The treatment of rhizarthrosis using trapeziometacarpal prostheses (TMP) is increasing. Complications may lead to loss of the implant and result in salvage surgery. Our aim was to assess major complications with the use of some TMP models and their rescue.
Material and methodRetrospective study on TMP implanted between 2006 and 2021. Models studied: Arpe®, Elektra®, Ivory®, Maïa®, Isis® and Touch®. Demographic data were assessed, implant placement by radiographic study, technical data, complications, salvage surgeries and final survival.
ResultsReview of 224 TMP, 45 Arpe® (95.5% survival, rate follow-up [R] 6–16 years), 5 Elektra® (80% survival, R 13–14), 14 Ivory® (92.8% survival, R 9–11), 7 Maïa® (100% survival, R 8–9), 115 Isis® (99.1% survival, R 1–8), 38 Touch® (100% survival, R 1–4). The medial angle of the dome with the proximal articular surface of the trapezium in the lateral plane, was: Arpe®: 8.85°, Elektra®: not assessable, Ivory®: 6.6°, Maïa®: 14.4°, Isis®: 3.8°, and Touch®: 5.95°. The Isis® was placed 100% with scopic guidance presenting a significantly lower angle respect to the medial angle of the dome with the proximal articular surface of the trapezium. As main complications, we observed 3.5% of dislocations and 4% of mobilisations, with the Elektra® being responsible for 47% of these. Nineteen salvage surgeries were performed, with 3% of the implants being lost.
ConclusionsDislocation and mobilisation are the most observed complications, the Elektra® responsible for almost half of them. Correct placement and implant design appear to be crucial to avoid them in the short and long term.
El tratamiento de la rizartrosis del pulgar mediante el uso de prótesis trapeciometacarpianas (PTM) está en continua expansión. Las complicaciones son temidas y pueden ocasionar pérdida del implante o cirugías de rescate, por lo que nuestro objetivo fue valorar las de mayor riesgo con el uso de varios modelos de PTM y su reparación.
Material y métodoEstudio retrospectivo sobre las PTM implantadas entre 2006 y 2021. Como modelos estudiados estuvieron: Arpe®, Elektra®, Ivory®, Maïa®, Isis® y Touch®. Se realizó una valoración de datos demográficos, técnica, estudio radiográfico de colocación, complicaciones, rescate y supervivencia.
ResultadosRevisión de 224 PTM, 45 Arpe® (supervivencia 95,5%, rango de seguimiento en años [R] 6-16), cinco Elektra® (supervivencia 80%, R 13-14 años), 14 Ivory® (supervivencia 92,8%, R 9-11), siete Maïa® (supervivencia 100%, R 8-9), 115 Isis® (supervivencia del 99,1%, R 1-8) y 38 Touch® (supervivencia 100%, R 1-4). Ángulo medio de la cúpula con la carilla articular proximal del trapecio en el plano lateral: Arpe®: 8,85°; Elektra®: no valorable; Ivory®: 6,6°; Maïa®: 14,4°; Isis®: 3,8°, y Touch®: 5,95°. La Isis® se colocó en 100% con guía escópica, presentando significativamente un menor grado con respecto al ángulo medio de la cúpula con la carilla articular proximal del trapecio. Las complicaciones fueron 3,5% luxaciones y 4% movilizadas; la Elektra® fue responsable de 47% de estas. Se realizaron 19 cirugías de rescate, perdiéndose 3% de los implantes.
ConclusionesLa luxación y la movilización han sido las complicaciones más observadas, siendo la Elektra® responsable de casi la mitad de ellas. La correcta colocación de la cúpula y el diseño del implante parecen ser cruciales para evitarlas a corto y largo plazo.
