To determine the incidence of dislocation after primary total hip arthroplasty using a posterior approach with repair of capsule and transosseous external rotators.
Material and methodHistorical cohort study between January 2009 and December 2015 of all the cases of dislocation of primary total hip arthroplasty operated using a posterior approach with repair of capsule and transosseous external rotators. Demographic and clinical data concerning the patient, surgery and dislocation were collected and analyzed. A descriptive analysis and a study of survival and risk function were performed by Kaplan–Meier's method considering the appearance of a hip dislocation as the final event.
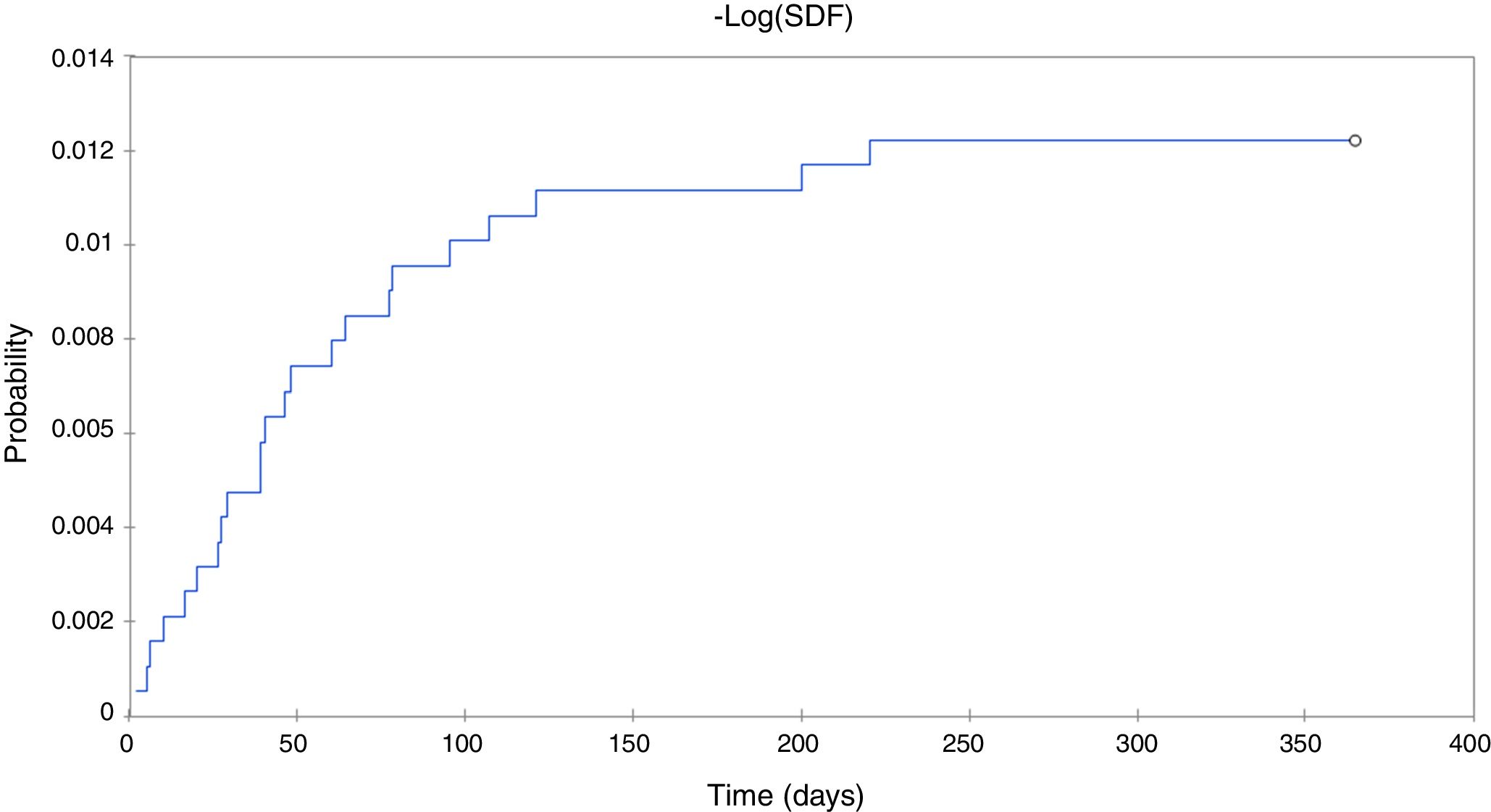
ResultsThe incidence of dislocation in our study was 1.2% (23 patients). In our study, the highest probability of dislocation occurred in the first 120 days. Forty-three point 5 percent of the dislocated patients needed revision surgery.
