerations is seen in 20% of the cases.1 In this report, the presence of mineralized material consistent with cementum was not observed, and the lesion was microscopically described by the presence of dense fibrous connective tissue with multiple bone trabeculae, covered by uneven pavement epithelium. Immunohistochemistry analysis of the lesion was also performed for smooth muscle actin, in which positivity for HHF-35 (anti-muscle actin antibody) was observed. Although it is not much used to diagnose fibro-osseous lesions,17 some authors such as Marcos et al. (2010)3 have already made use of this diagnosis resource in their study of four cases of peripheral ossifying fibroma and the results support a fibroblastic–myofibroblastic origin of the lesion, thus helping in its differential diagnosis. However, Lombardi and Morgan (1995)18 observed negative immunolabeling for SMA in peripheral ossifying fibromas and fibrous hyperplasia. In this clinical case, myofibroblastic origin of the lesion was proven, because we have observed immunopositivity for HHF-35 antibody.
The treatment of peripheral ossifying fibroma comprehends total exeresis of the lesion including periosteum and periodontal ligament, as well as all irritating factors that may cause its reappearance, since relapse rates are significant.1,7 Thus, in this clinical case, we decided to completely remove the lesion, along with extraction of the teeth involved. For such, we took into account the fact that these teeth have already presented supporting periodontium compromise and significant displacement associated with the need for removal of any factor that might predispose to relapses. In this manner, dental extraction was necessary not only because of periodontal compromise but also to eliminate the possible origin of the lesion, which according to literature, is related to periodontal ligament.4,9 Although the origin of the lesion in periodontal ligament is well supported in literature, there are isolated reports of peripheral ossifying fibroma in toothless patients.7
Relapse rate of peripheral ossifying fibroma is considered high, ranging from 8% to 20%3,10 and it is usually related to incomplete elimination of the lesion and to local irritating factors.4 Then, a strict postoperative follow-up is necessary to early detect relapses,2 since 1 out of each 5 lesions relapse after excision.6 Despite the large extension and the aggressive feature of the lesion described, as well as its relapsing tendency, in the thorough clinical and radiographic postoperative follow-up over 12 months, no relapse was seen. The authors believe that the recovery with no incidents and no relapses is due to a surgical procedure properly performed with respect to complete removal of the lesion associated with periodic control of the patient regarding elimination of plaque and other bacterial foci.
In front of pathologies like this that has been presented, it reinforces the need to follow-up annually for recurrences that are detected early and treatments properly conducted.
Conflict of interestThe authors hereby certify that there is no conflict of interest with any financial organization regarding the material discussed in this manuscript.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
We thank the Clinic & Surgery Department, Alfenas Dental School, Federal University of Alfenas-UNIFAL, Minas Gerais, Brazil, and funding agencies CAPES (Coordination for the Improvement of Higher Level- or Education-Personnel), FAPEMIG (Foundation for Research Support of Minas Gerais) and CNPQ (National Counsel of Technological and Scientific Development).