Sinus augmentation is a preprosthetic technique for rehabilitating posterior sector of the atrophied maxilla with implant-supported prosthesis. We retrospectively analyzed 34 consecutive sinus augmentations performed using only bovine hydroxyapatite.
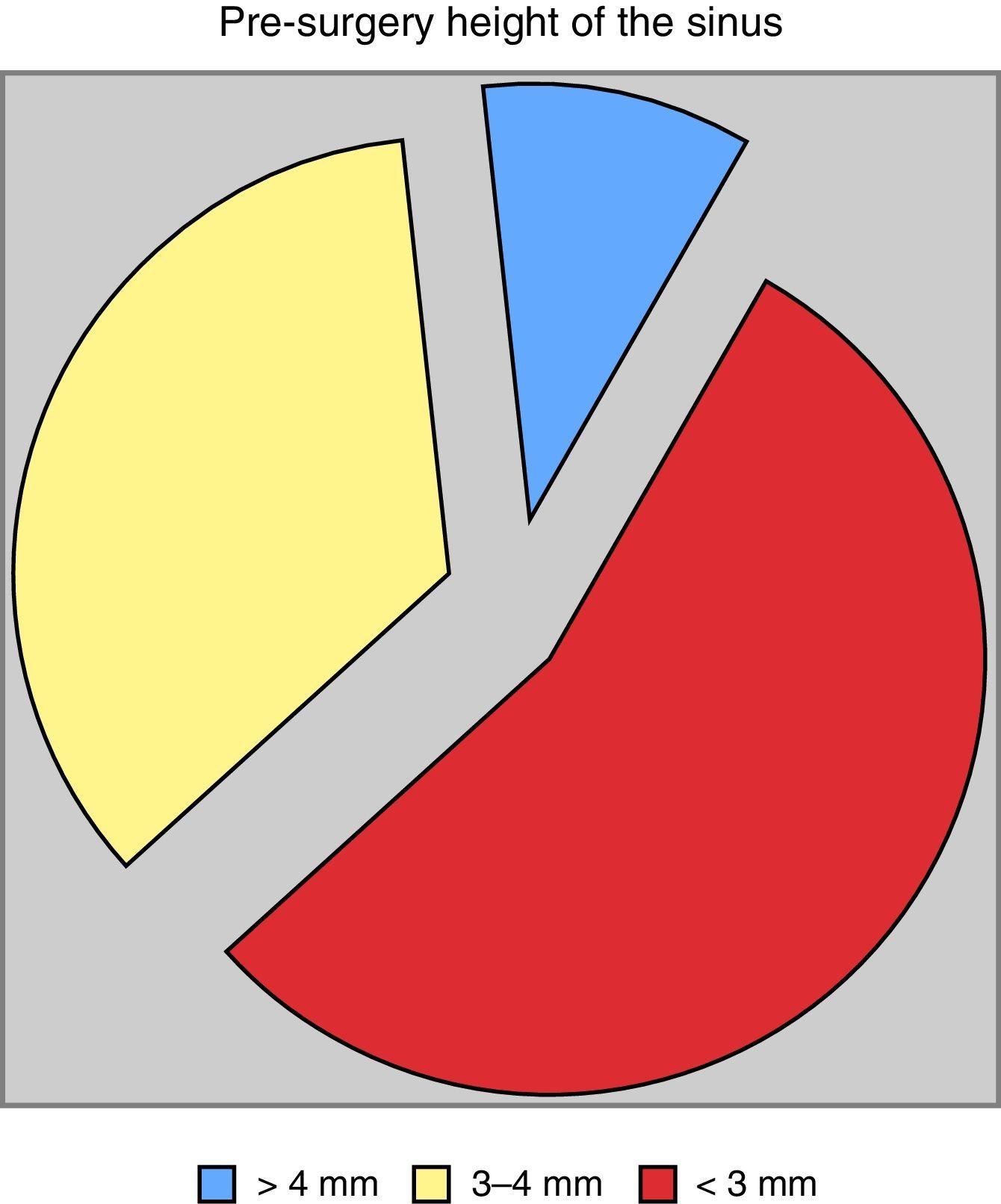
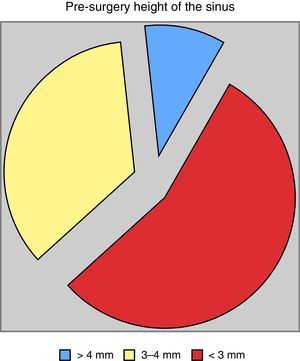
The presurgical height in 92% of the cases was 4mm or less.