ConclusionsCapsular repair and transosseous reattachment of the external rotators can help to reduce the incidence of dislocation in patients undergoing primary total hip arthroplasty through a posterior approach.
Determinar la incidencia de luxación después de una artroplastia total de cadera primaria utilizando un abordaje posterior con reparación capsular y reinserción transósea de rotadores externos.
Material y métodoEstudio de una cohorte histórica entre enero del 2009 y diciembre del 2015 de todos los casos de luxación de artroplastia total de cadera primaria intervenidos mediante un abordaje posterior con reparación capsular y reinserción transósea de rotadores externos. Se recogieron y analizaron los datos demográficos y los datos clínicos referentes al paciente, a la cirugía y a la luxación. Se realizaron un análisis descriptivo y un estudio de supervivencia y función de riesgo por el método de Kaplan-Meier considerando como evento final la aparición de una luxación de cadera.
ResultadosLa incidencia de luxación en nuestro estudio fue del 1,2% (23 casos). En nuestro estudio, la mayor probabilidad de luxación ocurrió en los primeros 120 días. El 43,5% de pacientes luxados necesitaron cirugía de revisión.
ConclusionesLa reparación capsular y la reinserción transósea de los rotadores externos pueden contribuir a reducir la incidencia de luxación en los pacientes operados de una artroplastia total de cadera mediante una vía posterior.
Total hip arthroplasty (THA) has been defined as the most successful surgery in the XX century, as it is efficacious in treating pain and restore the level of physical activity in line with the patient's age.1,2 However, despite the many advances in THA, dislocation continues to be an important complication. Dislocation of the hip is the second most common complication of THA, with an incidence rate of 0.3–10% in primary surgeries and up to 28% in revision surgeries.3,4 Furthermore, it is the leading cause of revision in THA during the first 5 years following surgery.5 This complication that the orthopaedic surgeon confronts entails great morbidity, as well as elevated economic costs. Most of the patients who exhibit these issues require hospitalization for one or more closed reductions and, on occasion, need revision surgery.4
Numerous risk factors for dislocation have been identified related not only with the patient, but also with the implant design and surgical technique. The type of approach can be included among the last group.5 Any number of approaches can be used to perform a THA. Each one has its pros and its cons. At present, there is no consensus as to which one is the best.6,7 The posterior approach is the most widely used, as it allows for full exposure of the femur and acetabulum, the abductor muscles are not injured, and it has a shorter learning curve.8 Some series have reported dislocation rates 2–3 times higher following primary THA performed using the posterior approach versus a primary THA using an anterior approach.7 Nevertheless, some authors have indicated that the risk of dislocation with this approach decreases significantly with repair of the capsule and reinsertion of the short external rotator muscles.9 Because there is a lack of comparative clinical trials and the controversy surrounding the integrity of this repair during the postoperative period, some orthopaedic surgeons currently do not routinely perform it.10,11
The objective of this study is to determine the incidence of dislocation following primary THA using the posterior approach with repair of the capsule and transosseous reinsertion of the external rotators. In addition, we compare our incidence of dislocation with the literature and analyze the risk factors, time of dislocation, and treatment received in our patients.
