To present a case of sclerosing polycystic adenosis (SPA) of the parotid gland, highlighting the probable etiology and the benign behavior of these cases.
Case reportA woman of 22 years old had a right parotid mass with a slowly progressive growth associated with a chronic infection due to Epstein–Barr virus. Initially, it was asymptomatic and subsequently the patient developed light dysesthesias in the region. A superficial parotidectomy was done and the microscopic study informed SPA.
ConclusionThe SPA is similar to the fibrocystic changes, sclerosing adenosis and adenoid tumors of the mammary gland. The main location of the SPA is the parotid gland and it is considered a disease due to a pseudotumoral inflammatory reaction with a possible association with the Epstein–Barr virus. There is evidence that monoclonal cell populations exist. The treatment consists in excision of the tumor with a superficial parotidectomy, which has demonstrated high cure rates.
Presentar un caso de adenosis poliquística esclerosante (APE) de la glándula parótida, destacando la etiología probable y el comportamiento benigno de estos casos.
Caso clínicoMujer de 22 años con una masa parotídea derecha de crecimiento lentamente progresivo asociada con una infección crónica por el virus de Epstein–Barr. Inicialmente, era asintomática y posteriormente desarrolló disestesias ligeras en la región. Se realiza una parotidectomía superficial y el resultado histopatológico es de APE.
ConclusiónLa APE muestra cambios histopatológicos similares a los hallados en la enfermedad fibroquística, adenosis esclerosante y los tumores adenoideos de la glándula mamaria. La ubicación salivar principal de la APE es la glándula parótida y se trata de una enfermedad causada por una reacción inflamatoria pseudotumoral con una posible asociación con el virus de Epstein–Barr. Hay pruebas de que existen poblaciones celulares monoclonales. El tratamiento de elección es quirúrgico, siendo la parotidectomía superficial la técnica de elección al haber demostrado tasas de curación elevadas.
The parotid gland tumors are classified according to their morphological and histological patterns. The most common site of presentation of a salivary neoplasm is the parotid gland. The 85% of these neoplasms are benign tumors, being the pleomorphic adenoma the most frequent type.1
