Neck chordomas are rare, slow growing, but locally destructive tumors. Most tumors arise in male patients, rarely metastasize and have a high recurrence rate.
ObjectiveTo describe the evolution of a neck chordoma for over twenty years and discuss the appropriate therapeutic options.
Story of caseFemale patient, 62 years old, with a history of multiple recurrences of neck chordoma, initially diagnosed by a swelling on the superior and lateral wall of the oropharynx. She underwent several surgical approaches, one of which was complemented with external beam radiotherapy, one of them being paliative.
ConclusionConsidering the high rate of recurrence of this tumor, the surgical team must be empowered to perform different routes for surgical approach, minimizing the risks and complications.
Los cordomas cervicales son tumores poco frecuentes, de crecimiento lento, pero destructivos localmente. Afectan con más frecuencia al sexo masculino, rara vez metastatizan y se asocian a una elevada tasa de recidivas.
ObjetivoDescribir la evolución de un cordoma cervical durante más de 20 años, y abordar las opciones terapéuticas más apropiadas.
Caso clínicoPaciente de sexo femenino, de 62 años de edad, con antecedentes de múltiples recidivas de un cordoma cervical, cuyo diagnóstico inicial se estableció por la inflamación de la porción superior y pared lateral de la orofaringe. Se sometió a diversos procedimientos quirúrgicos, uno de los cuales se complementó con radioterapia de haz externo, en una ocasión con intención paliativa.
ConclusiónDebido a la elevada tasa de recidivas de este tumor, es preciso que el equipo quirúrgico cuente con la formación, aprendizaje y experiencia apropiados para tomar decisiones sobre la vía de abordaje quirúrgico óptima de este tumor debe estar facultada para realizar las diferentes vías de abordaje quirúrgico, lo que reducirá a un mínimo los riesgos y complicaciones.
Chordomas are slow-growing malignant neoplasms. They correspond to about 5% of all primary bone tumors. They originate from the axial skeleton with increased frequency in the region of the sacrum (50%), then the base of the skull (35%) and neck chordomas are not common a presentation.1 Differential diagnosis is made with chondrosarcoma, pituitary tumor, schwannomas, metastases or nasopharyngeal carcinoma. Most of these tumors are found in males between 30 and 70 years of age, rarely metastasize and have a recurrence rate of about 29%.1
The aim of this paper is to describe the evolution of a neck chordoma in two decades of clinical follow-up, as well as, the therapeutic attitudes used according to the topography of the recurrence.
Case reviewFemale patient currently aged 62 years old. In 1989, she attended an otorhinolaryngology clinic by a foreign body sensation in the oropharynx of progressive onset, with about 6 months of evolution. She denied other relevant complaints. The physical exam showed a lump in the lateral aspect in the left of the oropharynx wall, in its uppermost part, projecting cranially to the nasopharynx. The mucosa was of normal appearance and the rest of the exam showed no significant changes.
The neck CT described a cervical lesion in the left parapharyngeal region with approximately 15mm×15mm, with foci of calcification within and with contrast enhancement. It showed no signs of medullar and/or intracranial invasion. It was made a surgical excisional biopsy by transoral route and the diagnosis was a conventional chordoma with a lobular growth pattern. The surgical margins were free of tumor.
In 1991, the patient had a recurrent lesion in a topography similar to the previous, although slightly larger, centered on C3. It was carried out, at this time, a left cervical approach. Histopathology showed that the surgical margins were not free of the tumor. The treatment was complemented with external beam radiation with 60Gy for 5 months and the response was favorable.
After six years, the lesions appeared again as a bulging of the left lateral wall of the oropharynx. The imaging scan showed a lesion centered on C1, but now with signs of bone invasion. No signs of spinal cord involvement. It was then carried out a surgical intervention through a paramedian transmandibular approach centered on the chin, combined with a modified Wilson transpalatine approach.
In 1998, a new swelling is observed now in the posterior oropharyngeal wall with about 15mm×10mm that was approached transorally.
