Bone elongation with magnetic endomedullary nails (MEN) has been proposed as an advantageous alternative to other techniques, by eliminating the drawbacks of external fixation. The aim of this work is to analyse the results and assess the complications in a series of patients under the age of 18.
Material and methodsFrom 2014 to 2019, 31 elongations (23 femurs, 8 tibias) using MEN (Precice2®) have been performed in 28 patients younger than 18 (15 males and 13 females). In this observational retrospective study, only patients with follow-up longer than 18 months have been included. The average age has been 14.4 years (8–18). The most relevant aspects analysed have been: previous shortening/deformity, elongation/correction achieved and time to full weight bearing. Complications and re-interventions have also been assessed.
ResultsThe elongation achieved has been 5.5cm on average (3–8). In 28 elongations (90.3%) the planned goal of lengthening was achieved. The mean healing index (HI) was 1.1months/cm. More than half of elongations (55%) presented complications. Although they produced permanent sequelae in only two patients (7.1%), a total of 9 patients required re-intervention (13 operations). No infections were detected.
ConclusionsBone lengthening with MEN in individuals younger than 18 has achieved its goal in more than 90% of patients in an effective, accurate and safe manner. The use of MEN in this series has eliminated the need for external fixators and has successfully tutorized the operated segment. The high number of complications detected in this study remains a concern.
El alargamiento óseo con clavos endomedulares magnéticos (CEM) se plantea como alternativa ventajosa a otros alargamientos, al eliminar los inconvenientes de la fijación externa. El objetivo de este trabajo es analizar los resultados y valorar las complicaciones en una serie de pacientes menores de 18 años.
Material y métodosEntre 2014 y 2019 se han realizado 31 alargamientos con CEM tipo Precice2® (23 fémures, 8 tibias), en 28 pacientes menores de 18 años (15 varones y 13 mujeres). Este estudio retrospectivo observacional incluye pacientes con un seguimiento mayor de 18 meses. La edad media ha sido de 14,4 años (8-18). Los aspectos más relevantes analizados han sido: acortamiento/deformidad previos, alargamiento/corrección conseguidos y tiempo hasta carga completa. Además se han revisado las complicaciones y las reintervenciones.
ResultadosEl alargamiento conseguido ha sido de 5,5cm de media (3-8). En 28 alargamientos (90,3%) se ha conseguido (24) o superado (4) el objetivo planificado. El índice de curación medio fue de 1,1 meses/cm. Más de la mitad de los alargamientos (55%) han presentado alguna complicación. Aunque estas solo han dejado secuelas permanentes en 2 pacientes (7,1%), 9 de ellos han precisado reintervención (13 operaciones). No ha habido infecciones.
ConclusionesLa elongación ósea con CEM en pacientes menores de 18 años ha conseguido su objetivo en más de un 90% de los casos de manera eficaz, precisa y segura. En esta serie, los CEM han eliminado la necesidad de fijadores externos y han tutorizado eficazmente el segmento operado. La alta incidencia de complicaciones sigue siendo preocupante.
Gradual bone distraction is a widely used resource in reconstructive surgery of the locomotor system, primarily in shortening, deformities and defects of the long bones. These surgical techniques have evolved2 since the first bone lengthening procedures were performed in the early 20th century.1 However, their complication rates remain a concern,3 particularly those related to the long-term use of external fixation.4–6 The first fully implantable endomedullary distraction nails were developed in the 1990s with the aim of eliminating the need for external fixation and its drawbacks.3 These devices evolved until the considerably more reliable motorised nails with external electrical7 or magnetic control emerged,8,9 which are currently the most widely used. Although a drastic reduction in the problems inherent to external fixation has been achieved, bone elongation using these devices is not free of complications and new problems have arisen with their use.3
The aim of this work was to conduct a study of our first 31 elongations with a magnetic endomedullary nail (MEN) (Precice2®) in patients under 18 years of age and, from the results obtained in our series, to contrast the advantages attributed to these devices and to analyse the complications that occurred.
Material and methodsWe conducted a retrospective observational study in a series of 31 lower limb lengthenings with magnetic pins, in 28 patients under 18 years of age undergoing surgery between 2014 and 2019. The minimum follow-up was 18 months from the end of treatment (full unassisted weight bearing). The mean age of the included patients was 14.4 years (8–18).
The 31 operated segments (23 femurs and 8 tibias) corresponded to 15 males and 13 females. The aetiology of the shortening was congenital in 14 cases (52%) and dysplastic in 4 patients (14.3%).
The type of nailing used was 21 anterograde femoral trochanteric, 2 retrograde femoral and 6 anterograde tibial. In 2 tibias with missing ankles (one previously arthrodesed and one with severe deformity and degeneration) we used straight nails implanted through a transcalcaneal approach. In no case were nails implanted through open physes.
All patients underwent procedures of femoral or tibial lengthening with or without simultaneous acute angular correction, using a Precice2® titanium MEN (Nuvasive, San Diego, USA).
There was individualised preoperative planning for each case. For the lengthening with/without angular correction using MEN, preoperative measurements and analysis of the length discrepancy and deformity were taken using anteroposterior and lateral standing teleradiographs of the lower extremity. The elongation osteotomy was performed minimally invasively at the metaphyseal-diaphyseal level, except in the case of associated deformity, where the apex of the deformity required a different location. The dimensions of the implant were also considered: calibre, according to the diameter of the medullary canal and length, depending mainly on the level of osteotomy selected. The surgical technique was minimally invasive and guided by radioscopy to introduce the MEN and for the osteotomy10 and locking. In no case were active physes crossed when inserting the MEN, in either the femur or the tibia. In 8 cases, Poller screws were used when there was a risk of loss of correction during nail insertion or deformation of the segment, either due to poor bone quality or because of the stress expected with distraction.