Using a trapeziometacarpal prosthesis (TMP) to treat thumb rhizarthrosis is increasing practice, especially in Europe, and has become the technique of choice for many surgeons, since it restores biomechanics and achieves better and faster results than other classical techniques.1–3
Many designs have been developed and used since the late 20th century. De la Caffinière designed what was termed the first generation of TMP in the early 1970s; it was a cemented implant that had high rates of loosening and disappointing long-term results.4 Years later, in the 1990s, models termed second generation were designed, and presented improvements that helped reduce implant failure, such as anatomical designs, modularity, porous titanium, or hydroxyapatite coatings. Technical improvements in implantation appeared later, such as the use of intraoperative fluoroscopy, termed third generation, using the dual mobility concept as inspired by the total hip prosthesis.2
However, the risk of complications is always present; these can be major, potentially leading to loss of the implant, such as infection, dislocation, or loosening, or minor, less likely to jeopardise the survival of the prosthesis, such as de Quervain's tenosynovitis, tenosynovitis of the flexor carpi radialis or pollicis longus, or lesions of the sensitive branches of the radial nerve at the level of the surgical approach. There are several systematic reviews on the different models marketed that highlight these complications.5–7 The variety of implants that we have used and that are available, together with the progressive increase in their indication in our setting, were decisive in initiating this study and in assessing the rationale for their use.
The aim of our study was to review the major complications that we have observed in our experience with the use of different TMP models, and to evaluate the causes of failure and salvage techniques used since we began to implant them in 2006.
Material and methodRetrospective observational study of TMPs implanted in our institution's hand unit between March 2006 and June 2021. The review included all patients diagnosed with initial grade III or IV rhizarthrosis of the thumb (scaphotrapeziotrapezoid impingement, without clear bone contact),8 who underwent placement of a primary TMP with at least one year of clinical and radiological follow-up.
Those who did not meet the minimum clinical or radiological follow-up were excluded. Demographic data such as age, sex, laterality, dominance, and disease progression time were collected.
