To evaluate the influence of epidemiological factors on the outcomes of surgery for degenerative lumbar disease in terms of quality of life, disability and chronic pain.
Material and methodA total of 263 patients who received surgery for degenerative lumbar disease (2005–2008) were included in the study. The epidemiological data collected were age, gender, employment status, and co-morbidity. The SF-36, Oswestry Disability Index (ODI), Core Outcomes Measures Index (COMI), and VAS score for lumbar and sciatic pain were measure before and 2 years after surgery. The correlation between epidemiological data and questionnaire results, as well as any independent prognostic factors, were assessed in the data analysis.
ResultsThe mean age of the patients was 54.0 years (22–86), and 131 were female (49.8%). There were 42 (16%) lost to follow-up. Statistically significant correlations (P<.05) were observed between age, gender, co-morbidity, permanent sick leave, and pre-operative pain with changes in the ODI, COMI, physical and SF-36 mental scales, and lumbar and sciatic VAS. Linear regression analysis showed permanent sick leave and age as predictive factors of disability (β=14.146; 95% CI: 9.09–29.58; P<.01 and β=0.334; 95% CI: 0.40–0.98, P<.05, respectively), and change in quality of life (β=−8.568; 95% CI: −14.88 to −2.26; P<.01 and β=−0.228, 95% CI: −0.40 to −0.06, P<.05, respectively).
ConclusionBased on our findings, age and permanent sick leave have to be considered as negative epidemiologic predictive factors of the outcome of degenerative lumbar disease surgery.
Evaluar si los factores epidemiológicos afectan a los resultados de la cirugía por enfermedad lumbar degenerativa en términos de calidad de vida, discapacidad y dolor crónico.
Material y métodoDoscientos sesenta y tres pacientes intervenidos por afección lumbar degenerativa fueron incluidos en el estudio (2005–2008). Variables epidemiológicas: edad, género, situación laboral y comorbilidad. Se completaron en el preoperatorio y 2 años tras la cirugía el Medical Outcomes Study Short Form-36 version 2, Oswestry Disability Index (ODI), Core Outcomes Measures Index (COMI) y EVA para dolor lumbar y ciático. En el análisis de los datos, se evaluó la correlación entre variables epidemiológicas y el cambio en los resultados de los cuestionarios, así como, la existencia de factores pronósticos independientes.
ResultadosEdad media 54,00 años (22–86); 131 mujeres (49,8%); 42 pérdidas de seguimiento (16%). Se observaron correlaciones significativas (p<0,05) entre la edad, el género, la comorbilidad, la incapacidad laboral permanente y el dolor preoperatorio con el cambio del ODI, el COMI, los componentes de salud física y mental y las EVA de lumbar y ciático. El análisis de regresión lineal muestra a las ILP y la edad como variables predictoras del cambio de la discapacidad (β=14,146; IC del 95%, 9,09–29,58; p<0,01, y β=0,334; IC del 95%, 0,40–0,98, p<0,05, respectivamente) y de la calidad de vida (β=−8,568; IC del 95%, −14,88, −2,26; p<0,01 y β=−0,228, IC del 95%, −0,40, −0,06, p<0,05, respectivamente).
ConclusiónSegún nuestros resultados, hemos de considerar al aumento de la edad y la incapacidad laboral permanente como factores epidemiológicos predictores negativos de los resultados tras cirugía por patología lumbar degenerativa.
Chronic lumbar (or low back) pain is one of the major clinical entities affecting the musculoskeletal system, with a high incidence (85%) and prevalence (84%) in industrialized countries.1–3 The diagnostic process and treatment of chronic lumbar pain (CLP) and the entities included within degenerative lumbar pathology (DLP)4 (Table 1) often require interventions that generate high healthcare expenditures.5 Nevertheless, the implementation of these interventions has increased notably in recent decades. For example, the annual number of lumbar fusions due to DLP in the US has increased from 174,223 operations in 1998 to 413,171 in 2008, becoming the first cause of spinal fusion (or arthrodesis).6
Diagnoses included within degenerative lumbar pathology.4
| Untreatable lumbar pain in the absence of stenosis or spondylolisthesis |
| Disc hernia and radiculopathy |
| Stenosis and spondylolisthesis |
| Stenosis without spondylolisthesis |
CLP and DLP are considered multifactorial clinical entities. Therefore, the results of interventions aimed at addressing them are influenced by several physical, psychological and social factors, many of which are epidemiological factors, such as age, employment status, educational level and smoking, among others.7–9 Moreover, there is still controversy regarding some of them, as in the case of age.10–14The objective of our study was to assess whether epidemiological factors affect postoperative results of DLP interventions in terms of quality of life, disability and chronic pain in our population, aiming to provide new information in order to help improve the selection process of patients and the surgical indications for DLP.