The success rate of the maxillary sinus augmentation was 100% for this technique. 13.4% of the implants were placed immediately with a success rate of implants placement of 93.9%. The non-osseointegrated implants were all successfully replaced. Follow-up period was 1268 days.
The success rate obtained using bovine hydroxyapatite alone is similar to that using other types of materials, while avoids morbidity of the autologous bone donor area.
La elevación del seno es una técnica preprotésica para la rehabilitación del sector posterior atrofiado del maxilar con una prótesis de implantación. Analizamos retrospectivamente 34 casos consecutivos de elevación del seno maxilar con el empleo de tan solo hidroxiapatita bovina sola.
La altura prequirúrgica era de 4mm o menos en el 92% de los casos.
El porcentaje de éxitos de la elevación del seno maxilar con esta técnica fue del 100%. Un 13,4% de los implantes se colocaron inmediatamente, con un porcentaje de éxitos de la implantación del 93,9%. Los implantes no osteointegrados se sustituyeron todos con éxito. El periodo de seguimiento fue de 1268 días.
El porcentaje de éxitos obtenido con el empleo de hidroxiapatita bovina sola es similar al de otros tipos de materiales, al tiempo que se evita la morbilidad en el área donante de hueso autólogo.
Sinus augmentation was first reported by Tatum in 1976 and subsequently described by Boyne and James in 1980.1,2 It is a preprosthetic technique to increase the height of the lateral and posterior sectors of atrophied maxillas for their rehabilitation with implant-supported prostheses. It is a predictable technique to restore sufficient bone volume for implant placement.3
The etiology of maxillary bone resorption is multifactorial and influenced by age, bone diseases, and tooth extractions. Thus, bone resorption continues after tooth extraction, producing a decrease in height and width. With the decrease in bone height, the remnant bone narrows and becomes closer to the nasal cavity, maxillary sinuses, and the group of nerves of the incisive canal.4 Patients with severe maxillary atrophy are subject to changes in masticatory, swallowing and speech function, and these changes can often result in psychological problems.
During the maxillary sinus floor elevation procedure, the space created between the residual maxillary ridge and the elevated Schneiderian membrane is usually filled with grafting material. In this way, a bone fraction is created that may allow for reliable implant placement, either simultaneously with the elevation procedure when the residual ridge allows for primary implant stability or as a second stage after healing of the grafted site.5
The utilization of different filling materials has been reported after augmentation. The autologous graft is the gold standard, given its osteogenic, osteoinductive, and osteoconductive properties. It can be obtained from different areas, including retromolar trigone, chin, or iliac crest. Other options, such as allografts, xenografts, and alloplastic materials, have also been widely reported in the literature.
Recent studies analyzed maxillary sinus filling with periosteal cell grafts from the lateral jaw.6 Some authors have also supported the non-utilization of cavity filling.7
Other available techniques to increase the maxillary height include bone splitting, bone sandwich graft after LeFort-type osteotomy, and onlay grafts.
The objective of this study was to retrospectively analyze sinus augmentations performed with biomaterial alone as well as the implants success rate. We also describe different complications that were observed during the procedure.
Materials and methodsThis retrospective study included 34 consecutive sinus augmentations performed with biomaterial alone from 2008 through 2011.