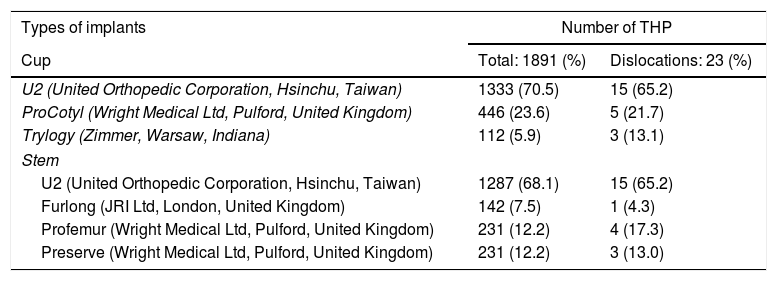
Material and methodStudy designA historical cohort was evaluated that included all the patients who underwent a scheduled primary THA in our institution's hip unit using the posterior approach with repair of the capsule and transosseous reinsertion of the external rotator musculature between January 2009 and December 2015. Patients in whom THA was performed due to dysplasia or fracture, patients with superficial prosthesis, and those who presented neuromuscular diseases or mental illness. There were 1891 hip surgeries in 1437 patients; 651 men (45.3%) and 786 women (54.7%). The mean age of the sample was 69 years (range 36–89 years). The cup was not cemented in any of the cases. In 16.3% (308 hips), the stem was cemented (Table 1). Of these patients, those who display dislocation were identified. For the final analysis, only the cases meeting the following inclusion criteria were evaluated: patients operated on by surgeons specialized in the hip with a diagnosis of early dislocation of THA. Early dislocation was defined as dislocation occurring within the first 12 months.12
Types of implants placed in the study.
| Types of implants | Number of THP | |
|---|---|---|
| Cup | Total: 1891 (%) | Dislocations: 23 (%) |
| U2 (United Orthopedic Corporation, Hsinchu, Taiwan) | 1333 (70.5) | 15 (65.2) |
| ProCotyl (Wright Medical Ltd, Pulford, United Kingdom) | 446 (23.6) | 5 (21.7) |
| Trylogy (Zimmer, Warsaw, Indiana) | 112 (5.9) | 3 (13.1) |
| Stem | ||
| U2 (United Orthopedic Corporation, Hsinchu, Taiwan) | 1287 (68.1) | 15 (65.2) |
| Furlong (JRI Ltd, London, United Kingdom) | 142 (7.5) | 1 (4.3) |
| Profemur (Wright Medical Ltd, Pulford, United Kingdom) | 231 (12.2) | 4 (17.3) |
| Preserve (Wright Medical Ltd, Pulford, United Kingdom) | 231 (12.2) | 3 (13.0) |
THP: total hip prosthesis.
In patients meeting the inclusion criteria and without any exclusion criteria, the following data were collected and analyzed: demographic data (age, sex), clinical data about the patient (body mass index, American Society of Anesthesiologists [ASA]), and data regarding surgery and dislocation (aetiology of the THA, time in days between the surgery and the 1st episode of dislocation, mechanism of dislocation, number of dislocations, type of treatment, and complications).