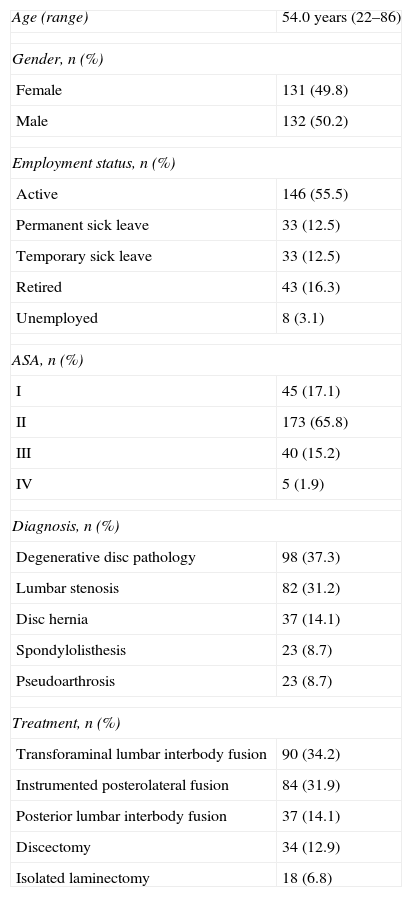
Material and methodsWe provide a retrospective case series of 263 patients who underwent DLP interventions between 2005 and 2008 and who completed preoperative questionnaires (Table 2). A total of 42 cases were lost during follow-up (16%) and did not complete questionnaires at 2 years; 35 patients were not located and 7 died.
Epidemiological data (263 patients).
| Age (range) | 54.0 years (22–86) |
| Gender, n (%) | |
| Female | 131 (49.8) |
| Male | 132 (50.2) |
| Employment status, n (%) | |
| Active | 146 (55.5) |
| Permanent sick leave | 33 (12.5) |
| Temporary sick leave | 33 (12.5) |
| Retired | 43 (16.3) |
| Unemployed | 8 (3.1) |
| ASA, n (%) | |
| I | 45 (17.1) |
| II | 173 (65.8) |
| III | 40 (15.2) |
| IV | 5 (1.9) |
| Diagnosis, n (%) | |
| Degenerative disc pathology | 98 (37.3) |
| Lumbar stenosis | 82 (31.2) |
| Disc hernia | 37 (14.1) |
| Spondylolisthesis | 23 (8.7) |
| Pseudoarthrosis | 23 (8.7) |
| Treatment, n (%) | |
| Transforaminal lumbar interbody fusion | 90 (34.2) |
| Instrumented posterolateral fusion | 84 (31.9) |
| Posterior lumbar interbody fusion | 37 (14.1) |
| Discectomy | 34 (12.9) |
| Isolated laminectomy | 18 (6.8) |
We included in the study those patients who met the following inclusion criteria: being of legal age, having been diagnosed with any of the clinical entities considered as DLP and having undergone surgery for this reason during the period mentioned above. We excluded from the study those patients with a language barrier that prevented them from understanding the questionnaires correctly.
The epidemiological data collected during the study were age, gender, employment status prior to the intervention and the level of comorbidity according to the scale of the American Society of Anesthesiologists (ASA).15,16 We also recorded the clinical diagnosis and the surgical procedure performed.
Quality of life was assessed through the Medical Outcomes Study Short Form-36 version 2 (SF-36),17,18 disability through the Oswestry Disability Index (ODI),19,20 the Core Outcomes Measures Index (COMI)21,22 was used to assess patients globally and visual analogue scales (VAS) were used to evaluate lumbar and sciatic pain23,24 preoperatively and at 2 years after the operation.
All these questionnaires were completed by patients during the preoperative visit, when we also recorded epidemiological factors, and at 2 years after the surgical intervention.
