Tuberculosis (TB) is a contagious infectious disease caused by Mycobacterium tuberculosis (Koch's bacillus). Co-infection with human immunodeficiency virus (HIV) and TB has reached a significant importance as a public health problem and this association has been recognized as the most significant event that changed “the balance between man and Koch's bacillus” in the last century, and has a large contribution to the risk for disease spreading. Tuberculosis has two main standard categories of clinical manifestations: primary and secondary. Primary TB is responsible for the initial infection with lungs being the involved organ. Oral lesions are observed as a secondary TB clinical manifestation with most frequent sites being hard and soft palate, tongue, lips, gums, tonsils, and salivary glands. A case of classical TB lesions in the oral cavity is reported, and the importance of a correct diagnosis through careful history taking is emphasized. Treatment selection needs to be done assertively, with great determination and building a link between patient and treatment protocol, in order to promote patient's adherence.
La tuberculosis (TB) es una enfermedad infecciosa contagiosa causada por Mycobacterium tuberculosis (bacilo de Koch). La coinfección del Virus de Inmunodeficiencia Humana (VIH) con TB son problemas de salud pública graves, además que esta asociación ha sido identificado como el evento más significativo que cambió “el equilibrio entre el hombre y el bacilo de Koch” en el último siglo y es crucial en el riesgo de propagación de la enfermedad. La tuberculosis se manifiesta en dos estándares: primaria y secundaria; el primario es responsable de la infección inicial y el órgano de elección es el pulmón. Las lesiones orales se observan a nivel secundario y los sitios más frecuentes son el paladar duro y blando, lengua, labios, encías, amígdalas y las glándulas salivales. Esta revisión presenta un caso con lesiones clásicas de tuberculosis en la cavidad bucal haciendo hincapié en la importancia de un correcto diagnóstico a través de la anamnesis. El tratamiento se debe hacer con la seguridad, la determinación y la formación de enlaces que facilitan la adherencia del paciente al tratamiento.
Tuberculosis (TB) is a chronic infectious granulomatous disease caused by the aerobic bacillus Mycobacterium tuberculosis, called Koch's bacillus discovered by Robert Koch in 1882.1–4
Tuberculosis is a major public health concern especially in Asia and Africa, and is still among the most life-threatening infectious diseases, resulting in high mortality risk in adults. With a prevalence of 9.2 million new cases diagnosed, in the world, which occurred 1.7 million tuberculosis deaths in 2006, and was possible to notice that 0.7 million cases and 0.2 million deaths were in HIV positive.5,6 The WHO report of 2008 showed the expected incidence of 9.4 million TB cases, about 139 cases per 100,000 individuals; This represents an increase of 100 thousand new cases in 2007.7,8 Interestingly, there seems to be a high rate of co-infection that includes TB and HIV patients, responsible for almost 28% of tuberculosis deaths.8,9 The countries with the largest number of cases in 2009 were India and China. Tuberculosis in India is a public health problem, with a fifth (21%) of all TB cases in the world.10
There is a relation between the disease intense growth with the acquired immunodeficiency syndrome (AIDS) by the population affected, due to the T lymphocyte issue, the largest component of the cellular immune response against M. tuberculosis, causing serious implications.1,3,4 The infections are the result of bacillus spread directly from person to person, transmitted by an individual with an active disease.1,3,11
The infection is distinguished by two phases: primary and secondary. The primary tuberculosis is mild, manifesting with fever, chills, cough and sputum production.1,3,11 Microorganisms produce initially a non-specific inflammatory chronic reaction. In most individuals, primary infection results from a local fiber calcified nodule, situated in the initial site of involvement. However, live microorganisms may be present in these nodes and remain dormant for many years, until some other episode of immunosuppression happens and the disease can be activated.11
Only about 5–10% of TB patients’ progress from infection to active disease and a coexisting immunosuppression is often responsible. In rare situations, active TB may manifest on primary infection. However, the disease activation usually develops in other stages, from the reactivation of the microorganism in a previously infected person, such reactivation is characteristically associated with a compromised host defense system, it may cause lung disease and is called secondary tuberculosis. Granulomatous lesions may promote diffuse dissemination through the vascular system by tubercle bacilli, which may result in liver, renal, gastrointestinal and meninges involvement.1,3,11,12