Sclerosing polycystic adenosis (SPA) is a rare disease of the salivary glands, first described by Smith et al. at 1996.2 The SPA is similar to the fibrocystic changes, sclerosing adenosis and adenoid tumors of the mammary gland.3,4 The main location of the SPA is the parotid gland, but there are reported cases in the submandibular and accessory salivary glands too2
Case reportA woman of 22 years old with no pathologic family history has a negative IgM, but with a positive IgG Epstein–Barr serum antibody test. The patient went to the ENT because of a right parotid mass with a slowly progressive growth of 8 months. Initially, it was asymptomatic and subsequently the patient developed light dysesthesias in the region.
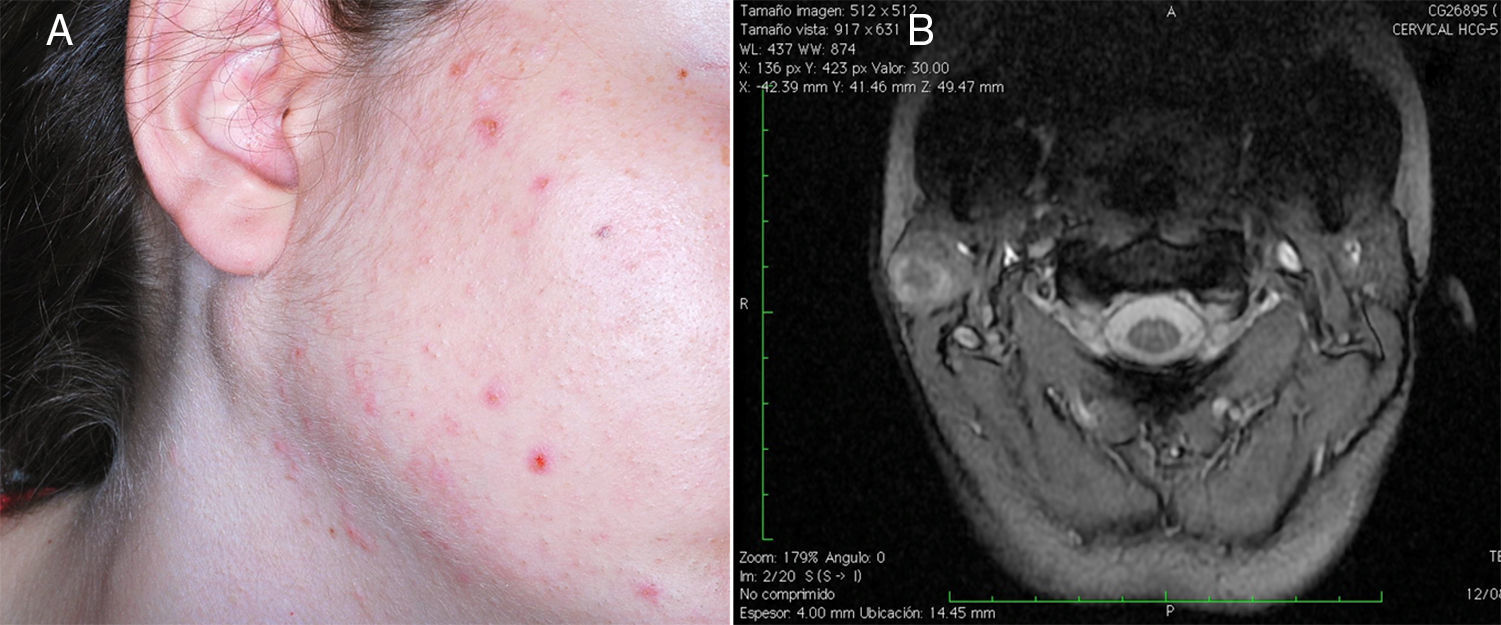
A physical examination was done. A hard, painless, non-fluctuating tumor of 2cm×2cm of maximum diameter was revealed, posterior to the right angle of the jaw, and without trophic changes in the skin. In the T2 of the MRI it is confirmed a 2cm×1.8cm in diameter mass in the tail of the right parotid with hyperintense areas inside the gland, but without spreading to adjacent structures (Fig. 1A and B). Fine needle aspiration cytology was performed to orientate the diagnosis, having a histopathologic result of chronic sialadenitis.
A mass of 2cm×2cm of maximum diameter was revealed, posterior to the right angle of the jaw (A). Axial T2 MRI image of the neck, it is confirmed a 2cm×1.8cm in diameter tumor in the tail of the right parotid, with hyperintense areas inside the gland but without evidence of extension to adjacent structures (B).
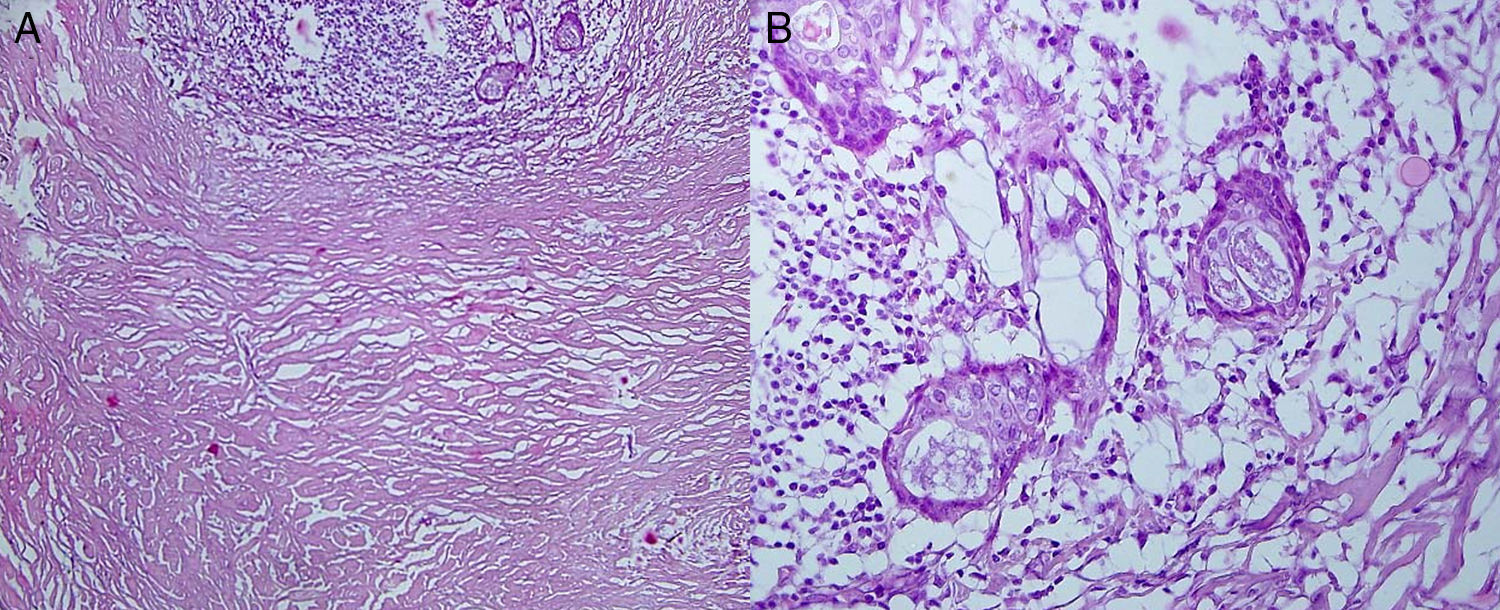
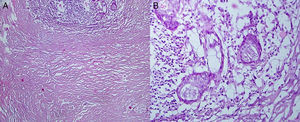
The provisional probable diagnosis was a parotid tumor with a clinical and radiological benign behavior, likely a pleomorphic adenoma. Therefore a preauricular parotidectomy was done by cervical incision, removing the supra-facial portion of the right parotid gland. The microscopic study informed glandular parenchyma in continuity with a dense-hyaline connective tissue with undefined borders that forms a sclerosing-hyaline stroma mass with inflammatory cells and interposed myoepithelial elements. No nuclear atypia of the ductal and squamous epithelium was revealed (Fig. 2A and B). This is suggestive of sclerosing polycystic adenosis (SPA) of the parotid gland. At one year of follow-up, the patient is asymptomatic, with a favorable clinical outcome and without tumor relapse.
