To develop recommendations on the evaluation and management procedure in patients undergoing total knee replacement based on best evidence and the experience of a panel of experts.
MethodsA multidisciplinary group of 12 experts was selected that defined the scope, users and the document parts. Three systematic reviews were performed in patients undergoing knee replacement: (i) efficacy and safety of fast-tracks; (ii) efficacy and safety of cognitive interventions in patients with catastrophic pain, and (iii) efficacy and safety of acute post-surgical pain management on post-surgical outcomes. A narrative review was conducted on the evaluation and management of pain sensitisation, and about the efficacy and safety of pre-surgical physiotherapy. The experts generated the recommendations and explicative text. The level of agreement was evaluated in a multidisciplinary group of 85 experts with the Delphi technique. The level of evidence was established as well for each recommendation.
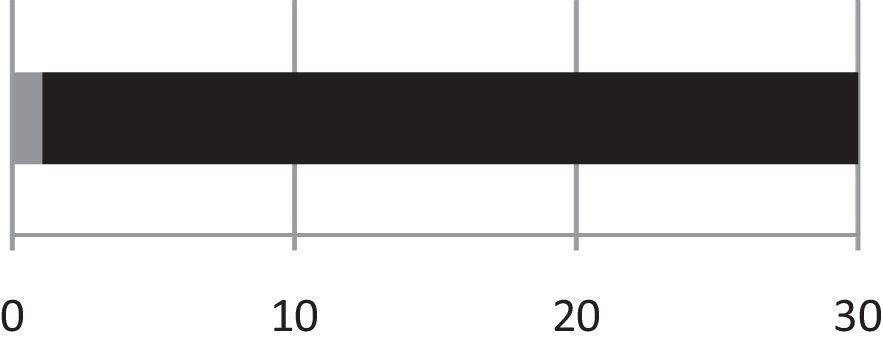
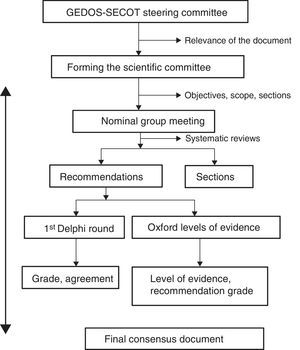
ResultsA total of 20 recommendations were produced. An agreement higher than 80% was reached in all of them. We found the highest agreement on the need for a full discharge report, on providing proper information about the process and on following available guidelines.
ConclusionsThere is consensus among professionals involved in the management of patients undergoing total knee replacement, in that it is important to protocolize the replacement process, performing a proper, integrated and coordinated patient evaluation and follow-up, paying special attention to the surgical procedure and postoperative period.
Desarrollar recomendaciones sobre el proceso de evaluación y manejo del paciente con artrosis de rodilla e indicación de artroplastia basadas en la mejor evidencia científica disponible y la experiencia de un panel de expertos.
MétodosSe seleccionó un grupo multidisciplinar de 12 expertos que definieron: alcance, usuarios, apartados del documento, revisiones sistemáticas a realizar y a quienes se asignaron tareas. Se realizaron 3 revisiones sistemáticas en pacientes con indicación de artroplastia de rodilla sobre: 1)eficacia y seguridad de los protocolos de fast-track; 2)papel de las intervenciones cognitivo-conductuales en sujetos con catastrofismo, y 3)efecto del control del dolor agudo posquirúrgico en los resultados. Se realizaron 2 revisiones narrativas sobre la sensibilización central en este grupo y sobre la eficacia de la rehabilitación preoperatoria. Los expertos redactaron los apartados y generaron las recomendaciones. Estas recomendaciones se consensuaron mediante la metodología Delphi en un grupo multidisciplinar de 85 expertos. Se estableció también el nivel de evidencia de cada recomendación.