The extrapulmonary tuberculosis is about 25% of TB lesions, 10–35% are found in the region of the head and neck and 0.2–1.5% in the oral cavity.8 The most common extrapulmonary regions in the head and neck are the cervical lymph nodes, followed by the larynx and ear. The regions much less common are nasal cavity, nasopharynx, oral, parotid gland, esophagus and spine.11
In the last two decades due to decreased treatment adherence and control of TB cases and with the advent of AIDS, there is the development of multi-resistant of Koch bacillus, occurring gradually, increasing the number of diseases cases, resulting in pharyngo-laryngeal lesions, associated or isolated.13
The tuberculosis lesions in the oral cavity are rare and may occur anywhere, being more frequent in tongue, palate, lips, mucosa, gums, brake, jaw bones, periapical region, tonsils, uvula, pharynx and larynx can manifest as a chronic irregular ulcer, shallow or deep, painless, vegetating surface, with numerous yellowish submucosal points (granules of Trélat), tending to size increase slowly and progress to deep ulcers on the basis of purulent lesions, containing active microorganisms and highly infectious.3,8,10,11
The presentations include areas of nodular leukoplastic, it may also occur as a granuloma, osteomyelitis, or salivary gland disease.8
The oral lesions of primary tuberculosis usually involve gums, mucobucal sulcus and inflammation areas adjacent tooth extraction sites, and the secondary tuberculosis oral lesions occur in the tongue, palate and lips, and may involve the maxillary bones, occurring microorganism penetrations in the area and periapical inflammation through the bloodstream or through a pulp exposed to the oral environment.3 Usually it is associated with lymph node regionalized. The tuberculosis osteomyelitis in the jaw has been reported and appears as not defined radiolucent areas.3,11
It is important to note that infectious oral ulcers may present a similar shape to the other ulcerative oral cavity lesions, for that reason there is the need of microscopic diagnosis, in conjunction with tuberculin skin test (Mantoux), or sputum culture.8,10
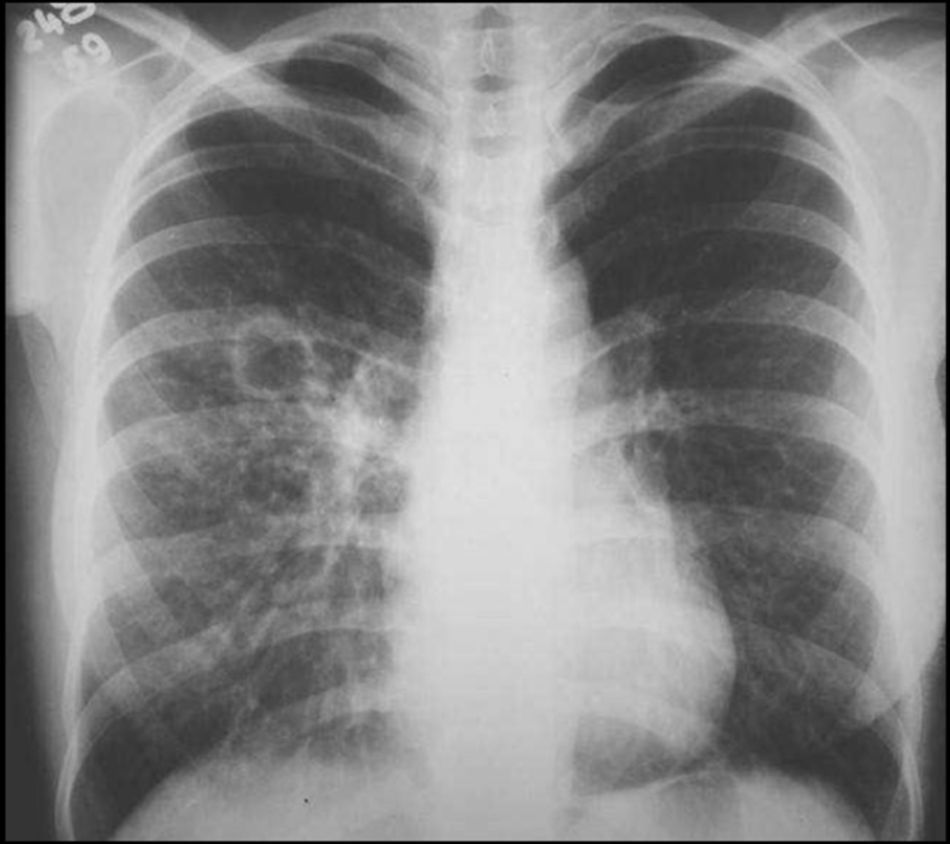
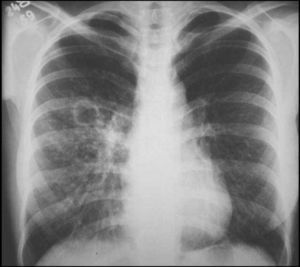
Case reportMale patient, 43 years old, dark skin, heterosexual, with incomplete college degree, married, referred to Center of Study and Treatment for Patients with Special Needs (CEAPE) – Paulista University – Indianapolis Campus – São Paulo – Brazil, anamnesis report showed illicit drugs addiction, alcoholic and smoking habits, with psychiatric diagnosis of Panic Disorder and fear of death, treated with Fluoxetine 20mg and Rivotril 2mg daily, intending to restart the treatment of neuro-tuberculosis and pulmonary tuberculosis for the third time, reporting to be bacillus resistant due to the lack of adherence to recommended treatment, because the patient had abandoned the treatment by choice every time clinical condition improved, occurring subsequent recurrence, exacerbated complication, aggravating the condition. Test values performed were done 2 months after showing lymphocyte CD4=75cells/mm3 blood and viral load 156,000copies per mm3 of blood. Dental treatment was done in our clinical service and this time sought solution to the oral lesion that assailed 2 weeks ago. During intraoral clinical examination, oral lesions were observed in hard and soft palate, in the oropharynx, extending tonsillar pillars, demonstrating painful irregular ulcer with yellowish points called nodules of Trélat, those injuries promote speech, swallowing and feeding problems, intensifying the drop in their immune resistance (Fig. 1). He also presented generalized lymphadenopathy in cervical chain, weight loss of 12 pounds in one year, hemoptysis constant, local pain, fever and cough. He reported that the treatment of tuberculosis associated with antiretroviral therapy (HAART), has previously caused side effects of allergic reactions maculopapular rash, elevated transaminases and later exacerbated effects of Stevens Johnson Syndrome, where once again the patient discontinued therapy, opposite the table shown at that time was reversed with Diprospan® (betamethasone dipropionate+betamethasone disodium phosphate) 3 ampoules intramuscular (IM) applied every 24h. The adjuvant treatment for oral lesions was the Elixir Dexamethasone (Decadron®) – 5 