The statistical analysis was performed using the software package SPSS 15.0 (SPSS Inc., Chicago). Quantitative variables (pre–post analysis) were analyzed using the Student t test for dependent data. In order to compare the mean values of the difference between the preoperative and postoperative results of the questionnaires for categorical variables we used the Student t test for independent data in the case of dichotomous variables (gender) and the ANOVA test for categorical variables (ASA and work activity, with the values of the different categories of these variables being dichotomous). The intergroup analysis of those variables where significant differences were found in the ANOVA test was performed using the Honestly-Significant-Difference Tukey test. The study of the correlation between quantitative variables and the variation of the results of the questionnaires was conducted using the Pearson correlation coefficient. Finally, we applied multiple linear regression analysis to identify the existence of possible predictors of change in the results of the questionnaires. To do this, we studied as possible independent predictors the epidemiological dichotomous qualitative and quantitative variables, with significant results in studies for comparison of means and correlation, respectively, and as dependent variables the values of change of the different questionnaires.
ResultsThe mean age of the sample was 54 years (range: 22–86 years). Of the 263 patients, 38 (14.8%) were aged 40 years or younger and 74 (29%) were 65 years or older; 131 patients (49.8%) were female, 146 (55.5%) were active prior to surgery, 33 (12.5%) were on temporary sick leave (TSL), another 33 (12.5%) were on permanent sick leave (PSL) and, finally, 43 patients (16.3%) were retired. The main reasons for surgery were degenerative pathology of an intervertebral disc in 98 cases (37.3%) and lumbar spinal canal stenosis in 82 (31.2%). The most common procedures were transforaminal lumbar interbody fusion (TLIF), performed in 90 cases (34.2%), and instrumented posterolateral fusion (IPF) in 84 (31.9%). In 173 cases (65.8%) there was some kind of spinal canal decompression. A total of 173 (65.8%) patients presented grade II comorbidity according to the ASA scale (Table 2).
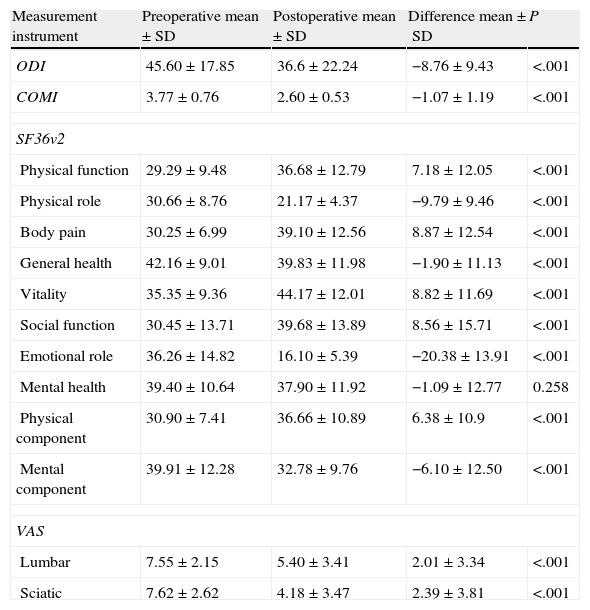
A statistically significant improvement at 2 years in the mean value of the results in all questionnaires, except for the mental health dimension (MH) of the SF-36 (Table 3), was observed.
Comparison of preoperative and 2-year means of the various measurement instruments through the Student t test for dependent variables.
| Measurement instrument | Preoperative mean±SD | Postoperative mean±SD | Difference mean±SD | P |
| ODI | 45.60±17.85 | 36.6±22.24 | −8.76±9.43 | <.001 |
| COMI | 3.77±0.76 | 2.60±0.53 | −1.07±1.19 | <.001 |
| SF36v2 | ||||
| Physical function | 29.29±9.48 | 36.68±12.79 | 7.18±12.05 | <.001 |
| Physical role | 30.66±8.76 | 21.17±4.37 | −9.79±9.46 | <.001 |
| Body pain | 30.25±6.99 | 39.10±12.56 | 8.87±12.54 | <.001 |
| General health | 42.16±9.01 | 39.83±11.98 | −1.90±11.13 | <.001 |
| Vitality | 35.35±9.36 | 44.17±12.01 | 8.82±11.69 | <.001 |
| Social function | 30.45±13.71 | 39.68±13.89 | 8.56±15.71 | <.001 |
| Emotional role | 36.26±14.82 | 16.10±5.39 | −20.38±13.91 | <.001 |
| Mental health | 39.40±10.64 | 37.90±11.92 | −1.09±12.77 | 0.258 |
| Physical component | 30.90±7.41 | 36.66±10.89 | 6.38±10.9 | <.001 |
| Mental component | 39.91±12.28 | 32.78±9.76 | −6.10±12.50 | <.001 |
| VAS | ||||
| Lumbar | 7.55±2.15 | 5.40±3.41 | 2.01±3.34 | <.001 |
| Sciatic | 7.62±2.62 | 4.18±3.47 | 2.39±3.81 | <.001 |
COMI: Core Outcomes Measures Index; ODI: Oswestry Disability Index; SD: standard deviation; SF36v2: Medical Outcomes Study Short Form-36 version 2; VAS: visual analogue scale.