In tibial elongations, a distal fibula osteotomy was always combined with fibular fixation in distal-third tibia with a tetra-cortical screw. If the expected tibial elongation exceeded 4cm, an Achilles tenotomy was also performed.
At 5–7 days postoperatively, following the principles of callotasis,11 distraction was started at a rate of 1 and 0.75mm/day in femur and tibia, respectively. Physiotherapy was always started between the 7th and 15th postoperative day with a general programme aimed at maintaining and, where appropriate, gaining joint movement and muscle power of the affected limb.
Only 3 patients were lengthened due to stature (pathological short stature), while the remaining patients had a length discrepancy: 24 due to a mean shortening of 4.5cm (2–10cm) and only one had a lengthening of 3cm. The lengthening target was a mean 5.5cm (3–8cm) for length discrepancies and 7.2cm for short stature (6.5–8cm).
Clinical and radiological follow-up took place periodically, every 15 days, over the distraction period and every month thereafter until consolidation, when full weight bearing of the limb was allowed.
In 2 cases in this series, the MEN remained implanted and immediate lengthening (“dormant nail”) did not proceed for different reasons. In these cases, a circumferential osteotomy with a Gigli saw was necessary before starting distraction.
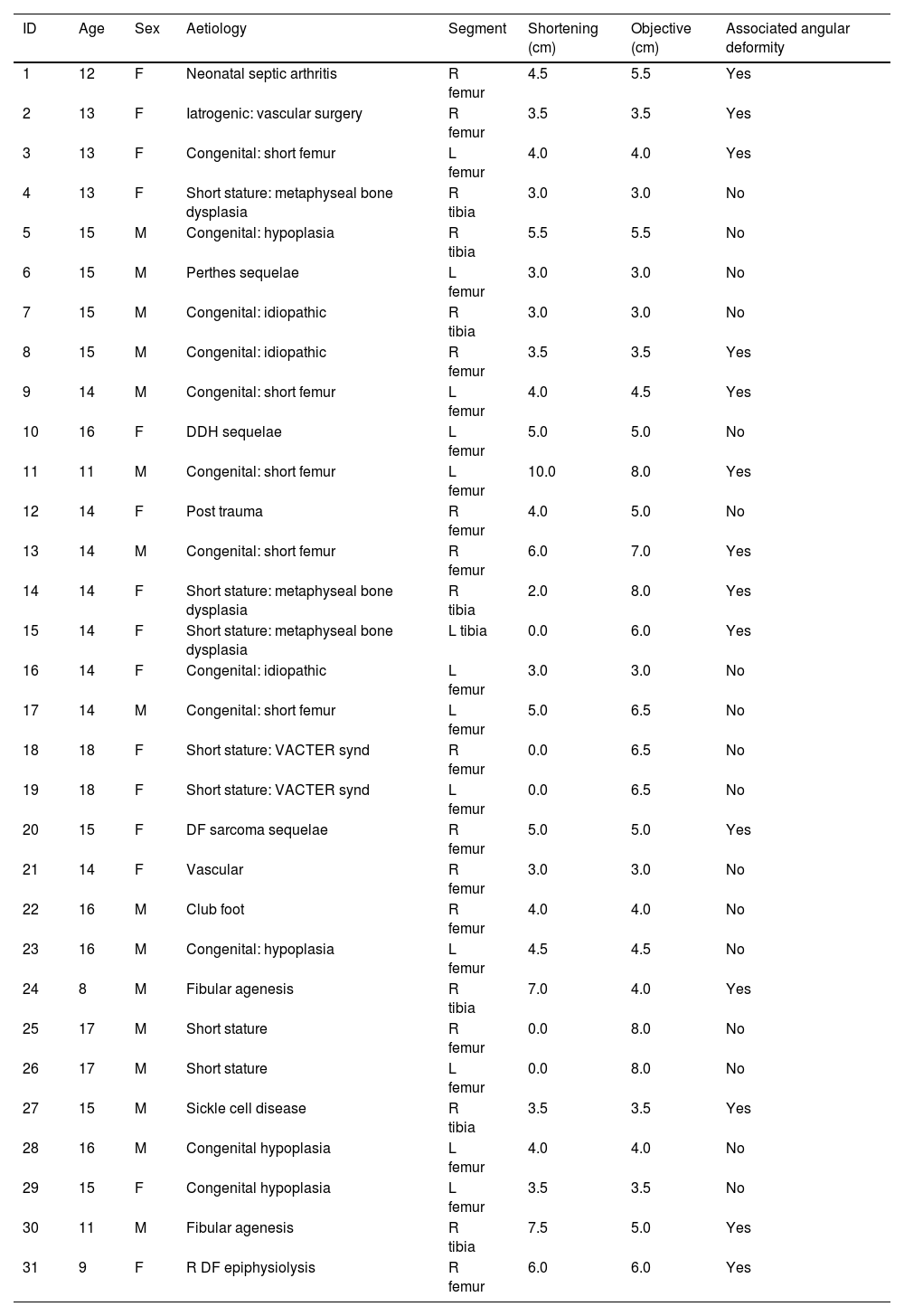
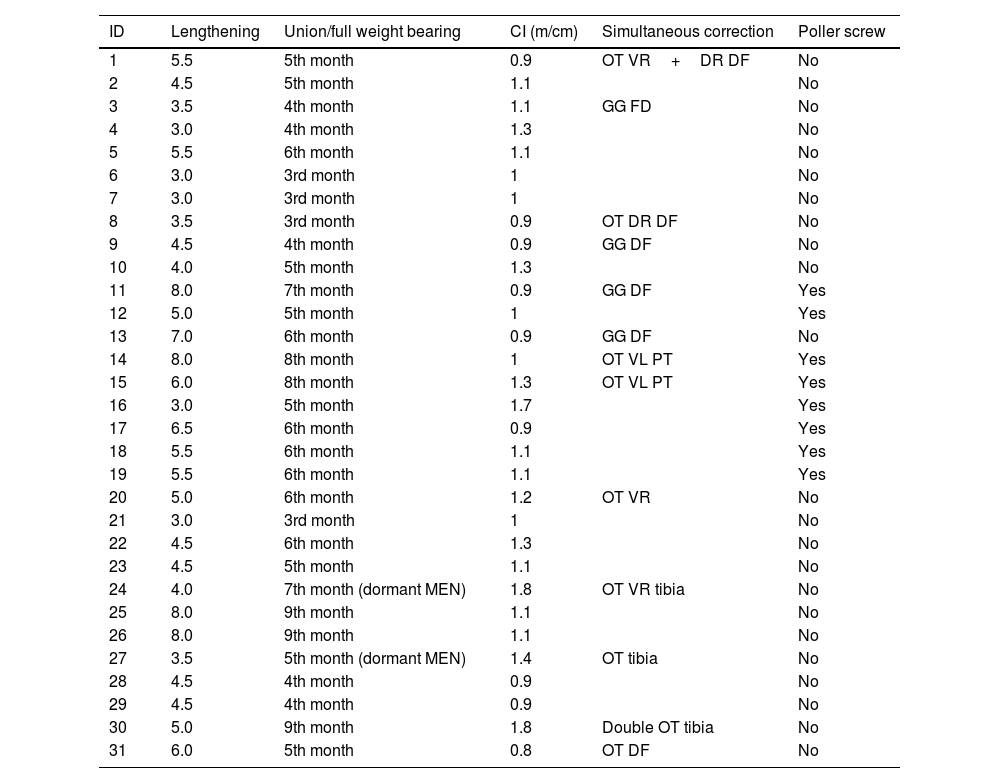
The most relevant aspects and data analysed in our series were previous shortening/deformity, lengthening/correction achieved, time to full weight bearing (Table 1) and the consolidation index (CI), ratio between months to consolidation and centimetres achieved (Table 2).
Demographics.
| ID | Age | Sex | Aetiology | Segment | Shortening (cm) | Objective (cm) | Associated angular deformity |
|---|---|---|---|---|---|---|---|
| 1 | 12 | F | Neonatal septic arthritis | R femur | 4.5 | 5.5 | Yes |
| 2 | 13 | F | Iatrogenic: vascular surgery | R femur | 3.5 | 3.5 | Yes |