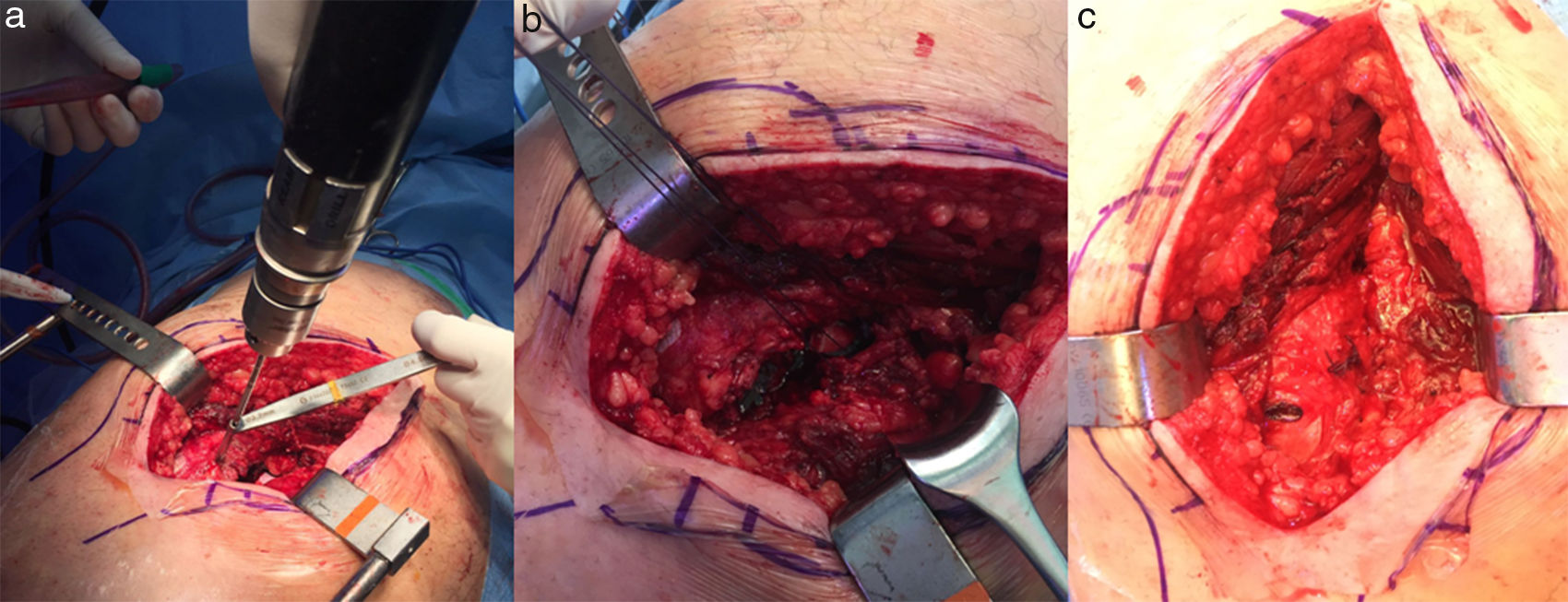
Description of the surgical techniqueThe surgical technique was the same in all cases. The interventions were performed by the same team of surgeons specialized in the hip. All the patients received antibiotic prophylaxis and anticoagulation therapy with low molecular weight heparin. Patients were placed on their side with supports at the level of the pubic symphysis and the sacrum to stabilize the hip. Surgery was performed using a posterior approach. The tensor of the fascia lata was later opened and the fibres of the gluteus maximus were dissected, detaching the external rotators muscles of the hip that included the pyramidalis muscle, superior and inferior gamellus muscles, internal and external obturators, and quadratus femoris muscle. The muscles were detached as close as possible to their insertion in the trochanter. Prior to dislocating the hip, a Steinmann was placed 2–3cm above the upper edge of the acetabulum, measuring and marking the distance between the Steinmann and the lateral surface of the greater trochanter. This step was useful to mark length of the leg and offset of the hip, which were re-measured with the trial implants. A posterior T-capsulotomy and posterior coxofemoral dislocation were then performed. The acetabular and femoral components were prepared following the usual surgical technique and attempting to reproduce femoral and acetabular anteversion, as well as the offset between the diaphyseal axis and the centre of the femoral head. Once the stability of the prosthesis had been verified, the capsule and rotator musculature were repaired by means of 2 transosseous sutures on the posterior edge of the greater trochanter (Fig. 1a–c). The more proximal suture included the pyramidalis tendon and the more distal one included the remaining rotator musculature. Closure was performed by planes, the fascia lata, subcutaneous, and skin.
Repair of the rotator musculature by placing 2 transosseous sutures on the edge of the greater trochanter. (a) Preparation of transosseous holes on the posterior edge of the greater trochanter. (b) Two transosseous sutures. The more proximal suture included the pyramidalis tendon and the more distal one included the remaining rotator musculature. (c) Final result of the repair.