All surgeries were performed by the same surgeon. Outcomes were evaluated by a maxillofacial surgeon not connected with the clinic, based on radiological images and clinical records. In all patients, the bone quality of the posterior maxilla was type 4 according to Misch's classification.8
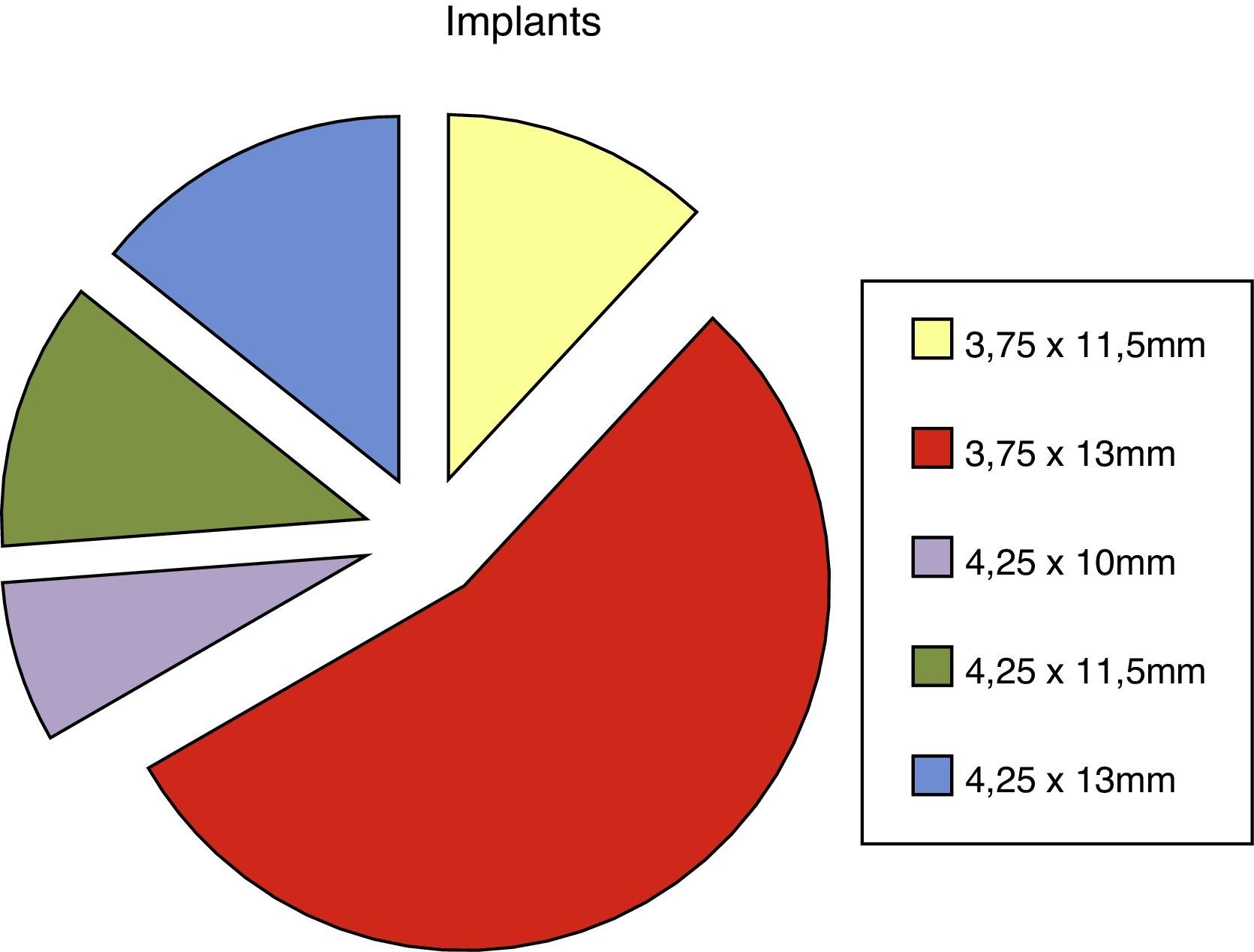
Out of 95 sinus augmentations performed with autologous bone filling, a mixture of bone with hydroxyapatite, or bovine hydroxyapatite alone, we selected 34 augmentations that used bovine hydroxyapatite alone. 61 sinus augmentation were rejected due to the use of a mixture of materials. In these patients, we inserted 84 titanium implants with RBM-treated surface, external hexagon and standard platform.
Data were gathered on the sex, age, concomitant diseases, pre- and post-augmentation height, time interval between sinus augmentation and implant placement, timing of prosthetic loading, complications during surgery, and implant losses.
In all patients, an initial panoramic X-ray and CT scan were performed to yield the maximum possible information on the sinus anatomy and to rule out associated disease. All patients subsequently underwent another panoramic X-ray and/or CT scan.
Bone gain was measured manually in the panoramic X-ray at 180 days (the magnification was taken into account).
Surgical protocolAll procedures were conducted under local anesthesia (articaine with adrenalin).
