Vertebral compression fractures by osteoporosis (OVF) is usually a diagnostic problem and coincides on the age group of metastatic vertebral compression fractures (MVF). Although radiography is the first diagnostic technique, generally is not accurate for depicting demineralization and soft tissue lesions. Magnetic resonance (MRI) is the diagnostic choice. The most relevant signs are intravertebral fluid collection or fluid signal, other vertebral deformities without oedema and older age. Among the most relevant findings for diagnosis MVF are soft tissue mass and pedicle intensity signal asymmetries. However, reproducibility of these findings in clinical practice is moderate.
La compresión vertebral por fractura osteoporótica vertebral (FOV) es habitualmente un problema diagnóstico y coincide con el grupo de edad de las fracturas vertebrales metastásicas (FVM). Aunque la radiografía es la primera prueba diagnóstica, habitualmente es insensible para detectar desmineralización y lesiones de partes blandas. La resonancia magnética (RM) es la prueba de elección. Los signos de imagen más indicativos de FOV son el signo de la hendidura (señal de líquido intravertebral), otras fracturas sin edema intraóseo y la edad. Entre los más relacionados con FVM se encuentran la tumoración paravertebral y las asimetrías en los pedículos vertebrales. Sin embargo, la reproducibilidad de estos signos de imagen en la práctica clínica es moderada.
Osteoporosis frequently appears with ageing and vertebral fracture is the most common condition that may occur because of it.1,2 The existence of a fracture without a traumatic history is diagnosis in itself of osteoporosis, regardless of the result of the densimetry.3 The diagnosis of osteoporotic vertebral fracture (OVF) indicates a search for its aetiology, the establishment of treatment for osteoporosis and the adoption of preventive measures to reduce the risk of more fractures presenting.3 However, OVFs are usually under-diagnosed for many reasons, the main one being that they are usually asymptomatic, only detected by imaging techniques.4 Even with X-rays, up to 50% are undetected.5 It is estimated that one third of OVFs are never diagnosed.6 Studies have been published that detect vertebral fractures with automatic algorithms. Their results are still unsatisfactory, where, together with radiography, they present a diagnostic accuracy similar to that of an expert radiologist.7 The same occurs in computed tomography (CT) in studies conducted for any reason. Its sensitivity is .68 and specificity is .91. Poorer performances occur in other countries. Its authors indicate that these results cannot be extrapolated to the rest of the population.8
A major impediment is that the usual diagnostic densitometry test for diagnosing osteoporosis has major limitations. In the Spanish population it has been proven that 59% of patients with vertebral fractures, detected by CT for other reasons, had densitometry that did not indicate osteoporosis.9
Another complication is that these fractures usually coexist with the age group where vertebral metastases (MVF) occur, which means that they can be confused with those caused by osteoporosis, and fractures of both types can coexist in the same patient.
Myths in vertebral fracturesAmong the commonly widespread ideas that must be disproved, there are two that stand out. One, that all vertebral deformity is a fracture. In addition to congenital malformations (e.g., butterfly vertebra), there are constitutional, non-traumatic and degenerative irregularities of the vertebral plateaus. The other myth indicates that the fracture must cause deformity. Magnetic resonance imaging (MRI), among other techniques, facilitates the assessment of trabecular fractures prior to the existence of cortical deformity.
Imaging studiesX-ray is the basis of diagnosis when a fracture is suspected and the most commonly used test. A height loss of ≥20% is considered a fracture. It is not suitable in cases of suspected spinal metastases, because it only detects demineralisation when bone loss is ≥50%.10 Although there are no defined criteria for the diagnosis of a recent fracture,4 they are usually classified according to Genant's semi-quantitative classification11 as mild, moderate or severe. All physicians involved in their diagnosis and treatment should avoid ambiguous terms such as “wedging,” “collapse,” “compression,” “height loss,” or “wedge deformity” and call them fractures.12 Among the different types of fractures, there are some types with a higher risk of vertebral collapse13 (Table 1).
There are recent guidelines for the indication of diagnostic tests, such as the American College of Radiology's evidence-based medicine (EBM) with its appropriateness criteria14 (Table 2).
Indications for diagnostic tests as appropriate for vertebral compression fractures according to ACR Appropriateness Criteria. Only the appropriate ones are indicated.