After five years a new suspect focus appeared near the deep lobe of the left parotid, extending to the posterior wall of the oropharynx and with extension to nasopharynx. It was decided, at this stage, for a new approach with transpalatine Wilson incision.
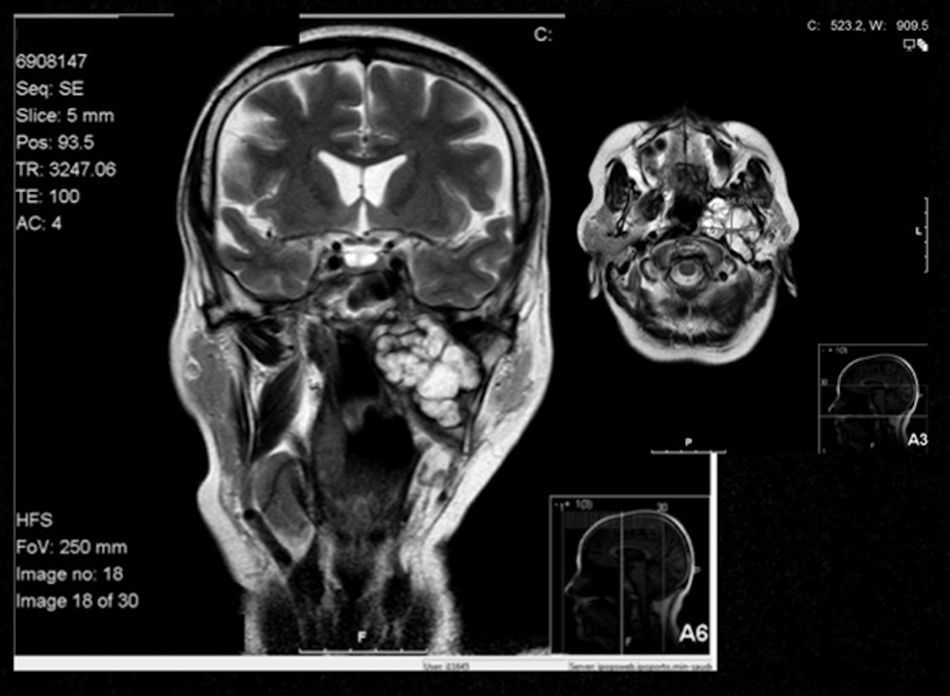
In 2011, a new tumor was evident in the left aspect of the nasopharynx with extension into the ipsilateral masticator space (Fig. 1). It was approached by a way of mandibulotomy centered to the chin already described.
In all histological exams, the diagnosis was always of a conventional chordoma, and except for an episode mentioned above, the surgical margins were free of tumor.
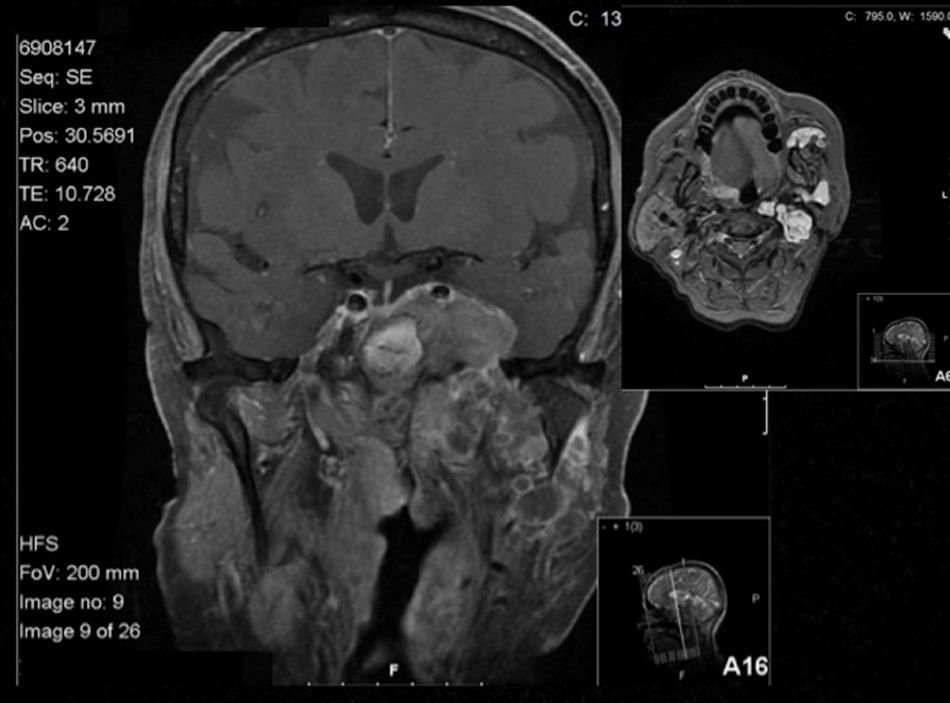
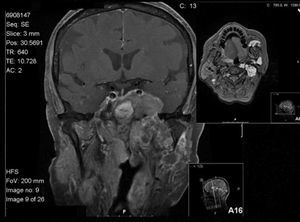
One year after this surgery, the lesion recur, but this time with intracranial extension. The tumor invaded the left paraselar region with extension into the cavernous sinus and trigeminal ganglion. It encased the internal carotid anterior, and anteriorly it invaded the paranasal sinuses and laterally the temporal lobe (Fig. 2). After multidisciplinary consultation, it was decided to do palliative radiation therapy.
DiscussionVirchow, in the 19th century, was the first to describe a chordoma, calling it as Ecchordosis Phisaliphora. Later, Ribbert describes the origin of this neoplasm as the notochord remnant.2
Symptoms depend on the point of origin of the tumor and the prognosis depends on the size and topography. These tumors are rare, slow growing and can be highly invasive and locally destructive.2
This case describes the challenges of this entity highlighting the different routes of surgical approach and emphasizes the high rate of recurrence.2,3
The neck chordomas are rare and the extension to the pharynx is even rarer. Depending on their origin, the skull base chordomas are locally aggressive. The treatment is surgical excision of the lesion. However, depending on location, this can be difficult to achieve.4The radiation therapy is recommended when it is not possible to perform as en bloc excision, in cases of tumor persistence after surgical removal, as well as in cases of recurrence.5–7