The surgery consisted of a crestal incision with anterior and posterior release incisions. The mucoperiosteal flap was lifted and the Caldwell-Luc procedure was performed for lateral access (Fig. 1), preparing an oval osteotomy (Fig. 2) with a tungsten bur and irrigating with saline solution; perforation of Schneider's membrane was avoided by carefully detaching it from the sinus walls with membrane elevators.
A oxidized cellulose polymer layer was placed on the augmented sinus floor in order to isolate possible undetected microperforations (Fig. 3), and the cavity was then filled with two bovine hydroxyapatite vials and compacted (Fig. 4). A resorbable collagen membrane of equine origin was placed for the correct isolation of the area. No periodontal dressing material was used.
None of the patients had sinus pathology.
All patients were treated with amoxicillin–clavulanic acid (clindamycin for allergic patients) before and after the procedure.9 They started the treatment an hour before the surgery with amoxicillin 875mg-clavulanic acid 125 every 8h and they completed 7 days of treatment. 0.12% chlorhexidine as an oral rinse for ten days was used as well. Sutures were removed at one week post-surgery.
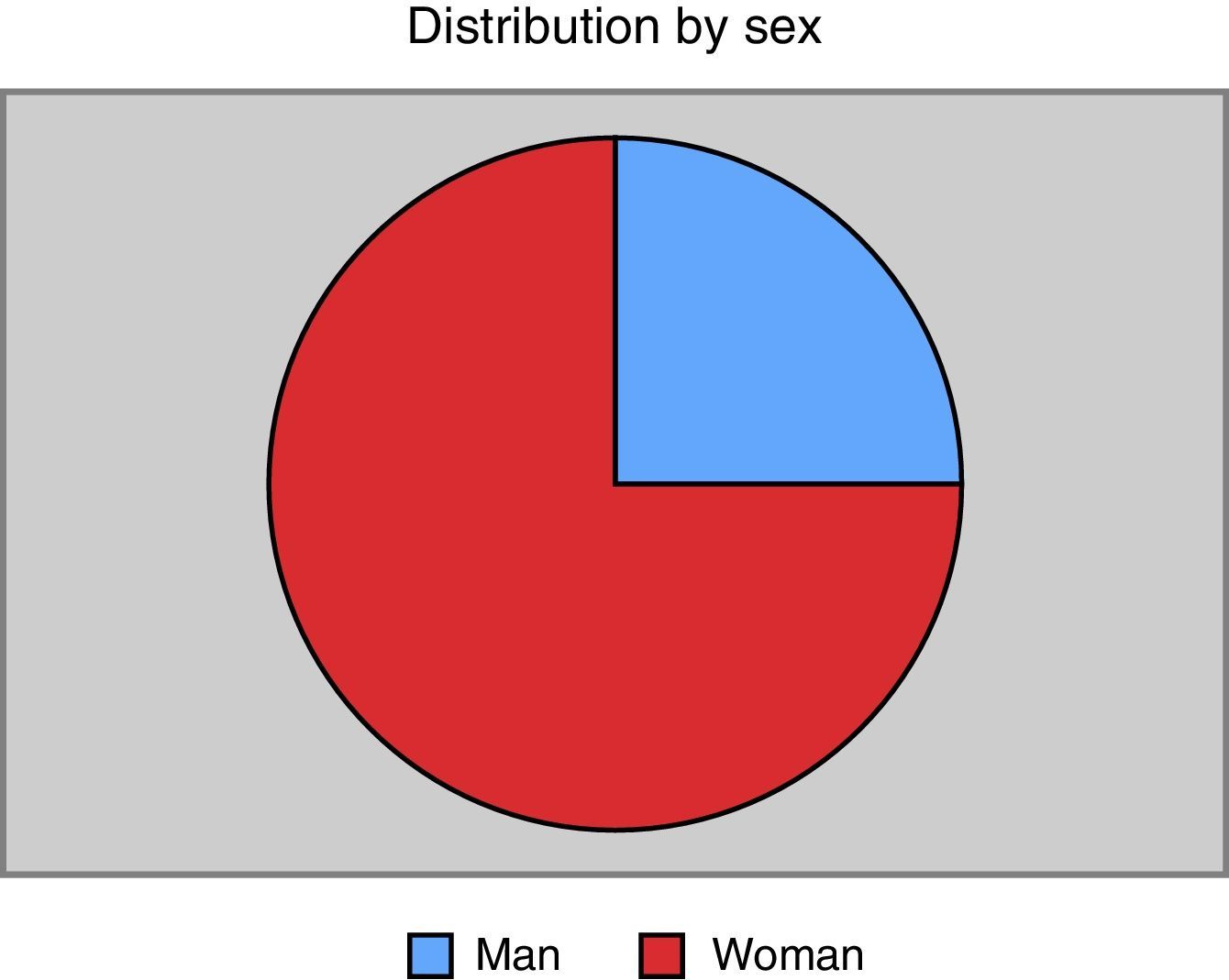
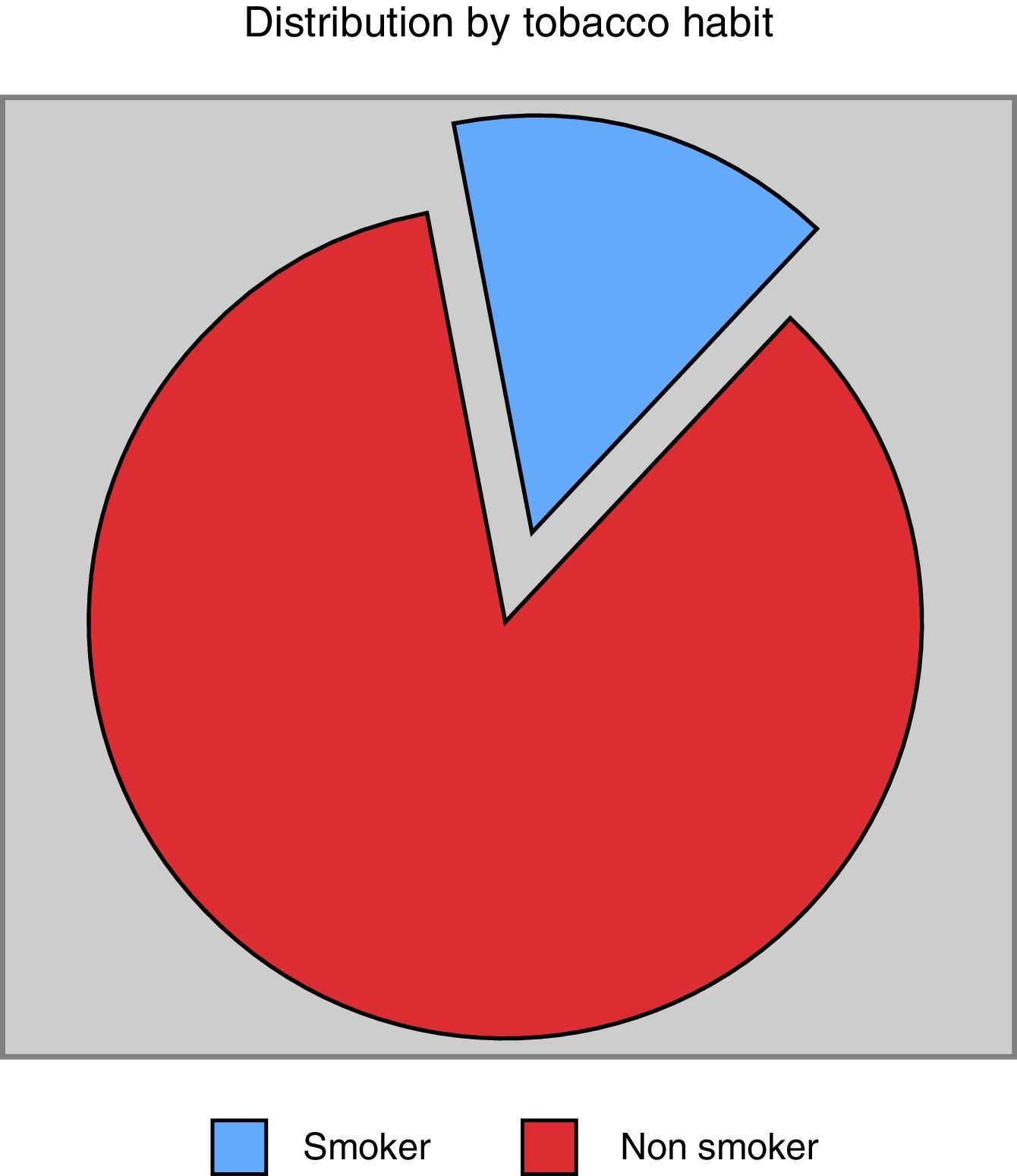
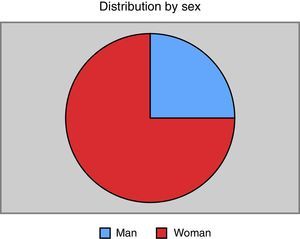
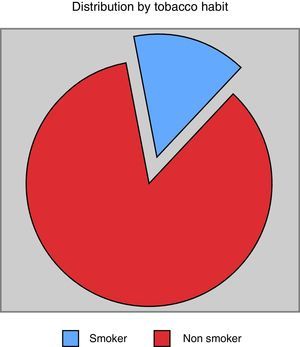
ResultsThe study included 34 patients, in whom 37 sinus augmentations were conducted; 75% were female (Fig. 5), the mean age was 54 years, and 14.7% of patients were smokers (Fig. 6). One patient was diabetic and one had a history of bisphosphonate treatment that had been suspended more than six months before the surgery.