| New symptomatic vertebral compression fracture on X-ray. Non-neoplasia | |
|---|---|
| Technical | Suitability category |
| Non-contrast segmented MRI of the spine | Usually adequate |
| Non-contrast segmented CT of the spine | Usually adequate |
| New symptomatic vertebral compression fracture on X-ray. History of neoplasia | |
|---|---|
| Segmented spinal MRI with and without contrast | Usually adequate |
| Non-contrast segmented CT of the spine | Usually adequate |
| Non-contrast segmented MRI of the spine | Usually adequate |
| Asymptomatic vertebral compression fracture on X-ray. History of neoplasia | |
|---|---|
| Segmented spinal MRI with and without contrast | Usually adequate |
| Non-contrast segmented CT of the spine | Usually adequate |
| Non-contrast segmented MRI of the spine | Usually adequate |
| New low back pain. History of treated or multiple vertebral fractures | |
|---|---|
| Non-contrast segmented CT of the spine | Usually adequate |
| Non-contrast segmented MRI of the spine | Usually adequate |
Computed tomography (CT) shows obvious fractures and involvement of the spinal canal, but does not facilitate visualisation of intra-osseous oedema and soft tissue injuries. It can show adnexal haematoma in acute trauma, but it is much inferior to MRI in the delineation of tissue contrast.15 Its other great limitation is dosage. While the effective dose of an X-ray is 2.5mSv and the dose of densitometry is .01–.05mSv, the dose of a spinal CT segment is 6.0mSv.13 Its advantage is lower cost compared to MRI and its wide availability in non-complex hospitals, where MRI is not available. MRI is the test of choice, both to establish OVF diagnosis and to attempt to rule out neoplastic origin,3 due to its greater contrast resolution, multiplanar capacity and absence of ionising radiation.
Among the MR imaging sequences to differentiate OVF and MVF, there are in-phase and out-of-phase weighted ones. They are based on the fact that normal bone marrow loses signal intensity when out of phase due to its greater fatty component, but the presence of metastases means that it does not lose signal intensity (Fig. 1).
(A) Sagittal CT image of compression fracture at T12. Note the gas in the anterior spine, and also the intradiscal gas. (B) Sagittal in-phase T1-weighted MR image. Note the hypointense area in the anterior spine that corresponds to the intraosseous gas observed on CT. (C) Sagittal out-of-phase T1-weighted MR image. The normal bone marrow loses signal intensity (becomes hypointense), except for the bone infiltrated with pathological bone marrow (arrow) in the medial spine. (D) Sagittal T2-weighted MR image. We may distinguish invasion of the spinal canal with better precision than T1 images. (E) Axial T2-weighted MR image. Note the convex protrusion of the bone fragment into the spinal canal.
There is a variety of signs from imaging that make the diagnosis of OVF more likely than MVF, the most common being16:
- •
Slit formation (“fluid signal”): a homogeneous area of T1 hypointensity and high T2 intensity is defined with a slit sign or “fluid signal” that is associated with OVF rather than MVF (Fig. 2).
- •
Vertebral signal intensity pattern: a complete or partial replacement of vertebral signal intensity is associated with MVF. However, a band-like pattern more likely indicates OVF (Fig. 3). This vertebral oedema is considered acute, persisting for up to 2 months. Chronic vertebral fractures (>3 months) do not present it.
Figure 3.(A) 52-Year-old woman with a history of HER2+++ breast carcinoma without current treatment, presenting with pain in the right upper quadrant. Lateral X-ray showing grade 1 fracture at T12. (B) Sagittal T1-weighted MR image showing band-like hypointensity of the upper vertebral half due to intraosseous oedema. (C) Sagittal T2-weighted MR image with fat saturation showing convex retropulsion of the medial spine in the spinal canal (arrow), in addition to intraosseous oedema. (D) Axial T1-weighted MR image. Note symmetry in the signal intensity of the vertebral pedicles.