ResultadosSe generaron 20 recomendaciones. Todas alcanzaron un nivel de acuerdo mayor del 80%. El mayor acuerdo se alcanzó en la necesidad de realizar informe de alta completo, en informar adecuadamente al paciente sobre el proceso y en seguir las recomendaciones de las guías clínicas disponibles.
ConclusionesExiste consenso entre los responsables del manejo de los pacientes con artrosis de rodilla e indicación de artroplastia en que es necesario protocolizar el proceso de sustitución articular, realizando una correcta evaluación y seguimiento del paciente, de forma integral y coordinada y con especial atención al procedimiento quirúrgico y al postoperatorio.
Knee osteoarthritis is a common disease which can affect up to 10% of the general population and cause incapacitating pain.1,2 Treatment is symptomatic and ultimately some patients require joint replacement surgery.3–5
When a patient presents with knee osteoarthritis symptoms and it is considered that joint replacement surgery might be necessary in the short or medium term, a long process commences the final outcome of which will depend on, in addition to the operation per se, the steps taken before and after surgery.6–9 The final objective is for the patient to lead an active life, free from pain.
A great many practitioners are involved in the care of the knee osteoarthritis patient for whom a joint replacement is indicated. These include: the primary care physician, nursing staff, anaesthetist, rheumatologist, trauma surgeon, rehabilitation specialist, physiotherapist and psychologist and the social worker. There is often little coordination between these