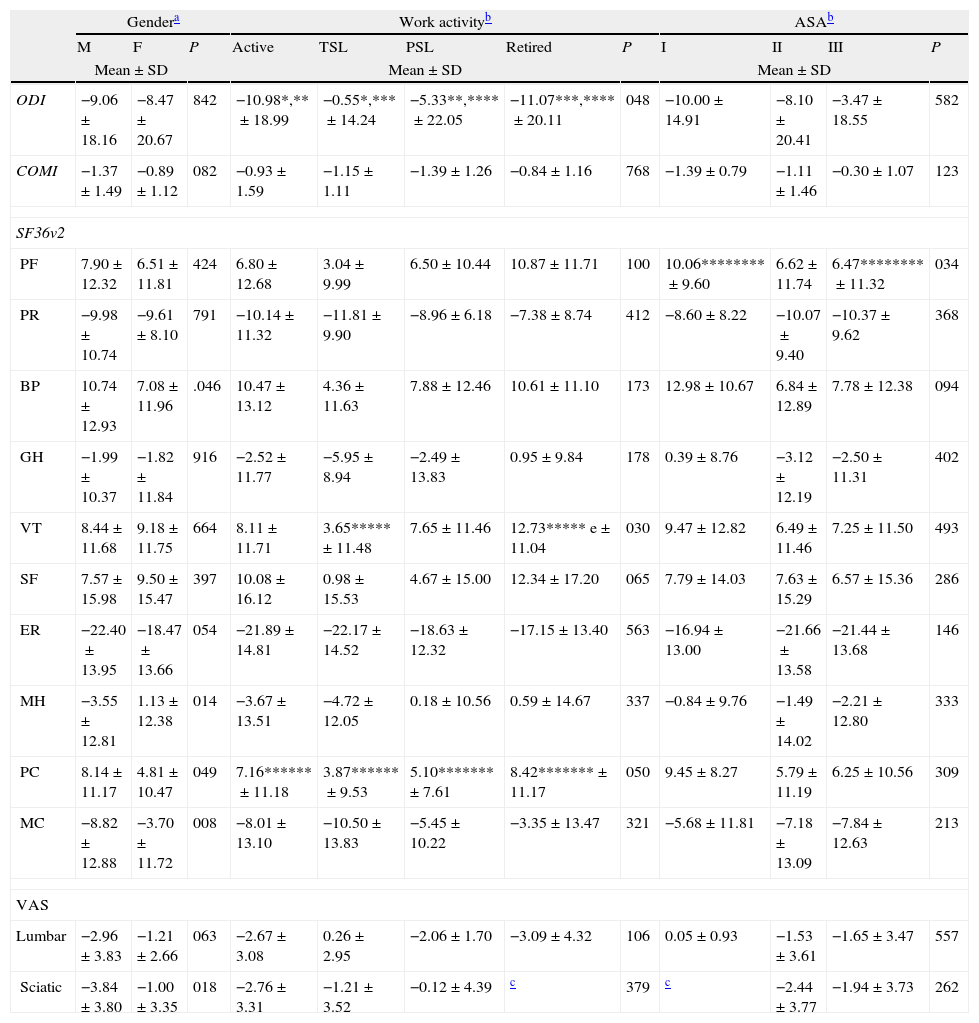
Comparing the mean results by gender illustrated how males presented significantly more improvement than females in the physical component (PC) (P=.049) and mental component (MC) (P=.008), as well as the dimensions of body pain (BP) (P=.046) and mental health (MH) (P=.014), and sciatic pain (P=.018). In the case of work status, we observed that patients on permanent and temporary sick leave presented less statistically significant improvement in the results of the ODI than active and retired patients (P=.048). A similar result was observed in the PC, where patients on TSL presented significantly less improvement than active ones (P=.049), whilst in patients on PSL the smallest improvement was significantly less than in retirees (P=.042). Meanwhile, in the vitality dimension of the SF-36, we only observed minor significant improvement in patients on TSL compared to retirees (P=.05).