| 3 | 13 | F | Congenital: short femur | L femur | 4.0 | 4.0 | Yes |
| 4 | 13 | F | Short stature: metaphyseal bone dysplasia | R tibia | 3.0 | 3.0 | No |
| 5 | 15 | M | Congenital: hypoplasia | R tibia | 5.5 | 5.5 | No |
| 6 | 15 | M | Perthes sequelae | L femur | 3.0 | 3.0 | No |
| 7 | 15 | M | Congenital: idiopathic | R tibia | 3.0 | 3.0 | No |
| 8 | 15 | M | Congenital: idiopathic | R femur | 3.5 | 3.5 | Yes |
| 9 | 14 | M | Congenital: short femur | L femur | 4.0 | 4.5 | Yes |
| 10 | 16 | F | DDH sequelae | L femur | 5.0 | 5.0 | No |
| 11 | 11 | M | Congenital: short femur | L femur | 10.0 | 8.0 | Yes |
| 12 | 14 | F | Post trauma | R femur | 4.0 | 5.0 | No |
| 13 | 14 | M | Congenital: short femur | R femur | 6.0 | 7.0 | Yes |
| 14 | 14 | F | Short stature: metaphyseal bone dysplasia | R tibia | 2.0 | 8.0 | Yes |
| 15 | 14 | F | Short stature: metaphyseal bone dysplasia | L tibia | 0.0 | 6.0 | Yes |
| 16 | 14 | F | Congenital: idiopathic | L femur | 3.0 | 3.0 | No |
| 17 | 14 | M | Congenital: short femur | L femur | 5.0 | 6.5 | No |
| 18 | 18 | F | Short stature: VACTER synd | R femur | 0.0 | 6.5 | No |
| 19 | 18 | F | Short stature: VACTER synd | L femur | 0.0 | 6.5 | No |
| 20 | 15 | F | DF sarcoma sequelae | R femur | 5.0 | 5.0 | Yes |
| 21 | 14 | F | Vascular | R femur | 3.0 | 3.0 | No |
| 22 | 16 | M | Club foot | R femur | 4.0 | 4.0 | No |
| 23 | 16 | M | Congenital: hypoplasia | L femur | 4.5 | 4.5 | No |
| 24 | 8 | M | Fibular agenesis | R tibia | 7.0 | 4.0 | Yes |
| 25 | 17 | M | Short stature | R femur | 0.0 | 8.0 | No |
| 26 | 17 | M | Short stature | L femur | 0.0 | 8.0 | No |
| 27 | 15 | M | Sickle cell disease | R tibia | 3.5 | 3.5 | Yes |
| 28 | 16 | M | Congenital hypoplasia | L femur | 4.0 | 4.0 | No |
| 29 | 15 | F | Congenital hypoplasia | L femur | 3.5 | 3.5 | No |
| 30 | 11 | M | Fibular agenesis | R tibia | 7.5 | 5.0 | Yes |
| 31 | 9 | F | R DF epiphysiolysis | R femur | 6.0 | 6.0 | Yes |
This table presents the most relevant data analysed in our case series.