All the patients received the same postoperative rehabilitation protocol. Walking was initiated 24h after surgery and patients were specifically recommended that they avoid hyperflexion of the hip during the first 3 months. Crutches were recommended while walking for at least the first 3 weeks after surgery, after which they were used prn.
Statistical analysisThe data obtained during follow up were entered into a database with protected introduction, performed with the MS-ACCESS 2013 software program. Descriptive statistics were used to present the cohort's characteristics. Statistical analyses, to evaluate the differences between patients with and without dislocation, were performed using Student's t-test for continuous variables and Pearson's chi-squared test to compare categorical variables. Likewise, survival and risk function were studied by means of the Kaplan–Meier method, considering the appearance of dislocation of the total hip prosthesis as the final event, with a 95% confidence interval (CI). A p value of <0.05 was deemed statistically significant. Statistical analyses were performed using the SPSS 20 software program (Australia, 2012, SPSS Inc.) (IBM Corp., IBM SPSS Statistics for Windows, Version 20.0, Armonk, NY).
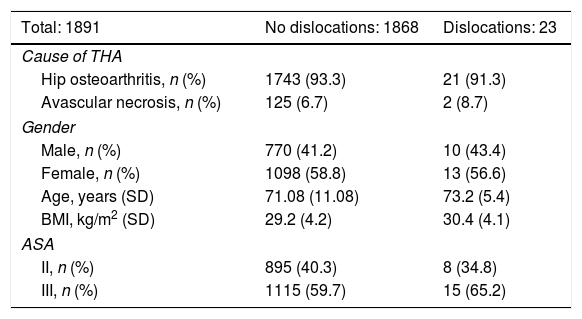
ResultsTwenty-three (23) early dislocations occurred, meeting the inclusion criteria of the 1891 hips that underwent THA by means of a posterior approach with repair of the capsule and external rotators (incidence: 1.21%). No statistically significant differences were detected when demographic data, patients’ clinical data, and surgery-related data were compared between those subjects that did not present early dislocation and those that did (Table 2).
Demographic data of study participants.
| Total: 1891 | No dislocations: 1868 | Dislocations: 23 |
|---|---|---|
| Cause of THA | ||
| Hip osteoarthritis, n (%) | 1743 (93.3) | 21 (91.3) |
| Avascular necrosis, n (%) | 125 (6.7) | 2 (8.7) |
| Gender | ||
| Male, n (%) | 770 (41.2) | 10 (43.4) |
| Female, n (%) | 1098 (58.8) | 13 (56.6) |
| Age, years (SD) | 71.08 (11.08) | 73.2 (5.4) |
| BMI, kg/m2 (SD) | 29.2 (4.2) | 30.4 (4.1) |
| ASA | ||
| II, n (%) | 895 (40.3) | 8 (34.8) |
| III, n (%) | 1115 (59.7) | 15 (65.2) |
ASA: American Society of Anesthesiologists Scale; THA: total hip arthroplasty; SD: standard deviation; BMI: body mass index.
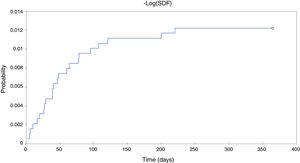
In patients with early dislocation, the mechanism of dislocation in 3 patients was trauma (13.1%) and in 20 it was casual following an impetuous movement (86.9%). In all the cases, the dislocation was posterior. One of the trauma cases also presented an associated ipsilateral periprosthetic fracture. Dislocations occurred between 2 and 220 days postop (mean of 35 days, SD 43.6). The overall survival mean taking dislocation as the final event in our sample (1891 hips) was 218 days (SD 0.4, 95% CI). In our study, the greatest likelihood of dislocation took place in the first 120 days (Fig. 2). More than eighty percent (86.6%) of the dislocations occurred in the first 120 days.