Finally, regarding the ASA scale, we only identified statistically significant differences in the physical function dimension of the SF-36 between patients with ASA I and III (P=.026) (Table 4). It should be noted that both the group of unemployed patients and those who presented ASA IV comorbidity were excluded from the above calculations, since only 1 patient in both groups could be assessed at 2 years after surgery.
Comparison of the mean differences between the preoperative results and results at 2 years between the various groups of the qualitative variables studied. Post hoc analysis of the intergroup differences.
| Gendera | Work activityb | ASAb | ||||||||||
| M | F | P | Active | TSL | PSL | Retired | P | I | II | III | P | |
| Mean±SD | Mean±SD | Mean±SD | ||||||||||
| ODI | −9.06±18.16 | −8.47±20.67 | 842 | −10.98*,**±18.99 | −0.55*,***±14.24 | −5.33**,****±22.05 | −11.07***,****±20.11 | 048 | −10.00±14.91 | −8.10±20.41 | −3.47±18.55 | 582 |
| COMI | −1.37±1.49 | −0.89±1.12 | 082 | −0.93±1.59 | −1.15±1.11 | −1.39±1.26 | −0.84±1.16 | 768 | −1.39±0.79 | −1.11±1.46 | −0.30±1.07 | 123 |
| SF36v2 | ||||||||||||
| PF | 7.90±12.32 | 6.51±11.81 | 424 | 6.80±12.68 | 3.04±9.99 | 6.50±10.44 | 10.87±11.71 | 100 | 10.06********±9.60 | 6.62±11.74 | 6.47********±11.32 | 034 |
| PR | −9.98±10.74 | −9.61±8.10 | 791 | −10.14±11.32 | −11.81±9.90 | −8.96±6.18 | −7.38±8.74 | 412 | −8.60±8.22 | −10.07±9.40 | −10.37±9.62 | 368 |
| BP | 10.74±12.93 | 7.08±11.96 | .046 | 10.47±13.12 | 4.36±11.63 | 7.88±12.46 | 10.61±11.10 | 173 | 12.98±10.67 | 6.84±12.89 | 7.78±12.38 | 094 |
| GH | −1.99±10.37 | −1.82±11.84 | 916 | −2.52±11.77 | −5.95±8.94 | −2.49±13.83 | 0.95±9.84 | 178 | 0.39±8.76 | −3.12±12.19 | −2.50±11.31 | 402 |
| VT | 8.44±11.68 | 9.18±11.75 | 664 | 8.11±11.71 | 3.65*****±11.48 | 7.65±11.46 | 12.73***** e±11.04 | 030 | 9.47±12.82 | 6.49±11.46 | 7.25±11.50 | 493 |
| SF | 7.57±15.98 | 9.50±15.47 | 397 | 10.08±16.12 | 0.98±15.53 | 4.67±15.00 | 12.34±17.20 | 065 | 7.79±14.03 | 7.63±15.29 | 6.57±15.36 | 286 |
| ER | −22.40±13.95 | −18.47±13.66 | 054 | −21.89±14.81 | −22.17±14.52 | −18.63±12.32 | −17.15±13.40 | 563 | −16.94±13.00 | −21.66±13.58 | −21.44±13.68 | 146 |
| MH | −3.55±12.81 | 1.13±12.38 | 014 | −3.67±13.51 | −4.72±12.05 | 0.18±10.56 | 0.59±14.67 | 337 | −0.84±9.76 | −1.49±14.02 | −2.21±12.80 | 333 |
| PC | 8.14±11.17 | 4.81±10.47 | 049 | 7.16******±11.18 | 3.87******±9.53 | 5.10*******±7.61 | 8.42*******±11.17 | 050 | 9.45±8.27 | 5.79±11.19 | 6.25±10.56 | 309 |
| MC | −8.82±12.88 | −3.70±11.72 | 008 | −8.01±13.10 | −10.50±13.83 | −5.45±10.22 | −3.35±13.47 | 321 | −5.68±11.81 | −7.18±13.09 | −7.84±12.63 | 213 |
| VAS | ||||||||||||
| Lumbar | −2.96±3.83 | −1.21±2.66 | 063 | −2.67±3.08 | 0.26±2.95 | −2.06±1.70 | −3.09±4.32 | 106 | 0.05±0.93 | −1.53±3.61 | −1.65±3.47 | 557 |
| Sciatic | −3.84±3.80 | −1.00±3.35 | 018 | −2.76±3.31 | −1.21±3.52 | −0.12±4.39 | c | 379 | c | −2.44±3.77 | −1.94±3.73 | 262 |
ASA: American Society of Anesthesiologists; BP: body pain; COMI: Core Outcomes Measures Index; ER: emotional role; F: female; GH: general health; M: male; MC: mental component; MH: mental health; ODI: Oswestry Disability Index; PC: physical component; PF: physical function; PSL: permanent sick leave; PR: physical role; SD: standard deviation; SF: social function; SF36v2: Medical Outcomes Study Short Form-36 version 2; TSL: temporary sick leave; VAS: visual analogue scale; VT: vitality.