DDH: developmental dysplasia of the hip; DF: distal femur; F: female; L: left; M: male; R: right; Synd: syndrome.
Series results.
| ID | Lengthening | Union/full weight bearing | CI (m/cm) | Simultaneous correction | Poller screw |
|---|---|---|---|---|---|
| 1 | 5.5 | 5th month | 0.9 | OT VR+DR DF | No |
| 2 | 4.5 | 5th month | 1.1 | No | |
| 3 | 3.5 | 4th month | 1.1 | GG FD | No |
| 4 | 3.0 | 4th month | 1.3 | No | |
| 5 | 5.5 | 6th month | 1.1 | No | |
| 6 | 3.0 | 3rd month | 1 | No | |
| 7 | 3.0 | 3rd month | 1 | No | |
| 8 | 3.5 | 3rd month | 0.9 | OT DR DF | No |
| 9 | 4.5 | 4th month | 0.9 | GG DF | No |
| 10 | 4.0 | 5th month | 1.3 | No | |
| 11 | 8.0 | 7th month | 0.9 | GG DF | Yes |
| 12 | 5.0 | 5th month | 1 | Yes | |
| 13 | 7.0 | 6th month | 0.9 | GG DF | No |
| 14 | 8.0 | 8th month | 1 | OT VL PT | Yes |
| 15 | 6.0 | 8th month | 1.3 | OT VL PT | Yes |
| 16 | 3.0 | 5th month | 1.7 | Yes | |
| 17 | 6.5 | 6th month | 0.9 | Yes | |
| 18 | 5.5 | 6th month | 1.1 | Yes | |
| 19 | 5.5 | 6th month | 1.1 | Yes | |
| 20 | 5.0 | 6th month | 1.2 | OT VR | No |
| 21 | 3.0 | 3rd month | 1 | No | |
| 22 | 4.5 | 6th month | 1.3 | No | |
| 23 | 4.5 | 5th month | 1.1 | No | |
| 24 | 4.0 | 7th month (dormant MEN) | 1.8 | OT VR tibia | No |
| 25 | 8.0 | 9th month | 1.1 | No | |
| 26 | 8.0 | 9th month | 1.1 | No | |
| 27 | 3.5 | 5th month (dormant MEN) | 1.4 | OT tibia | No |
| 28 | 4.5 | 4th month | 0.9 | No | |
| 29 | 4.5 | 4th month | 0.9 | No | |
| 30 | 5.0 | 9th month | 1.8 | Double OT tibia | No |
| 31 | 6.0 | 5th month | 0.8 | OT DF | No |
This table shows the lengthening achieved (cm), time to full weight bearing, consolidation index (CI) and simultaneous angular corrections and the use of Poller screw during the operation.
DR: derotational; DF: distal femur: GG: guided growth; OT: osteotomy; PT: proximal tibia; VL: valgus; VR: varus.
One year after the start of full weight bearing, patients/families completed a simple satisfaction questionnaire to subjectively evaluate the result obtained (very satisfied/satisfied/not very or not at all satisfied) and implant tolerance (good/fair/poor); they were also asked if they would undergo the surgery again if necessary.
ResultsIn the series studied, the MEN functioned correctly and accurately in all cases, and the reading on the remote-control unit (RCU) and the lengthening achieved consistently agreed. The mean lengthening was 5.5cm (3–8cm): 4.56cm in patients with length discrepancy and 6.8cm in patients lengthened for height. In 22 lengthenings the target was similar to the initial length discrepancy and only in 9 cases was the target different: in 3 cases (congenital) it was less, to avoid risks due to excess stress and/or to favour consolidation or due to the MEN's own capacity, while in 6 cases over-lengthening was planned to minimise length discrepancy at maturity. In 28 lengthenings (90.3%) the planned objective was achieved; however, in 3 of them it was necessary to lengthen more than planned to compensate for the length discrepancy and in another case, there was overlengthening of 1cm by error, which had no clinical repercussions. In 2 patients (3 segments) the target was not reached. One of them due to a femoral fracture, which caused a loss of lengthening of 1cm, and in another case due to psychological intolerance.