mouthwash twice a day for 2 days, on the second day began application of low power diode laser Gallium Aluminum Arsenide (GaAIAs) with a wavelength of 790nm, power 30mW, applied for 2min and 20s punctually, in each clinical lesion with energy density of 4J/cm2 each point. The next application had shown improvement of clinical features and the patient had reported comfort in the oral cavity, pain and burning decrease, facilitating swallowing and feeding (Fig. 2), laser therapy provided anti-inflammatory, analgesic, repair tissue and bactericidal. Oral treatment includes orientation for the patient to return to the medical service for urgent resumption of treatment and clinical follow-up. On a return visit, 20 days after 1st office visit he brought the new search results sputum positive culture for M. tuberculosis in 3 samples, research Baar also positive and chest's X-ray (Fig. 3). Other tests were also conducted to: Hepatitis C, Hepatitis B, toxoplasmosis, cytomegalovirus, syphilis, all negative. Currently patients do not follow HAART and tuberculosis therapy protocols correctly, making the number of extras occurrences grow. The antiretroviral medications administered are Efavirenz and Biovir, the complex B vitamin and thiamine, and anti-tuberculin drugs Rifampicin, Isoniazid and Ethambutol. The definition of preferred or alternative regimens followed three criteria: scientific rationale, efficacy, tolerability and clinical experience of the service that comes. After initiation of therapy, the patient presented an excellent grip, keeping the bond with the services and there was no negative complications that would lead to treatment dropout and further improvement was evident in the general and oral health, with weight gain, stimulating the proceed with the recommended treatment protocols.
HIV infection is an important modifier factor for increasing the incidence of clinic tuberculosis due to the alteration of T lymphocyte. The antituberculosis therapy is performed when the disease is active in other organs such as the lungs, the therapy of choice is still the Isoniazid (INH) and rifampin however there are many controversies regarding Isoniazid that may induce hepatotoxicity. During the treatment, tests should be frequent for liver function control, those with active disease need combination with chemotherapy.1,2 In addition, several factors have exacerbated the spread of the disease, such as tuberculosis transmission among people living in bad conditions or poor health systems, and bad public health infrastructure.11 We cannot disregard the impact of co-infection TB/HIV in patients life, since both diseases are developed over the years, and are able to bring many prejudices that influence significantly their life quality.3
If the professional suspects of any form of tuberculosis, the patient should be referred to the specialist for clinical and laboratory evaluation and oral lesions usually are solved with systemic treatment.4
Patients with disseminated tuberculosis are treated with INH, rifampin and pyrazinamide. Studies show that ethnicit, sex gender and age should be considered to decide about INH prescription.14
Oral lesions of tuberculosis are uncommon in most cases appearing as a chronic and painless ulcer, involving the region of gums, mucobucal sulcus and inflammatory areas adjacent tooth extraction sites, ulcers may be deep or shallow, tending to increase size slowly.1,11 Tongue ulcer may be the only manifestation of mycobacterial infection suggestive of tuberculosis in patients with HIV/AIDS, which may occur because of a recurrence episode of TB ganglionic.15
Most secondary infection causes lung injury. It is unclear whether the affection occurs from hematogenous spread or by exposure to contaminated catarrhal secretion. The discovery of active pulmonary tuberculosis as a result of the investigation of oral lesions occur, and it is not uncommon, and primary oral tuberculosis, without pulmonary involvement is rare.11
ConclusionTuberculosis transmission occurs through individuals infected, by aerosol, droplets and direct and indirect contact. In this situation, the dentist needs to be aware about Biosafety Universal Standards avoiding cross-contamination in workplace. It is important to consider tuberculosis as differential diagnosis of oral lesions. We emphasize the importance of a correct diagnosis considering anamnesis, devoid of fear and prejudices, improving the patient life quality, facilitating adherence to recommended treatments.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNone.
Patient consentThe patient signed the consent form.
Conflict of interestThe authors declare no conflict of interest.