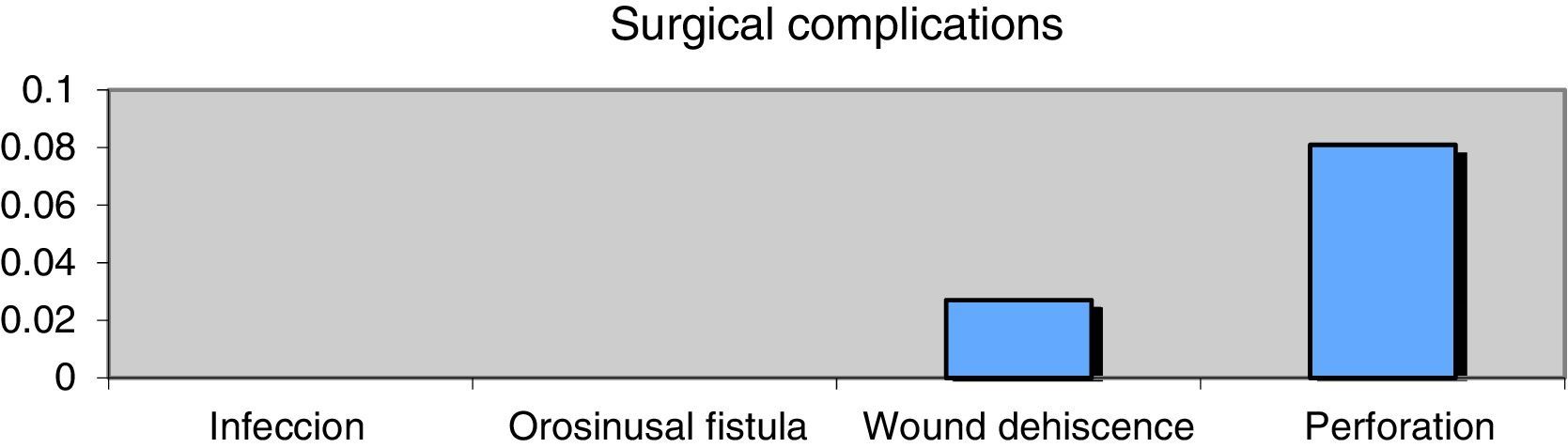
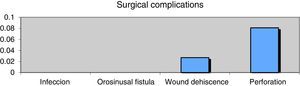
Three Schneider membranes were perforated (8.1%) during the sinus augmentation procedure, and one implant was lost during the osseointegration period. There was no relation between the perforation cases and the implant lost.
There were no cases of postsurgical infection and no oral-sinus communication (Fig. 7).
The mean sinus bone height was 3.1mm at baseline (i.e., most sinuses were severely resorbed) (Figs. 8 and 9) and 11.2mm post-treatment. A success rate of 100% was obtained for this technique.
Eighty-two implants were placed (all of them were from the same trademark); only 13.4% were placed immediately (height of >4mm), given the severe maxillary atrophy (92%) in the majority of the patients.