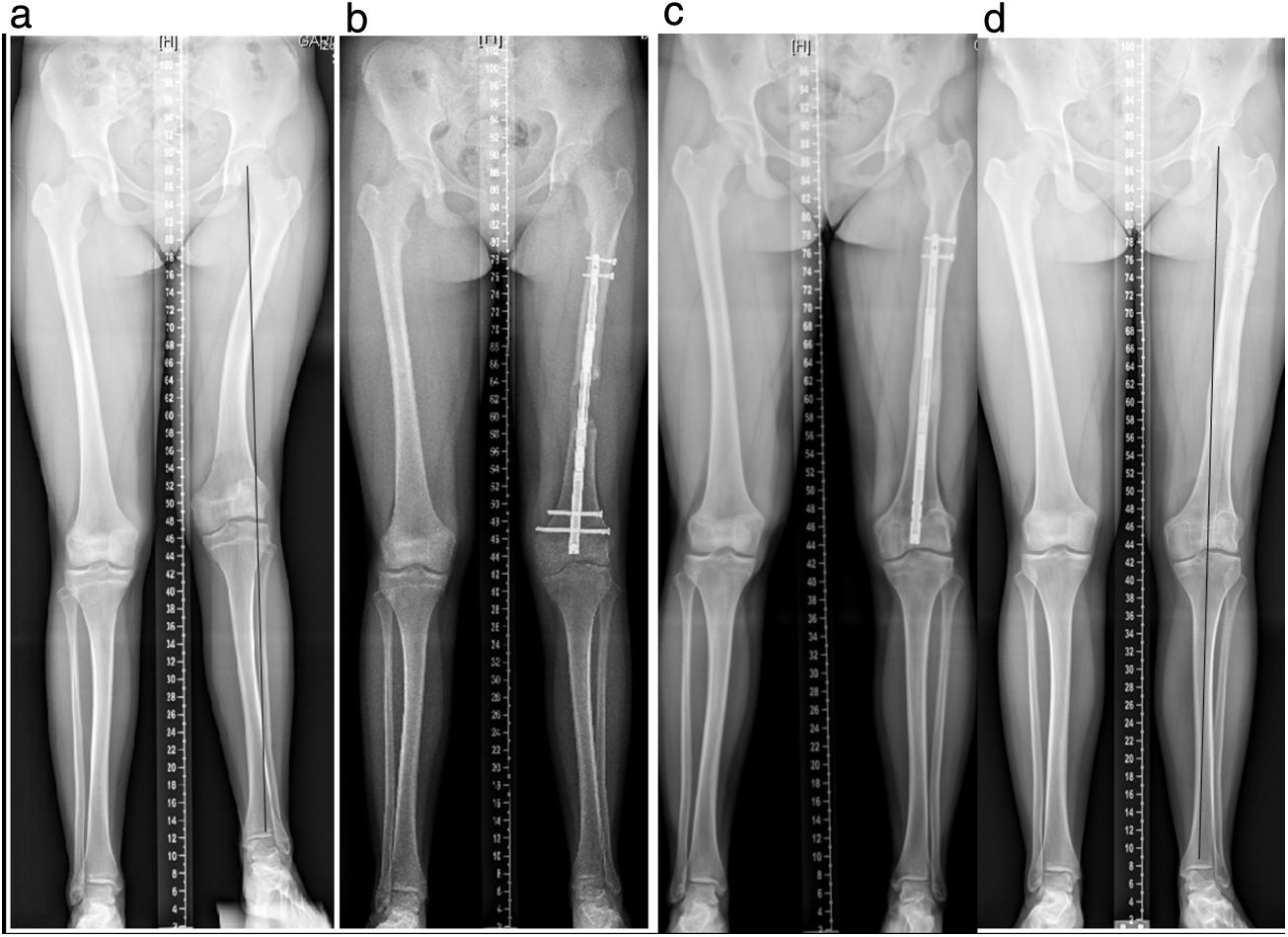
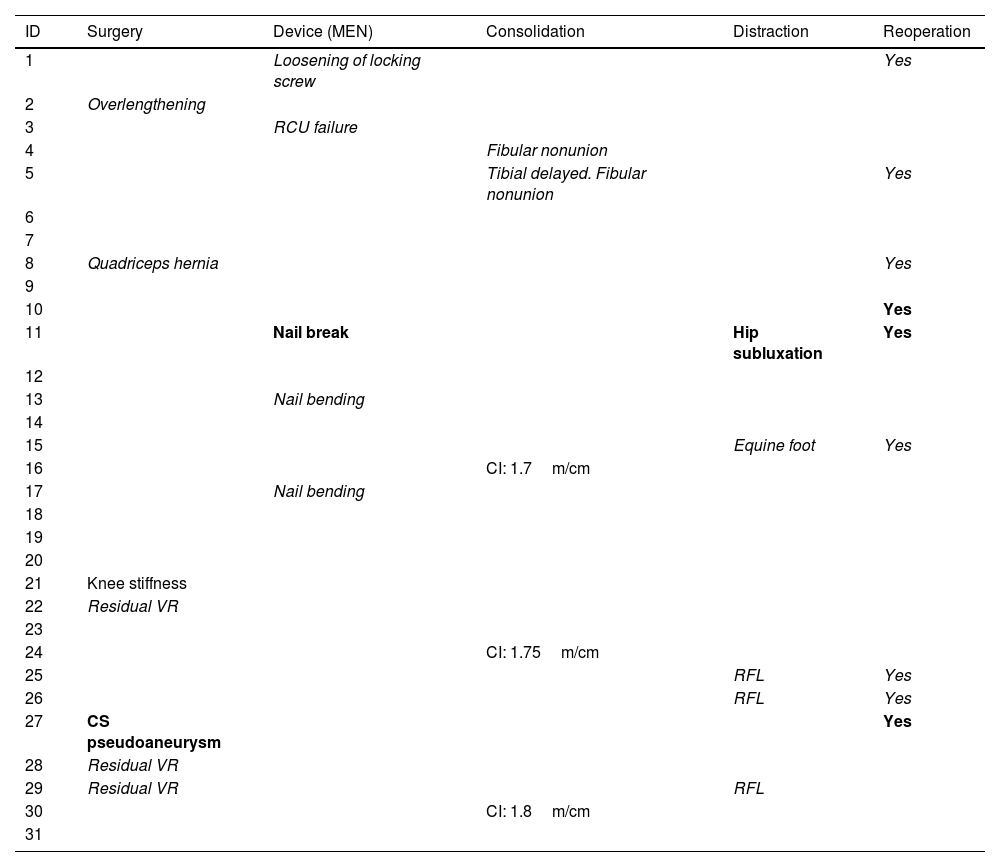
Fourteen of the segments (45%), in 12 patients, had associated deformities, of which 12 were angular, one rotational, and one mixed. None of the angular deformities exceeded 20° from normal. In 8 patients the angular and rotational deformity was corrected acutely (intraoperatively), by the elongation osteotomy itself in 6 cases (Fig. 1) and by another osteotomy in the other 2. In 4 cases of genu valgum, gradual correction took place using guided growth techniques. The corrections were complete in all cases and no residual deformities and/or recurrences were detected at follow-up.