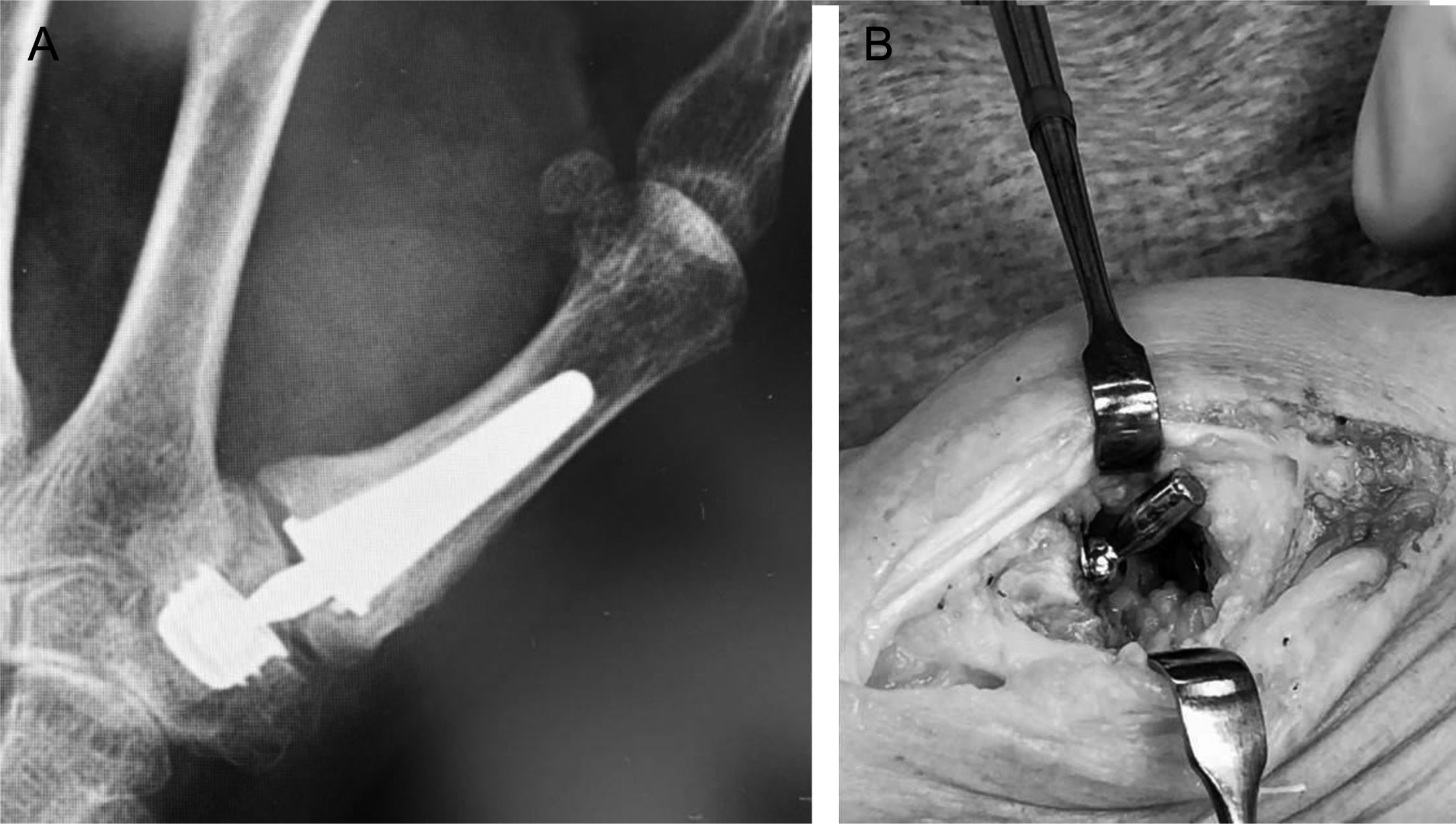
Implant placement was assessed by radiography, where special attention was paid to the cup at the level of the trapezium. For this purpose, the angle between the cup orientation and the proximal articular surface of the trapezium (PAST) was measured in the first postoperative radiographic control, considering an angle close to or greater than 20° a risk factor for dislocation or failure of the implant, especially in the mediolateral plane.9,10 Software for the visualisation of medical and radiological images for diagnostic use, RAIM Viewer version 2.5.0, was used to calculate the radiographic measurements (Fig. 1). Surgical technical data were also reviewed, such as the use or otherwise of fluoroscopy for implantation with guide wire in the trapezium or the use of cannulated material for reaming the cup.
(A) Dislocated Touch® prosthesis in the immediate postoperative period; showing a proximal articular surface of the trapezium (PAST) angle greater than 16°, the implant was placed without the aid of fluoroscopy. (B) Isis® prosthesis placed with the aid of fluoroscopy and reaming guide wire; a PAST angle close to 0°can be measured.
Six implant models were used; this variety is due to the more than 15 years’ interval between the oldest and the most modern. Some have been discontinued, such as the Arpe®; others have been discontinued due to poor results, such as the Elektra®; others have been discontinued for other business reasons, and others, such as those with dual mobility, appeared later.
The general characteristics of the implants were as follows: all were modular, cementless, patella-type, anatomically designed prostheses.
- 1.
Arpe® (Arpe® (Zimmer Biomet, Warsaw, IN, USA): hydroxyapatite coated cup and metacarpal stem. Hemispherical press-fit cup. Metal-polyethylene (MP) bearing.
- 2.
Elektra® (Small Bone Innovations International, ZA Les Bruyères, Péronnas, France): hydroxyapatite coated components. Cannulated conical cup, threaded, titanium alloy stem, and cobalt chrome cup. Cobalt chrome metal-on-metal (MM) bearing.
- 3.
Ivory® (Stryker Corporate, Kalamazoo, MI, USA): Hydroxyapatite-coated, double-coned cup and press-fit. MP bearings.
- 4.
Maïa® (Groupe Lépine, Lyon Nord, France): hydroxyapatite-coated and porous titanium. Titanium alloy cup and stem. Hemispherical cup with press-fit and 4 spikes for stability. MP bearings.