In this case, radiotherapy was performed initially by the persistence and because it was a local recurrence. There were no complications with the treatment. The other relapses were always handled by different types of surgical approaches combining various routes and thus it was possible to remove the initial tumor as well as all the recurrences with little comorbidity.
Except for the last tumor recurrence, which was handled with palliative radiation therapy due to inoperability of the lesion.
The transpalatine approach to the nasopharynx was first described in 1951 by Wilson and allows exposure of the nasopharynx, the clivus and to the posterior aspect of the nasal cavity.8
Surgical approaches involving median or paramedian mandibulotomies enable a way to reach to parapharyngeal space by sectioning of the superior pharyngeal constrictor muscle.9
Through the description of this clinical case, the authors show that there is a significant likelihood of recurrence with this type of tumor, possibly by the persistence of tumor cells in the surgical field or through the dissemination of the tumor cells in the operative field, which given the characteristics of slow growth of these tumors are manifested at intervals that can be rather far apart from each other.10,11
ConclusionThe selection of the surgical approach with these tumors should be appropriate to the location and, as a principle, should start with the least complex and disabling, to the most complex. This was the method used here, allowing the patient, throughout this time, to have a good quality of life without any neurological deficit.
It is of utmost importance to have a multidisciplinary approach to this type of tumor because of its appreciable recurrence rate.
On this basis, the authors conclude that surgical teams should be trained and qualified to perform different surgical approaches to allow the adequate surgical excision of these tumors, taking into account its location and size.
Protección de personas y animalesLos autores declaran que para esta investigación no se han realizado experimentos en seres humanos ni en animales.
Confidencialidad de los datosLos autores declaran que en este artículo no aparecen datos de pacientes.
Derecho a la privacidad y consentimiento informadoLos autores declaran que en este artículo no aparecen datos de pacientes.