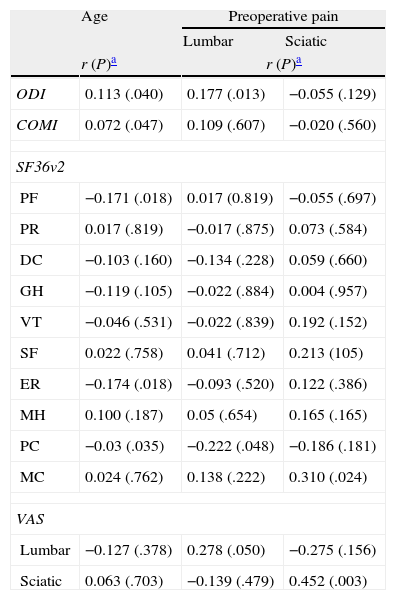
The correlation studies showed how the increasing age of patients was significantly correlated with a worse outcome in the ODI (r=0.113; P=.04) and PC of the SF-36 (r=−0.03; P=.035). Meanwhile, the intensity of preoperative lumbar pain was correlated with less improvement in the MC (r=−0.222; P=.048) and postoperative lumbar pain (r=0.278; P=.05). Moreover, the intensity of preoperative sciatic pain was significantly correlated with improvement in the MC (r=0.310; P=.024) and worse postoperative sciatic pain (r=0.452; P=.003) (Table 5).
Correlation studies between the continuous epidemiological variables and the variation in the results of the questionnaires.
| Age | Preoperative pain | ||
| Lumbar | Sciatic | ||
| r (P)a | r (P)a | ||
| ODI | 0.113 (.040) | 0.177 (.013) | −0.055 (.129) |
| COMI | 0.072 (.047) | 0.109 (.607) | −0.020 (.560) |
| SF36v2 | |||
| PF | −0.171 (.018) | 0.017 (0.819) | −0.055 (.697) |
| PR | 0.017 (.819) | −0.017 (.875) | 0.073 (.584) |
| DC | −0.103 (.160) | −0.134 (.228) | 0.059 (.660) |
| GH | −0.119 (.105) | −0.022 (.884) | 0.004 (.957) |
| VT | −0.046 (.531) | −0.022 (.839) | 0.192 (.152) |
| SF | 0.022 (.758) | 0.041 (.712) | 0.213 (105) |
| ER | −0.174 (.018) | −0.093 (.520) | 0.122 (.386) |
| MH | 0.100 (.187) | 0.05 (.654) | 0.165 (.165) |
| PC | −0.03 (.035) | −0.222 (.048) | −0.186 (.181) |
| MC | 0.024 (.762) | 0.138 (.222) | 0.310 (.024) |
| VAS | |||
| Lumbar | −0.127 (.378) | 0.278 (.050) | −0.275 (.156) |
| Sciatic | 0.063 (.703) | −0.139 (.479) | 0.452 (.003) |
BP: body pain; COMI: Core Outcomes Measures Index; ER: emotional role; GH: general health; MC: mental component; MH: mental health; ODI: Oswestry Disability Index; PC: physical component; PF: physical function; PR: physical role; SF: social function; SF36v2: Medical Outcomes Study Short Form-36 version 2; VAS: visual analogue scale; VT: vitality.