The microscopic study reveal a parotid gland tissue with periductal inflammation and fibrosis with intraluminal cellular debris and polymorphic nuclear cells. This glandular parenchyma appears in continuity with a dense-hyaline connective tissue with undefined borders that forms a sclerosing-hyaline stroma mass with inflammatory cells and interposed myoepithelial elements. (H&E; original magnification, 10×: A). A microscopic image with more detail reveals there is no presence of nuclear atypia of the ductal and squamous epithelium (H&E; original magnification, 100×: B).
There have been about 51 cases of sclerosing polycyst adenosis (SPA) in the salivary glands published. All cases of SPA have been unilateral like this case report.5
These tumors are diagnosed at a mean age of 40 years and the mean tumor size is in the range of 0.3–6cm. The clinical picture is nonspecific, presenting in most cases as a progressively growing intraparotid asymptomatic mass, although in some cases the tumor has been associated with pain and/or paresthesias in the region.2,6
These tumors are usually single, well-defined and partially encapsulated. There are few cases of SPA that have become multinodular. Moreover, there have been cases associated with mandibular pleomorphic adenomas, parotid oncocytomas or Whartin tumors.2,6
The pathogenesis of SPA is unknown, although there has been a possible association with the Epstein–Barr virus7 and in this particular case there is a history of chronic infection with this virus. Furthermore, there is evidence that monoclonal cell populations exist in some cases of SPA, however the meaning of this clonality is still uncertain. There is no gender predominance, although it is considered a slight predilection toward females.7
SPA is considered a disease due to a pseudotumoral inflammatory reaction. However because of the risk of recurrence and the presence of cell clonality it has been considered that it might have a tumoral origin.2
There are few descriptions of radiology because of the rarity of the tumor, but in the majority of cases it has been described a parotid mass with small cystic areas which are hyperintense on contrast-enhanced T2 MRI. In the ultrasound, it is described as a hypoechoic lesion, with well demarcated micro-cystic areas.7
Microscopically the SPA consists of lobes circumscribed by hyaline connective tissue. Moreover, within the fibrous tissue there is hyperplastic ductal and acinar epithelium with no differentiation.7,8 There has not been observed carcinomatous degeneration so far. Specific immunohistochemistry antibodies as anti-smooth muscle actin, can confirm the integrity of the myoepithelial cells layer in benign tumors, which is lost in carcinomatous lesions.2
Progesterone receptors have been demonstrated in 80% of epithelial cells and in 20% of cases there have been estrogen receptors in the dysplasic spotlights of ductal cells. Cytokeratin has been observed in the tubuloacinar elements and S-100, smooth muscle actin, and calponin stain is present in the myoepithelial cells.5
There are few diagnosed cases by fine needle cytology, in which cases there are found syncytial cells of epithelial ducts with apocrine changes.3,8 The differential diagnosis should include acinar cell carcinoma, sclerosing sialadenitis, salivary ductal carcinoma and adenocarcinoma.6 Mild dysplasia is reported in up to 30% of the cases and in about 10% there has been found a low grade in situ carcinoma.1
The treatment in most cases consists of excision of the tumor with a superficial parotidectomy with adequate surgical margins and facial nerve sparing, which has demonstrated a prolonged survival.2,4 Recurrences are rare and usually due to incomplete surgical excision or occult multifocal disease rather than a real recurrence.7 Local recurrence appeared between 19 and 30% of all cases.4,5 There are no documented metastases or associated mortality due to the SPA.8
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare no conflict of interest.