Shortening of 5.5cm, valgus and rotational deformity of the left femur after neonatal septic arthritis of the knee. Twelve-year-old female. (a) Preoperative teleradiographs. (b) Lengthening and angular/rotational correction using Precice2® retrograde nail. (c) Consolidation and compensation of the discrepancy 6 months postoperatively. The knee locking screws required early removal due to loosening of one of them. (d) Radiological control 12 months after nail removal.
Spontaneous consolidation of the elongated segment was achieved in all cases. The CI in this series was 1.1 months/cm (.83–1.8), exceeding 1.7 only in 3 cases of congenital shortening. With the use of MEN, it is important to bear in mind that the CI should only be approximate since, unlike classic lengthening, in which the end date is the date the external fixator is removed, here we count up until full weight bearing, which does not have an exact date. The MEN was removed on average 7.5 months after consolidation (start of full weight bearing), following radiological criteria (at least 3 cortices of similar thickness to the original cortex).
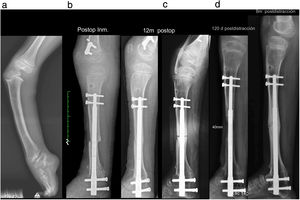
Adverse events were identified in 17 lengthenings (55%) in 16 patients (57%), but only 3 were considered severe (major), of which 2 (7.1%) were left with permanent sequelae (Table 3). The remaining 12 patients (14 segments) had no significant complications.
Complications in the series.
| ID | Surgery | Device (MEN) | Consolidation | Distraction | Reoperation |
|---|---|---|---|---|---|
| 1 | Loosening of locking screw | Yes | |||
| 2 | Overlengthening | ||||
| 3 | RCU failure | ||||
| 4 | Fibular nonunion | ||||
| 5 | Tibial delayed. Fibular nonunion | Yes | |||
| 6 | |||||
| 7 | |||||
| 8 | Quadriceps hernia | Yes | |||
| 9 | |||||
| 10 | Yes | ||||
| 11 | Nail break | Hip subluxation | Yes | ||
| 12 | |||||
| 13 | Nail bending | ||||
| 14 | |||||
| 15 | Equine foot | Yes | |||
| 16 | CI: 1.7m/cm | ||||
| 17 | Nail bending | ||||
| 18 | |||||
| 19 | |||||
| 20 | |||||
| 21 | Knee stiffness | ||||
| 22 | Residual VR | ||||
| 23 | |||||
| 24 | CI: 1.75m/cm | ||||
| 25 | RFL | Yes | |||
| 26 | RFL | Yes | |||
| 27 | CS pseudoaneurysm | Yes | |||
| 28 | Residual VR | ||||
| 29 | Residual VR | RFL | |||
| 30 | CI: 1.8m/cm | ||||
| 31 |
This table shows the complications in the series, the stage or cause of the problem and the patients who required reoperation (in roman: no complications; in italics: minor complications; in bold: major complications).
CI: consolidation index; CS: compartment syndrome; FL: fascia lata; MEN: magnetic endomedullary nail; RCU: remote control unit; RFL: retraction of fascia lata; VR: varus.
There were 7 surgical complications, 2 major and 5 minor (without clinical consequences). The first were “tip effect” results in femoral fracture at the proximal end of the MEN and one compartment syndrome in the operated leg. The fracture occurred at the end of the nail in a femur with a hip prosthesis and progressed well after internal fixation, although with a loss of elongation of 1cm. The compartment syndrome could not be reversed by extending the initial fasciotomy and a popliteal pseudoaneurysm was subsequently detected, which required an emergency by-pass with satisfactory outcome. Due to these complications, the nail was kept “dormant”, and elongation was completed without incident 3 years later. Currently, this patient has residual paralysis of the antero-external compartment of the leg; a potential candidate for future palliative surgery. The 5 minor events were of no clinical consequence; there were 3 cases of mild varus deformity of the proximal femur during nail insertion resulting in a slight loss of femoral length requiring over-elongation.
Five cases had device-related problems. One anterograde femoral nail broke through the proximal locking holes, probably due to premature weight bearing. In 2 cases bending of the implant was observed after the distraction was completed, with no consequences. The generator (RCU) stopped working in one case, which was resolved without repercussions by changing the generator. Loosening of a locking screw was also observed, which needed to be replaced.
There were 3 consolidation problems in the distraction zone: one case due to irregular tibial consolidation (anterior insufficiency) which required reinforcement with autologous graft, and in 2 tibial elongations, which developed fibular non-union.
There were 5 complications associated with distraction in 5 patients. One was a severe case of hip subluxation, which required reduction and pelvic osteotomy, resulting in moderate limitation of hip motion and mild gluteal insufficiency. The other 4 complications were minor, including a case of clubfoot in a tibial elongation, which progressed satisfactorily after lengthening the Achilles tendon, and 3 retractions of the fascia lata, which were resolved with surgical section (2 cases) or physiotherapy (1 case), with no sequelae.