The first treatment in all cases was closed reduction and the use of a dislocation-prevention device, orthesis to limit hip flexion and abduction for 3 months, except in the case with the associated periprosthetic fracture, in which revision surgery was initially indicated. Nine of the remaining 22 patients did not have any other episode of recurrent dislocation with the closed reduction and use of the dislocation prevention device (40.9%). In 13 subjects, the dislocation relapsed; 10 presented 2 episodes of dislocation, and 3 patients had 3 or more episodes of dislocation. Nine patients underwent another surgery; in all of these cases, computed axial tomography was performed in which the orientation of the acetabular component was evaluated. Four of the patients with relapse of dislocation were treated conservatively, as they did not want another surgery, presented appropriate orientation of the components on tomography, and exhibited no further episodes of dislocation (Table 3).
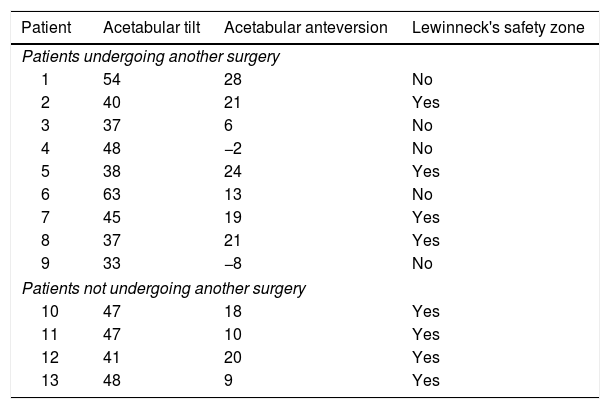
Tomographic measurements of the acetabular component in patients with more than one episode of dislocation of the total hip arthroplasty in our study, evaluating location within the Lewinneck's safety zone.
| Patient | Acetabular tilt | Acetabular anteversion | Lewinneck's safety zone |
|---|---|---|---|
| Patients undergoing another surgery | |||
| 1 | 54 | 28 | No |
| 2 | 40 | 21 | Yes |
| 3 | 37 | 6 | No |
| 4 | 48 | −2 | No |
| 5 | 38 | 24 | Yes |
| 6 | 63 | 13 | No |
| 7 | 45 | 19 | Yes |
| 8 | 37 | 21 | Yes |
| 9 | 33 | −8 | No |
| Patients not undergoing another surgery | |||
| 10 | 47 | 18 | Yes |
| 11 | 47 | 10 | Yes |
| 12 | 41 | 20 | Yes |
| 13 | 48 | 9 | Yes |
Revision surgery consisted, above all, of correcting the orientation of the components. In one case, a constrained cup was used. As far as postoperative complications are concerned, there were 2 periprosthetic infections, one acute and another one chronic; 3 dislocations of the revision surgery, and one demise due to septic shock resulting from hospital-acquired pneumonia. In the dislocations following revision surgery, 2 patients displayed dislocation after an impetuous movement and another patient after a fall. All were treated by closed reduction and presented no further episode of dislocation. Mean follow-up time was 34 months (range 12–66 months).
DiscussionDislocation following primary THA is the second most common complication after loosening. Nevertheless, it is a devastating complication for both the patient and the surgeon, as it may require hospitalization or prolonged rehabilitation, or additional surgical treatment.13 In our study, overall incidence of dislocation in our study was 1.2% and the greatest probability of dislocation was within the first 120 days. Revision surgery was required by 43.5% of the patients with dislocation.