- 5.
Isis® (Evolutis, Roanne, France): porous titanium coated. Threaded cup with truncated cone shape, semi-constrained with slight pistoning which reduces trapezium stresses. MP bearings.
- 6.
Touch® (KeriMedical, Les Acacias, Switzerland): dual mobility prosthesis, coated with porous titanium and hydroxyapatite. The cup has 2 available designs: hemispherical or conical. MP bearings.
The major complications observed, which put the implant at risk or caused its loss (dislocation, mobilisation, trapezium, or metacarpal fracture, infection, disabling trapeziometacarpal or scaphotrapeziometacarpal pain or scaphotrapeziometacarpal pain) were recorded; the surgical salvage techniques used were also evaluated. Finally, the survival of the implant at the last check-up was evaluated.
Statistical analysisStatistical significance tests were performed using the SPSS® 20.0 programme for Windows (SPSS Inc., Chicago, IL, USA) taking p<.05 as statistically significant. For the statistical analysis of quantitative variables, the Mann–Whitney U was used and for the study of qualitative variables, the χ2 test. The Kruskal–Wallis test was used for the comparative study of the overall PAST angle, and the Mann–Whitney U test was used for the comparative study of the PAST angle separately between the different types of prosthesis. Continuous variables were analysed using the median and the 95% confidence interval. Finally, categorical variables are shown as percentages.
ResultsA total of 224 TMPs implanted over the 15-year period described (208 patients, 16 bilateral) met the clinical and radiological follow-up criteria and were therefore included in the study; they had a mean age of 59 years (40–78), 176 were women (85%) and the dominant side was affected in 84 patients (45%).
Regarding follow-up time, 30 prostheses exceeded 10 years, with a range (R) between 10 and 16 years, 57 exceeded 5 years (R: 5–9), 53 exceeded 3 years (R: 3–4), and 84 at least one year (R: 1–2).
The following models were implanted: 45 Arpe®, between 2006 and 2016, 5 Elektra®, between 2008 and 2009, 14 Ivory®, between 2011 and 2013, 7 Maïa®, between 2013 and 2014, 115 Isis®, between 2014 and 2021, and 38 Touch®, between 2018 and 2021.
Table 1 summarises the general characteristics of each TMP, the PAST angle and whether intraoperative fluoroscopy was used for placement. According to the prosthesis model, we observed the following major complications along with the salvage surgery used if required, in addition to the median survival of each implant at last follow-up (Table 2):
- -
Arpe®: 3 dislocations, 2 cup loosenings, one intraoperative trapezius fracture, one infection, and one intolerable trapeziometacarpal pain. One of the dislocations was traumatic after 3 weeks and was resolved by closed reduction, with no further complications. Another dislocation occurred after 2 months due to malposition of the cup, and was resolved by replacement of the cup to a retentive cup plus cerclage of the trapezium due to intraoperative fracture; after 5 years, further salvage was required due to pain by resection arthroplasty with palmaris longus hemitendon interposition (RAI) (Fig. 2). The third dislocation of this model was resolved with change to a retentive cup, after 7 months, with no further complications. The case of trapeziometacarpal pain due to loosening of the implant, uncontrollable with conservative treatment, required salvage with RAI after 2 years. An infection after 2 months was resolved with surgical lavage and antibiotic treatment. An intraoperative trapezium fracture during preparation of the cup was resolved with autologous bone grafting. Survival after 6 to 16 years was 95.5%.
Figure 2.(A) Arpe® prosthesis with very inclined cup, proximal articular surface of the trapezium angle of 27°. (B) Implant dislocation. (C) Rescue with retained and reoriented cup complicated by trapezium fracture requiring wire cerclage. (D) Final salvage: resection of the trapezium and tenosuspension.