practitioners and the patient suffers as a consequence of a lack of common objectives and integrated care protocols. The so-called fast-track protocols in knee arthroplasty were designed as systems to optimise the processes associated with the surgical procedure and have proven effective in streamlining the surgical process and improving patient satisfaction.10–12 However, these protocols do not cover aspects prior or subsequent to the operation, which also have an effect on outcomes.
The aim of this consensus document was to analyse the care process for patients with knee osteoarthritis for whom a knee arthroscopy was indicated from the time that arthroplasty was considered a possibility until one year after surgery, to then provide recommendations based on the best available evidence, and the experience and opinion of the practitioners involved. A multidisciplinary scientific committee was formed for the purpose, and all the individual phases of the process were considered (pre, peri and post-operative periods).
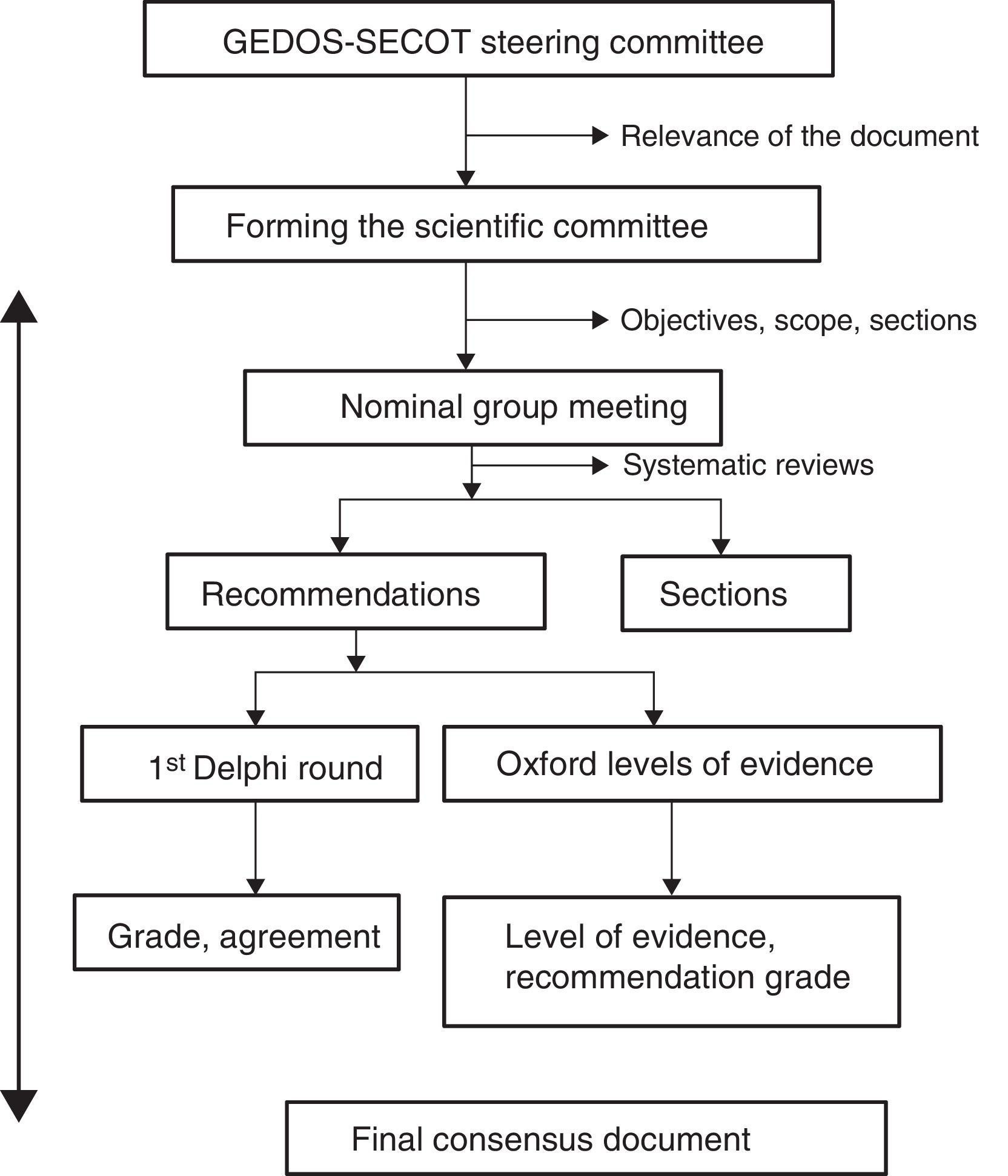
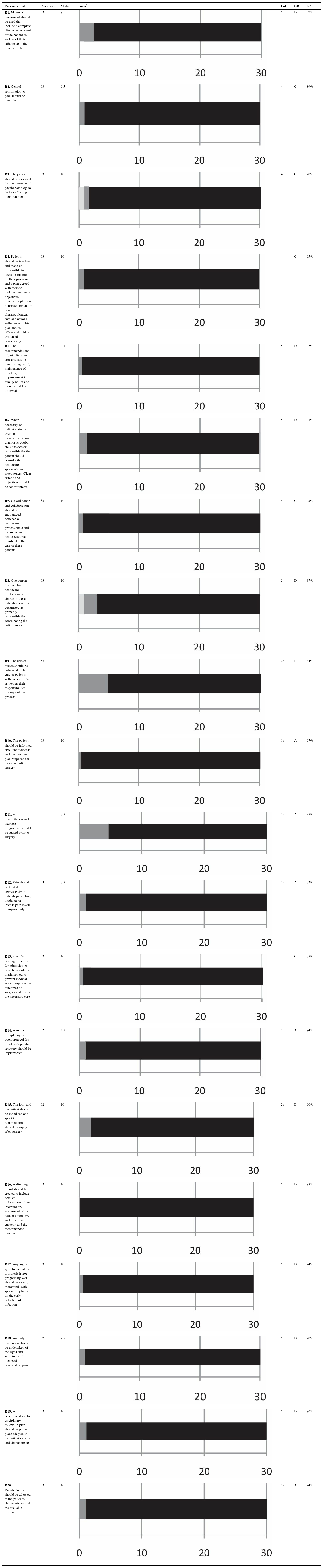
MethodsWe followed the Delphi technique to prepare the consensus.13 This system is based on presenting a panel of experts a series of questions independently and anonymously prepared by a scientific committee and, by repeated circulation of the responses of this group, adjusting these questions and establishing points of consensus (Fig. 1). The document was prepared entirely by the distribution of tasks and comments to the parties, with the help of systematic and narrative reviews of the literature, and methodological expert advice.