(0.15MB). - •
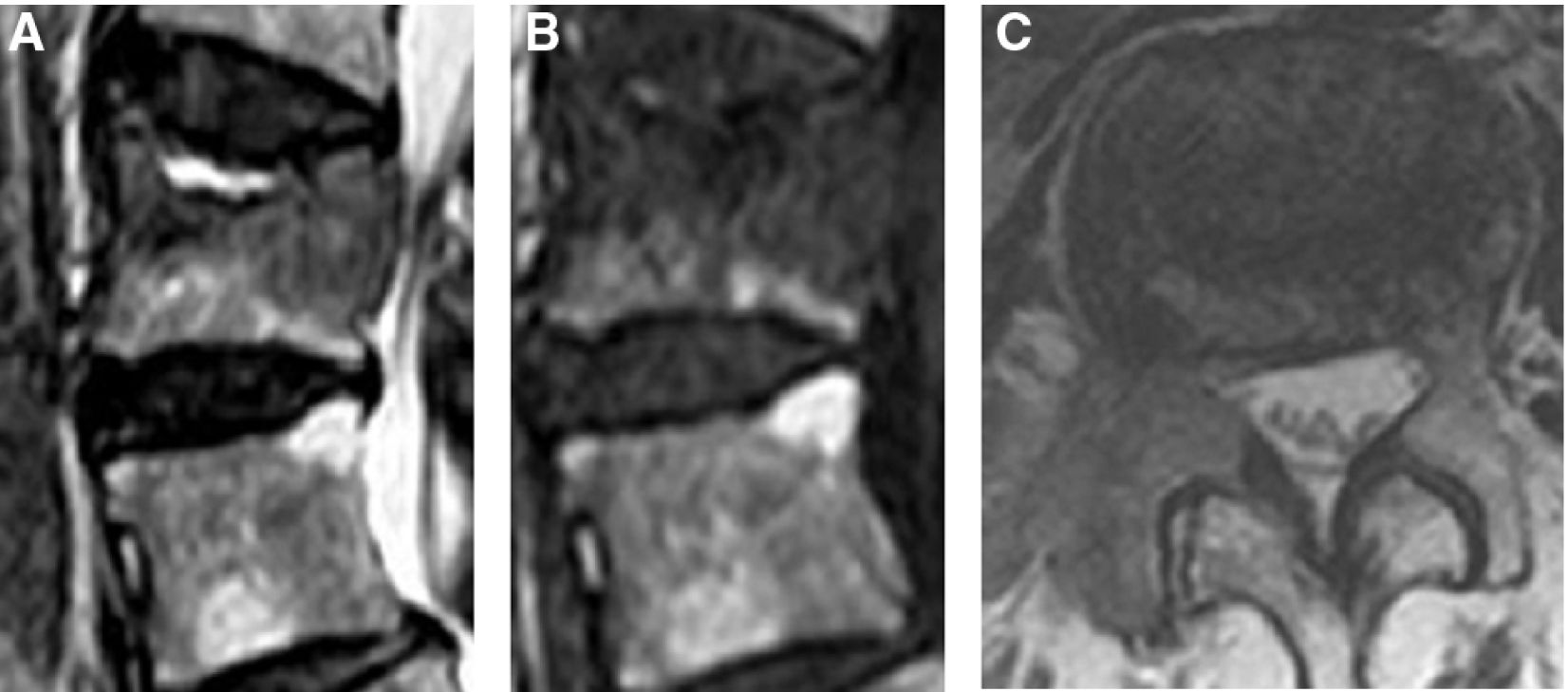
Pedicle involvement: the existence and asymmetry of signal intensity in the posterior half of the pedicle makes the diagnosis of MVF17 more likely (Fig. 4). This description includes areas of focal type signal intensity.16 Furthermore, metastases that affect the vertebral lamina have a higher risk of causing symptomatic spinal cord compression,18 while only 22% of metastases in the vertebral body affect this location.19
- •
Contour of the posterior vertebral edge: it was considered that if the fracture presents a distortion of the convex posterior edge towards the spinal canal, it is more likely to be MVF.17 However, these findings are equally observable in OVF17 (Fig. 3C).
All these signs were analysed in a cohort study of patients with vertebral fractures. A multivariate model was made, which collected them as they were observed in clinical practice and obtained a probability ratio (odds ratio [OR]); If it was >1, the increasing probability of the specific diagnosis increased compared to the other. The most predictive signs were: for MVF, focal paraspinal tumour and focal signal intensity changes (deposits) in vertebral pedicles.16 Likewise, more indicative for OVF were age, other compression deformities without intraosseous oedema and formation of cleft or fluid signal (Table 3). In any event, when these imaging signs converge, malignant pathology is more likely (Fig. 5).
Variables associated with metastatic vertebral fracture.
| OR | |
|---|---|
| Focal paraspinal tumour | 7.87 |
| Focal deposits in vertebral pedicles | 4.8 |
| Age | .94 |
| Other compression deformities without intraosseous oedema | .15 |
| Cleft formation or liquid signal | .11 |
OR: odds ratio. If it is >1, the increasing probability of the specific diagnosis (event) increases.
(A) Sagittal T2-weighted MR image. L2 fracture is observed with fluid sign with signal hyperintensity in the superior endplate, but underlying hypointense lesion. (B) Sagittal T1-weighted MR image. Horizontal signal hypointensity is observed in the superior endplate, confused with the underlying hypointense lesion. (C) Axial T1-weighted MR image. Signal hypointensity is seen with destruction of the right pedicle due to metastasis.
It is of note that articles and web applications, purportedly based on BPM,20 existed for these vertebral fractures and were advertised as predictors of fracture type, based on the before-mentioned MRI signs. However, the reproducibility of these imaging signs in MRI has only recently been established.21 Interobserver agreement between different specialists in clinical practice is moderate and does not depend on their experience or the hospital comlexity.21
Therefore, the serious limitations of BPM,22 must be acknowledged, mainly because reproducibility and reliability are confused with agreement. One limitation is that the diagnostic tests on which the BPM should be based are themselves inconsistent or their reliability has not been demonstrated.23
To conclude, the most indicated test for correct assessment is MRI and for OVF, the most indicative signs are cleft formation or fluid signal, or other compression deformities without intraosseous oedema, and age.
Level of evidenceLevel of evidence iv.
Ethical considerations- 1.
No animal testing.
- 2.
No patients or humans were involved since this is a review article.
- 3.
No clinical trial or part of the same included.
- 4.
All the data shown in the figures and tables included in the manuscript are included in the results and conclusions section.
None.
Conflict of interestsNone.