No problems with infection or cases of corrosion of the material were detected.
Of the 16 patients with complications, 9 (32%) required 13 reoperations but only 2 (7.1%) had the permanent sequelae mentioned above. The remaining 26 patients (92.8%) recovered from the procedure without any significant consequences.
Subjectively, the patients stated in the survey that they tolerated the treatment well, and all the cases were satisfied or very satisfied with the result and would undergo the surgery again, except for 2 cases who were not very or not at all satisfied, one of which, in view of their progress, would not undergo the surgery again.
DiscussionMagnetic expandable implant technology has been a decisive step forward in the evolution of bone distraction in general and in the treatment of limb length discrepancies in particular.12,13 This is why we have used it since 2014.
The advantages of bone distraction with MEN over more conventional techniques12 are, on the one hand, external fixation is removed and, on the other, the implant tutorises the elongated/corrected segment. In our series, these advantages were confirmed without exception, as in no case was external fixation required to achieve effective distraction. This was of considerable benefit to our patients in that it simplified the surgical technique, facilitating early joint recovery and acceptable comfort, as well as avoiding infections during treatment. No deformities or fractures of the elongated segment, typical of classic lengthening with external fixators alone, were observed.14 Also, the fact that the lengthening was not extreme (maximum 8cm) was probably an additional advantage.15 In support of these findings, our patients also declared almost unanimous satisfaction with the result obtained, like that of recent comparative studies.13
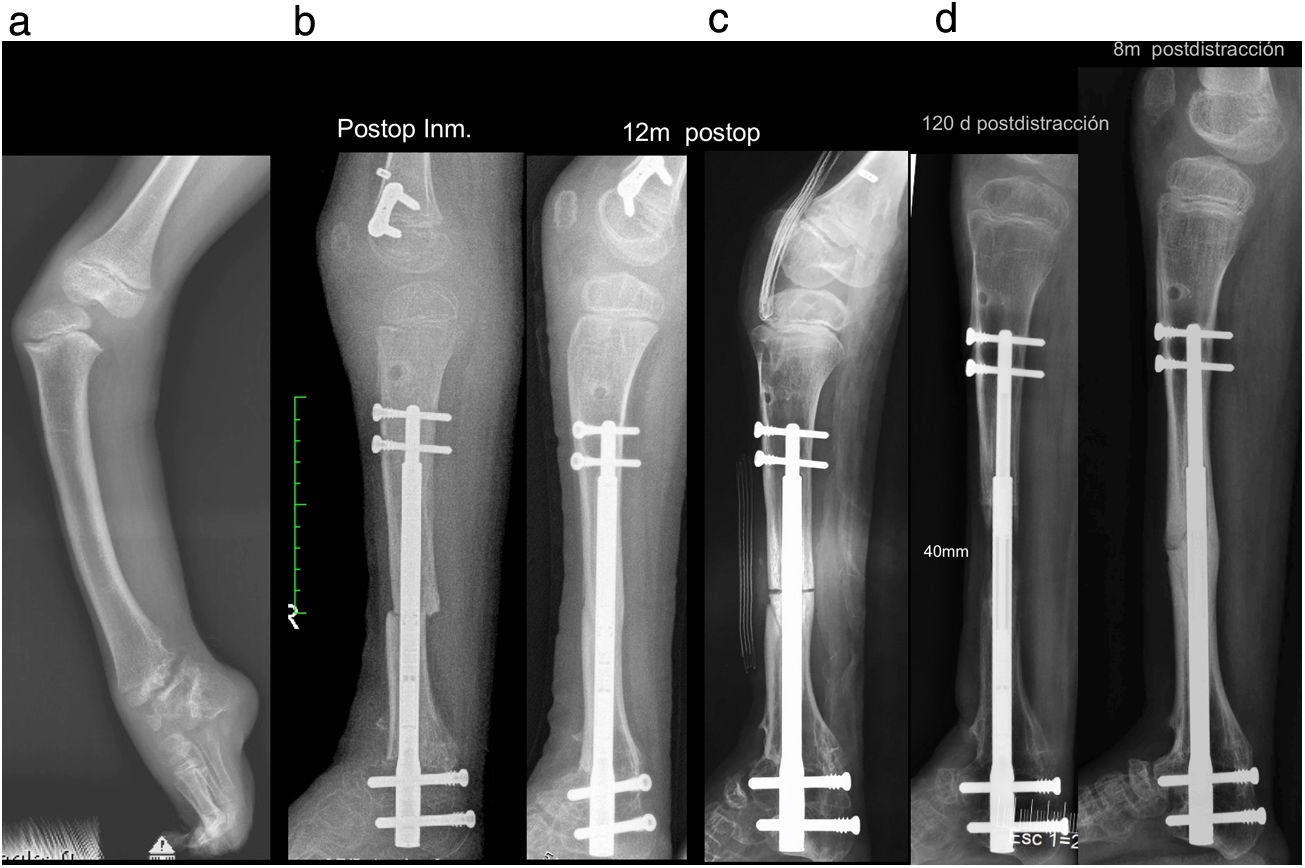
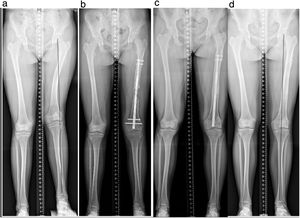
Another important advantage of the MEN is that it can remain implanted for a long time and can be activated at will, which allows lengthening to be postponed (“dormant nails”) or fractionated lengthening.12,13 In our series, 2 patients had dormant nails which were activated without problem, long after implantation (Fig. 2).