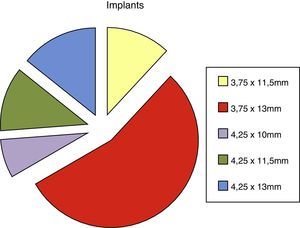
Five implants were lost during the osseointegration period, giving a success rate of 93.9%; these non-osseointegrated implants were all successfully replaced. The implants were loaded at a mean of 143 days after their placement (Fig. 10), and the mean follow-up period was 1268 days (range, 396–2778 days). The different sizes places are seen in the chart (Fig. 11).
No implant failure rate was observed in patients with comorbidity or tobacco habit.
DiscussionThe aim of sinus augmentation is to increase the height of the posterior and lateral sectors of the maxilla to permit implant placement for the rehabilitation of patients with atrophic maxilla. Given the concomitant morbidity and rapid resorption of autogenous bone, usually endochondral bone, various bone substitutes have been studied,10 including a mixture of autologous bone with hydroxyapatite, hydroxyapatite alone, ceramic materials, and methylcellulose, among others.
Some authors found that the use of bovine hydroxyapatite avoids donor area morbidity while offering a similar implant success rate to that obtained with other materials; these studies, published in 2005, found no significant differences between sinus augmentation with tricalcium phosphate or autologous bone grafts.10,11 Bovine hydroxyapatite, which has osteoconductive properties, is obtained from bovine bone in which the organic component has been completely removed. It is believed that the thermal and chemical treatment used to extract this component produces losses in antigenicity and in the potential inflammatory response.
In comparison to autologous bone grafts (e.g., from iliac crest or parietal bone), the use of bovine hydroxyapatite avoids the need for general anesthesia during surgery and precludes donor area morbidity.
Thus, there are authors who believe that there is no reason to prefer autogenous bone over bone substitutes.12
It has been studied the maxillary sinus lift with out any graft material, but in critic defects, the Oliveira et al. conclude that the poor bone gain results are mainly associated with insufficient bone quality and the large scope of the defects.13
It is remarkable that in Rickerts’ metaanalyses published in 2011 comparing the bone fraction after applying: autogenous bone and bone substitutes (bovine hydroxyapatite, bioactive glass, corticocancellous pig bone) revealed no significant differences in bone formation after five months.14 Zijderveld et al.12 concluded that the sinus augmented with autogenous bone, the newly formed bone was significantly higher than in the b-tricalciumphosphate group after the same healing period.
Membrane perforation was observed in 8.1% of our cases with size less than 2mm. This is the most frequent complication,15 and was recorded in 10.1% of cases by Cho-Lee et al.15 and in 18.42% of cases by Herrero et al.16 The placement of an oxidized cellulose polymer layer beneath the lifted membrane can be beneficial for isolating the bovine hydroxyapatite. In addition, oxidized cellulose polymer layer adheres to and seals the sinus membrane, which may explain the absence of infections in the present patients, but further studies are needed.
There are no major differences between our implant success rate and those obtained by other authors. Thus, the global success rate reported by Cho-Lee et al. in their retrospective study of different filling materials was 96.91%, in comparison to 93.1% in the present study. However, in contrast to our series, the mean height before treatment was 6.59mm, enabling immediate implant placement in 64.7% of the patients due to the higher primary stability that could be achieved. In the present study, in which the mean height was much lower (3.1mm), only 13.4% of implants could be placed in the same surgical act. Sakka et al. obtained a 94.8% success rate in patients undergoing sinus augmentation with parietal bone filling.17 In 2011, Herrero et al.16 achieved an implant success rate 96.4% but the mean presurgical height, which was not reported, was likely much greater than in the present study, given that an immediate implant could be placed in 89.53% of their cases.
Chen only places immediate dental implants in a sinus with at least 5 mm.18
Our implant success in severely resorbed sinuses using bovine hydroxyapatite alone is within the range reported by other authors. This procedure does not require general anesthesia and avoids patient morbidity.
According to these study findings, sinus augmentation with bovine hydroxyapatite alone is a safe surgical technique that yields a very high implant success rate. This approach is not associated with any donor morbidity and achieves the predictable rehabilitation of patients with absence of posterior sectors in a severely atrophied maxilla. Histological and histomorphometrical analysis would be helpful in order to obtain the bone gain.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe authors declare that there is no external funding.
Conflicts of interestThe authors declare that they have no conflicts of interests.