(0.29MB). - -
Elektra®: all the cups of this implant loosened over the first 6 months, 3 of which were completely dislocated by loosening. Of the loosened cups, one required salvage with a cemented cup after one year, another loosened with subsequent dislocation and required salvage with a cemented cup after 5 years, and a third loosened implant was salvaged with a cemented cup; later, due to poor clinical progress, it was salvaged with RAI after 7 years (Fig. 3). One of the loosened implants, and another loosened implant with subsequent dislocation, tolerated the procedure well, and the patients did not require further procedures. Survival after a minimum follow-up of 13 years is 80%, taking into account that all the cups loosened.
- -
Ivory®: 2 loosenings of the cup were observed, one scaphotrapeziotrapezoid pain and one trapeziometacarpal pain that could not be controlled conservatively. The 2 patients whose cups loosened died after more than 2 years of follow-up. The patient who presented with scaphotrapeziotrapezoid pain required salvage surgery after 5 years by resection of the distal pole of the scaphoid plus interposition of the palmaris longus muscle hemitendon, with significant subsequent improvement without affecting the implant. The patient who presented uncontrollable trapeziometacarpal pain required salvage surgery with RAI at one year. Survival after 9 to 11 years of follow-up was 92.8%.
- -
Maïa®: we did not observe any major complication with this implant after a minimum follow-up of 8 years; survival was 100%.
- -
Isis®: 3 trapezium fractures were observed which required intraoperative salvage with a cemented cup, and 2 intraoperative metacarpal fractures were resolved, one with wire cerclage and the other with immobilisation. A traumatic dislocation after 3 years with subsequent recurrence due to peripheral polyethylene breakage required salvage surgery with RAI; this case coincides with one of the intraoperative metacarpal fractures (Fig. 4). Another patient presented with trapeziometacarpal pain requiring salvage surgery, with periprosthetic ossification leading to loosening of the neck, which required re-impacting and peritrapezial bone resection (Fig. 5). Survival after a follow-up of between 1 and 8 years was 99%.
Figure 4.(A) Isis® prosthesis that during surgery suffered a first complication with fracture of the metacarpal, resolved with wire cerclage. (B) Three years later, traumatic dislocation that caused peripheral breakage of the polyethylene. (C) Salvage with resection of the trapezium and tenosuspension, due to recurrent dislocation.
(0.2MB). - -
Touch®: we observed one dislocation due to manipulation in the immediate postoperative period that was resolved by closed reduction, without further complications. An intraoperative metacarpal fracture was treated with wire cerclage, with no further complications. Implant survival was 100% after a follow-up of one to four years.
Main characteristics of the different prosthesis models, use of fluoroscopy as guidance and PAST angle measured in each implant.
| Model | Cup | Bearing | Use of fluoroscopy as guidance, % | PAST angle (°), median (95% CI) |
|---|---|---|---|---|
| Arpe® | Spherical, press-fit | MP | 0 | 7 (5–10) |
| Elektra® | Conical/cannulated/threaded | MM | 0 | – |
| Ivory® | Truncated cone press-fit | MP | 0 | 5.85 (1.5–9) |
| Maïa® | Spherical, press-fit | MP | 0 | 8 (4.5–46) |
| Isis® | Truncated conical/threaded/semi-constrained | MP | 100 | 2.5 (2–3.4) |
| Touch® | Spherical, press-fit/dual mobility | MP | 75 | 5 (3.5–8) |
95% CI: 95% confidence interval; MM: metal–metal; MP: metal–polyethylene; PAST: proximal articular surface of the trapezium.