Finally, among the possible predictive variables found in the comparison of mean results of the qualitative variables and the correlation studies conducted with quantitative variables, the multiple linear regression analysis only identified the fact of being on PSL as a predictor of less improvement in the ODI (β=14.146; 95% CI, 9.09–29.58; P<.01) and the PC of the SF-36 (β=−8.568; 95% CI, −14.88 to −2.26; P<.01); just like age in the ODI (β=0.334; 95% CI, 0.40–0.98; P<.05) and PC (β=−0.228; 95% CI, −0.40 to −0.06; P<.05).
DiscussionThe outcomes of DLP surgery are influenced by physical, psychological and social factors, such as gender, age, employment status, educational level, smoking, being a first intervention or reoperation, income, legal disputes, depressive episodes or a neurotic personality and, of course, the degree of joint and intervertebral disc degeneration, with the latter being a significant risk factor for reoperation in surgery for a herniated disc.7–9 In this study, we noted how, in our population, quality of life, disability, general welfare and pain were correlated and, in some cases, were affected by epidemiological factors.
Due to this multifactorial involvement of postoperative outcomes, a division of broad concepts, such as “degenerative disc disease” and “chronic lumbar pain”, into relevant clinical entities, such as “spondylolisthesis”, “lumbar spinal canal stenosis” and “herniated disc” has been recommended, since the diagnosis itself is a factor which significantly affects the outcome.7,25,26
Age is an important and controversial variable since, although most authors agree in identifying it as an independent predictor, according to their studies, some identify it as a negative predictor10–13 and others as a positive predictor.14 In our study, as in much of the literature reviewed, we observed that younger patients presented better postoperative quality of life, disability and pain outcomes.13
Meanwhile, Manniche et al.27 identified female gender as a negative factor for the improvement of disability.
In our experience, the employment status of patients was an important determinant of postoperative outcomes and in our work we describe how the fact of being on permanent sick leave or not significantly affected the improvement in terms of quality of life and disability. The situation was similar to that of other factors which were previously described, such as low work satisfaction, poor economic situation and not receiving financial compensation in the event of sick leave, all of which are considered as independent negative predictors of quality of life, disability and postoperative pain.8,13,29,30
Although in our work we have only identified a weak correlation between preoperative lumbar or sciatic pain and postoperative results, preoperative pain is a variable that has been widely studied. Various works have reported that the intensity of preoperative lumbar pain negatively affects postoperative pain and outcome as assessed by COMI.30–32 Similarly, patients with worse lumbar than sciatic pain have worse outcomes after conservative or surgical treatment.33
Although they have not been explicitly reviewed in this work, smoking14,28,29 and psychiatric status, mainly depressive syndromes, 39,30,34 are 2 important factors that have also been frequently cited as significant negative predictors of disability improvement, quality of life and lumbar and sciatic pain in postoperative patients undergoing surgery for DLP. Other minor negative predictors cited in the literature are a history of repeated headaches, use of analgesics prior to the intervention, poor functional status, low expectations regarding the treatment and a high body mass index.29,30
Some noteworthy limitations of this study are the fact of being a nonrandomized, retrospective case series, whose number of patients and losses could lead to a decrease in sensitivity for detecting the effect of several variables, mainly those with lower frequency. Similarly, the significant extent of the ranges of the different variables must be counted as a separate limitation of this study given the objective of globally studying the population affected by DLP, which could mask the effect of a specific variable within a particular group of the population examined.
In conclusion, according to our results, we believe that increasing age and employment status are negative factors that can affect the postoperative outcome of degenerative lumbar disease, evaluated in terms of quality of life and disability, with these results being independent of gender, preoperative pain and comorbidity. Therefore, our study reinforces the hypothesis that an accurate and meticulous preoperative assessment of patients is essential to assist in the clinical treatment decision, in order to achieve the best results in each case.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lozano-Álvarez C, Pérez-Prieto D, Saló-Bru G, Molina A, Lladó A, Cáceres E, et al. ¿Pueden influir las variables epidemiológicas el resultado a los 2 años de una cirugía por enfermedad lumbar degenerativa en términos de calidad de vida, discapacidad y dolor postoperatorio?. Rev Esp Cir Ortop Traumatol. 2014;58:78–84.