Eight-year-old patient with fibula agenesis, knee dislocation and missing ankle. (a) Preoperative. (b) Immediate postoperative period after correction of deformities, ankle fixation and knee stabilisation. Given the considerable risk of reluxation, it was decided to keep the nail “dormant” (without distraction) and allow the osteotomy to consolidate. (c) Consolidated osteotomy 12 months postoperatively. (d) New osteotomy at that time to begin elongation and removal of the femoral 8-plate. (e) 120 days postoperatively, having achieved the objective of 4cm lengthening. (f) 8 months postoperatively with the segment consolidated.
The reliability of the implants was high in this series as they functioned without problem in all but one case, in which the MEN failed and was easily resolved by replacing the unit. The internal mechanism of the MEN did not fail in any of our cases. The precision of Precice® MEN, which has also been the subject of controversy in some publications,16 was satisfactory in our series, as reported by other authors.17,18
The reconstruction of the elongated segment was very satisfactory, with a mean CI of 1.1months/cm, comparable to that of similar series and to that accepted for classic lengthening.11 This contradicts Ilizarov's long-standing theory on the importance of keeping the endomedullary structures intact to achieve good consolidation,19 which has already been observed in other published series of lengthening over a nail (ASC).20,21
Despite these advantages, MEN are not free of complications as they remain gradual bone distraction systems that produce unnatural bone growth.22 In our series, more than half of the lengthening procedures (55%) had complications, 9 required reoperation, although they only left permanent sequelae in 2 patients (7.1%). This rate of adverse events is clearly lower than that published for conventional lengthening and ASC,3 but is still high.23
Although the operating technique has been simplified compared to classic lengthening,12 the surgical complications of these treatments can be serious. In our series, one vascular event stood out, probably due to arterial damage during nail locking, which produced the most important sequelae in this series. The accumulation of stresses generated by placing 2 intramedullary implants with hardly any separation between them caused a femoral fracture in another case. This event could have been avoided by using a shorter MEN or lengthening the other limb segment. The proximal femoral varus caused by insertion of the MEN into 3 trochanteric femoral nails resulted in an immediate loss of a few millimetres which then required overextension and slight medialisation of the mechanical axis, which will require further follow-up to determine its impact. In proximal tibial lengthening, however, we did not observe antecurvatum of the proximal fragment, a well-known tendency in the nailing of proximal third tibial fractures.24 One idea to ameliorate this effect is to place medial Poller screws in the proximal femoral fragment or posterior screws in the proximal tibial fragment. Tibial screws are widely used, but in the proximal femur their placement is technically more compromised and could weaken the calcar. Therefore, to avoid varus in the proximal femur, our recommendation would be to perform the osteotomy in more diaphyseal (more tubular) bone.
Although cases of MEN breakage and mechanical failure have been published,25,26 in our patients there was only one implant breakage, probably because the indications for starting weight bearing were not followed. In 2 other cases, we observed slight bending of the nail, although as this was detected after achieving the expected elongation, it had no consequences for the patient. The emergence of magnetic nails of greater strength, which allow early support, could be a good option to avoid this complication in cases where greater tension is expected, either due to the aetiology or the magnitude of the elongation.27 There is controversy about how to assess the strength of the elongated segment consolidation, in order to allow weight bearing, and objective measurement is not easy.28 Preliminary studies on MEN elongations argue that radiographic pixel density is reliable.29 We were guided by the radiological progress of bone regeneration and allowed gradual weight bearing to begin when at least 3 cortices of the same thickness as the original cortex were visible.
Complications due to distraction with MEN in our cases mainly focussed on the musculature and joints adjacent to the intervened bone, causing a serious case of hip subluxation and 4 retractions of the Achilles tendon or fascia lata. The joints, especially if unstable preoperatively, are very vulnerable to distraction and subluxations or dislocations can occur which, if not detected early, are very difficult to resolve,3,22 as occurred in one of our cases.
The use of MEN is limited in patients with open physes, as previous observations report frequent physeal damage in femoral fracture nailing in immature patients.30 Our 2 patients under 10 years of age had closed physes in the approach route, and therefore there was no risk of altering the growth of this area. Another limitation of MEN is in cases of severe deformity associated with shortening.31 Therefore, in our series, none of the deformities exceeded 20°. The third potential limitation of MEN is the cost of the implant. However, there are comparative studies with classic lengthening in which, adding up all the costs of the procedure, the results are favourable to those obtained with MEN.32
The main limitations of this study are its retrospective nature and the size of the sample, which means that our conclusions cannot be categorical. However, we believe that this preliminary experience may provide useful lessons for future users and, above all, may alert us to the most frequent difficulties in bone lengthening with MEN.
ConclusionsIn patients under 18 years of age, bone elongation with MEN of up to 8cm proved effective, reliable, precise, and safe in achieving its objective in over 90% of cases.
It has also proven to be an advantageous technique over traditional systems, as it simplifies the surgical technique, eliminates the problems associated with external fixation, and tutorises for the operated segment until it is consolidated.
Despite these advantages, these treatments still have a high complication rate, mainly associated with the distraction generated in the process.
Level of evidenceLevel of evidence IV.
FundingNo specific support from public sector agencies, commercial sector or non-profit organisations has been received for this research study.
Conflict of interestsThe authors have no conflict of interests to declare.
Protection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
We would like to thank Óscar Sánchez, Iván García and Mónica Alda for their technical support in the interventions carried out.