Number of different implants, major complications, and final survival observed.
| Model, n | Dislocation, n (%) | Loosening, n (%) | Infection, n (%) | TMC pain, n (%) | STT pain, n (%) | Loss of implant, n (%) | Survival, % (range follow-up years) |
|---|---|---|---|---|---|---|---|
| Arpe®, 45 | 3 (6.6) | 2 (4.4) | 1 (2.2) | 1 (2.2) | 0 | 2 (4.5) | 95.5 (6–16) |
| Elektra®, 5 | 3 (60) | 5 (100) | 0 | 0 | 0 | 1 (20) | 80 (13–14) |
| Ivory®, 14 | 0 | 2 (14) | 0 | 1 (7) | 1 (7) | 1 (7) | 92.8 (9–11) |
| Maïa®, 7 | 0 | 0 | 0 | 0 | 0 | 0 | 100 (8–9) |
| Isis®, 111 | 1 (0.9) | 0 | 0 | 0 | 0 | 1 (.9) | 99.1 (1–8) |
| Touch®, 38 | 1 (2.6) | 0 | 0 | 0 | 0 | 0 | 100 (1–4) |
Intraoperative complications are excluded from the table (see text).
STT: scaphotrapeziotrapezoid; TMC: trapeziometacarpal.
Our analysis of the absolute values of the dislocations showed that the mean PAST angle of patients with dislocation was 11.7° versus 5.5° of patients who did not have dislocation; this is a statistically significant difference (p=.048).
Separate analysis of the different prosthetic models in relation to the PAST angle showed that the Isis® prosthesis has a significantly smaller angle than the rest of the models. However, we observed no differences when comparing the rest of the models with each other (Table 3).
Separate comparative analysis between the different prosthetic models in relation to the PAST angle in the lateral plane.
| Model vs. model | Comparison of PAST anglep |
|---|---|
| Arpe® vs. Ivory® | .289 |
| Arpe® vs. Maïa® | .601 |
| Arpe® vs. Isis® | <.001 |
| Arpe® vs. Touch® | .174 |
| Ivory® vs. Maïa® | .314 |
| Ivory® vs. Isis® | .061 |
| Ivory® vs. Touch® | .899 |
| Maïa® vs. Isis® | .012 |
| Maïa® vs. Touch® | .222 |
| Isis® vs. Touch® | <.001 |
Test used: Mann–Whitney U test.
PAST: proximal articular surface of the trapezium.
In bold, statistically significant result.
Overall, a total of 24 major complications were observed (10.7%), of which 8 were dislocations (3.5%) and 9 loosenings (4%). The Elektra® was responsible for 47% of these. Nineteen salvage surgeries were performed, losing 3% of the implants.
DiscussionThe implantation of a prosthetic material such as the TMP implies both short- and long-term follow-up, because multiple complications can occur, which must be resolved in the most appropriate and satisfactory manner possible.10–13
Most of our complications (70%) were dislocations and loosenings, and these occurred in the first years from implantation. In most, a single model of MM bearing implant and cannulated cup was responsible, which we no longer use.
Later models, of better design and implanted with greater technical rigour, especially in terms of cup orientation, have presented fewer complications. The systematic use of fluoroscopy as guidance and cannulated material as with the Isis® helped us to obtain better placement of the cup, which was quantifiable by measuring the PAST angle; we also observed that it significantly relates to the rate of dislocations in our sample.