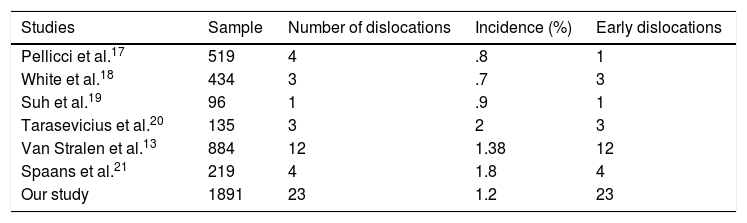
The published dislocation rate in primary hip prosthesis using a posterior approach is highly variable, between .3 and 9.7%.14,15 It is difficult to compare these rates in the literature, given that dislocation following THA is a multifactorial event.14,16 When comparing our results with other studies of transosseous reinsertion of the external rotators,14,17–21 we find a very similar incidence of dislocation (Table 4). Robinson et al. were the first to report that repair of the capsule and reinsertion of the external rotators might lower the incidence of dislocation from 7.5 to 1% in patients undergoing THA by means of a posterior approach.22 In their metaanalysis, Kwon et al. reported a relative risk of dislocation 8 times higher if soft tissue is not repaired.23 However, factors related to the patient, implants, and surgical technique have been reported that can have a bearing on the rate of dislocation.14 The following factors have been reported as factors that affect dislocation: age >70 years, being female, medical comorbidities, muscle status, and patient's education.5,21 In our study, the mean age was 73 years (SD 11 years), with 16 of the 23 dislocated patients being over the age of 70 years (69.5%). Likewise, there were more cases of dislocation among females 13/23 (56.5%); however, the overall rates of dislocation were very similar in both women (1.28%) and men (1.14%). ASA III also presented in most of the dislocated patients (65.2%). Another relevant point is the implants and surgical technique for their proper placement. Lewinnek et al. described the safety zone in 40±10° of acetabular tilt and 15±10° of acetabular anteversion, pointing out that correct component placement should avoid dislocation of THA.24 However, some studies show that, despite proper placement of the acetabulum, dislocations still occur. In their study, Abdel et al. reported that in 58% of their dislocations, the components displayed correct acetabular placement.25 In our study, of the dislocated patients on tomography, 61.5% of the patients presented dislocation despite being within Lewinnek's safety zone. In light of this problem, recent years have witnessed new concepts, such as combined anteversion, combined dynamic anteversion, and the lumbar-pelvic-femoral balance.26,27 Therefore, soft tissue repair is only one of the factors involved.
There is currently no consensus as to how best to perform this repair of the external rotators.14,17–21 Spaans et al., in their study that compared transosseous repair and transmuscular repair, revealed no differences in the rate of dislocation or as regards any other kind of complication, concluding that both reconstruction techniques are appropriate and equally efficacious.21 In our study, all the repairs were performed using a transosseous reinsertion, since we agree with the literature that reports transosseous reinsertion to be stronger than transmuscular reinsertion and that it is the most anatomical repair.14,20 It is worth pointing out that transosseous reinsertion has been reported to weaken the bone, which can cause failure in reinsertion and fractures due to trochanteric avulsion.18,21
Follow-up time is another issue, given that it plays a major role in the final incidence of dislocation. This figure differs across studies, although greater incidence is seen within the first 6 months.14,17–21 In our study, the greatest risk of dislocation was seen in the first 120 days. Only 3 patients presented dislocation after 120 days. Dislocation of a THA, in addition to being clinically relevant for the patient, is also highly significant in economic terms. This means that a dislocation represents a significant expense for the healthcare system. More important is the fact that close to half of the cases of dislocation required surgical revision.4,28 In our study, 10 cases needed revision (43.7%), one of them for an associated periprosthetic fracture. That is why we believe that any factor that can decrease the incidence of dislocation is important.
To the best of our knowledge, this is the study with the largest sample of patients undergoing primary THA using the posterior approach with repair of the capsule and transosseous reinsertion of the external rotators. As limitations of our work, it must be pointed out that, while it started as a prospective study, collection was retrospective, with the limitations that this kind of study entails. Moreover, there was not control group comprised of patients undergoing THA without soft tissue repair or with a transmuscular repair.
Our study concurs with the literature in that repair of the capsule and transosseous reinsertion of the external rotators can lower the incidence of dislocation in patients undergoing THA by means of a posterior approach. In addition, we agree with the literature that dislocation is a multifactorial event, which is why we highlight the importance of the capsule repair and rotator reinsertion, since it is a factor that can easily be controlled by the surgeon.
Level of evidenceLevel of evidence II.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Hernández A, Nuñez JH, Mimendia I, Barro V, Azorin L. Luxación temprana en artroplastias total de cadera primarias realizadas mediante vía posterior con reparación capsular y de rotadores externos. Rev Esp Cir Ortop Traumatol. 2018;62:421–427.