Systematic reviews on TMPs stand out in the literature, such as that by Huang et al.,5 from 2015, where they observed that the main long-term complications were loosening and dislocation of the implant, and in turn the most frequent causes of surgical revision; these results coincide with those of our work. This study looked at mixed models of cemented prostheses such as the De la Caffinière, in which the main complication was loosening, reaching up to 52% in some studies, and non-cemented and non-constrained prostheses such as the Arpe®, whose main complication was dislocation. Overall failure rates of the implants were as high as 33%. Another systematic literature review was that by Ganhewa et al.,6 published in 2019. They evaluated the failures of multiple surgical techniques for the treatment of rhizarthrosis, including different implant models. They considered as failure the need to perform a secondary salvage procedure. They observed that there is an initial phase of high failure rate followed by a plateau phase where these stabilise until the implant reaches its useful life and an increase in the rate of complications recommences. A specific model in this study is worth mentioning, namely the Elektra®, which they present as one of the implants with the highest failure rate, more than double that of other models such as Arpe®, Maïa®, or Ivory®, coinciding with our experience, in which all cups presented early loosening. The study by Thorkidsen et al.14 on the possible causes of failure of the Elektra® concluded that it was not only due to the cannulated design of the cup, but also to its MM bearing, which causes early loosening due to osteolysis by metallic particles, which were accessing the paratracheal space through the cup orifice for cannulation and through its periphery. In 2020, Remy et al.7 published another meta-analysis including the work on TMP with ball-and-socket design, complications, salvage surgeries after failure, and functional results. They observed a rapid functional recovery in patients, which was then sustained over time. The overall reported failure rate of multiple models reviewed was 12% after a mean 49 months of follow-up, with cup loosening accounting for 84% of the surgical revisions; according to the paper, part of these may have been due to technical implantation errors, such as malpositioning of the cup. They also observed a very low rate of infections, 0.23%. In recent years, new implant designs with more reliable osseointegration materials, together with studies that improve the surgical technique for implant placement, mainly the cup, are improving the results in the first years of follow-up, which in some models even achieve 100% survival. The study by Cootjans et al.15 on the Arpe® prosthesis reported a survival rate of 96% of cases at 6.5 years. Goubau et al. report an average 5-year survival rate of 95% with the Ivory®.16 Longer term results can also be found, such as the work by Martin-Ferrero at 10 years with the Arpe®, with 93.4% survival,17 and 95% also at 10 years with the Ivory® prosthesis in the study by Tchurukdichian et al.18 Chiche et al.19 report 88% survival of the Maïa® at 12 years. Other more evolved models, considered third generation, with a dual mobility cup, have also demonstrated high short-term survival, as in the study on the Touch® by Gonzalez-Espino et al.,20 with 100% survival at more than one year, or in the medium term on the Moovis® by Martins et al.,21 with mean 5-year follow-up and also 100% implant survival. The Isis®, which is the implant that we placed the most in our series, shows very promising published results in the short term, with a 100% survival rate in the first 2 years of mean follow-up.22 It seems that the correct position of the cup is crucial to reduce the risk of major complications, such as dislocation, wear, or loosening23; it should be centred on the trapezium to provide stability and avoid fracture of the trapezium or contact of the neck with the edge of the polyethylene leading to wear and loosening. Duerinckx and Caekebeke9 published a study in 2016 to help in cup orientation. The proximal articular surface of the trapezium can serve as a reference line; they determined that the line representing the centre of range of motion forms an angle of 90° with respect to the proximal articular surface of the trapezium in the anteroposterior view and 83° in the lateral view. Therefore, the cup should be placed parallel to the articular surface of the trapezium. Brauns et al.10 published another work, based on that of Duerinckx and Caekebeke, where they recommend that the cup be placed parallel to the PAST to decrease the risk of dislocation; they also warn that the risk of complications is significantly increased when it goes beyond 20°, especially in the lateral plane. In our results we observed that the dislocated prostheses had a significantly greater PAST angle than the others, which seems to be in line with the aforementioned studies. The correct orientation of the cup could be an advantage in the long term to minimise the risk of loosening, polyethylene wear, and dislocations, as described by these authors.
In the short term, the studies have already demonstrated that the cup does not loosen or dislocate, but longer-term studies are needed to verify the survival of the implants. The limitations we found in our study are, firstly, the heterogeneity of the sample, with multiple models studied, according to the supply of implants and the situation at any given time; secondly, the follow-up time, which, although long with some models, is still short with others, the most modern; finally, it is a retrospective study performed in a single centre and not randomised.
ConclusionMajor complications observed in our experience with TMPs are rare in different implant models, with the exception of one with an MM bearing. Dislocation and loosening are the most prevalent and complex to resolve, requiring salvage surgeries that may involve the loss of the implant. Correct cup placement and implant design appear to be crucial to avoid these complications in the short and long term.
Level of evidenceLevel of evidence iv.
FundingThis research received no specific grant from any funding agency in the public, commercial or not-for-profit sector.
Conflict of interestsThe authors have no conflict of interests to declare.