Phase 1. Consensus designThe initiative for undertaking the consensus came from the steering committee of the musculoskeletal pain study group of the Spanish Orthopaedic and Trauma Society (GEDOS-SECOT). A multidisciplinary steering group of 12 health professionals was established first (3 orthopaedic surgeons, 2 primary care physicians, 2 anaesthetists, 2 rehabilitation specialists, a nurse, a rheumatologist and a psychologist) with recognised experience in the field. In order to guarantee the panel's representativeness professionals were selected from different Spanish cities each from different hospitals. There were also 2 methodological experts.
The scope, objectives, users and sections of the consensus were decided at a first nominal group meeting. It was agreed to cover all the relevant aspects of the management of patients with knee osteoarthritis from the moment that arthroscopy is indicated (preoperative period: from the time that joint replacement surgery is decided until one week before the intervention), the operation (presurgical period: from one week prior to the intervention until 24h after it, or until discharge from hospital), and after one year postoperatively (postoperative period). It was agreed to undertake 3 systematic and 2 narrative literature reviews. It was also decided to wait for the results of the reviews to assign each panel member one or several sections of the consensus for drafting.
Phase 2. Systematic and narrative reviewsThree systematic reviews of the literature were undertaken on the efficacy and safety of fast track protocols, management of presurgical pain and of postsurgical pain long term, and interventions for catastrophic pain, and 2 narrative reviews on the efficacy of presurgical exercise on long-term postoperative function, and on the diagnosis and management of pain with central sensitisation.
The same review protocol was used for the systematic reviews. Studies were chosen that included adult patients for whom knee arthroplasty was indicated. Moreover, these studies had to analyse (according to the review) the efficacy and safety of the interventions described previously. Finally, only studies were included with the following designs: meta-analysis, systemic reviews, clinical studies and observational studies. The following bibliographic databases were screened in all the reviews: Medline (from its start until June 2015), Embase (from its start until June 2015) and Cochrane Library (from its start until June 2015). MeSH and free-text terms were used. For each review, 2 reviewers independently analysed the articles found through the search of the different bibliographic databases, as well as the detailed analysis of the articles included. The Oxford quality scale was used to evaluate the methodological quality of the studies included. Evidence tables were created describing the main characteristics of the studies included. The results of these systematic reviews were available to the steering group and were used to establish the evidence level of the recommendations.
Phase 3. Drafting of the consensus questionnaireThe various sections of the consensus were allocated to each group member. After completing a first draft of recommendations, the sections and recommendations were combined and edited for style. Then the document was circulated amongst the steering group and various corrections and comments made, and after repeating this process a final document was decided.
Phase 4. Delphi surveyA group of experts with 85 orthopaedic surgeons, anaesthetists, physician experts in rehabilitation and primary care, also including the steering group was formed (Annex 1). They were sent the questionnaire online, with the complete recommendations and instructions for them to vote (anonymously) on their grade of agreement with each of the consensus document recommendations. The grade of agreement was expressed by voting using a Likert scale from 1 (completely disagree) to 10 (completely agree). Agreement was defined if a score of 7 or more was achieved for each recommendation. The aggregated results of the Delphi technique were shown to all the panel members (modified Delphi). The recommendations with a grade of agreement (GA) less than 70% were reassessed and, if appropriate, were reedited and voted on in a second round.
Phase 5. Final consensus documentThe definitive document was drafted with all of this information. Each of the recommendations was assigned a level of evidence (LoE) and a grade of recommendation (GR) according to the recommendations of Oxford's Centre for Evidence Based Medicine,14 and a grade of agreement (GA) according to the Delphi technique results.
ResultsRecommendations for the management of patients undergoing knee arthroplastyThe patients to whom these recommendations apply are those with knee osteoarthritis and candidates for treatment with total knee arthroscopy or those who have already been treated by arthroscopy. Most of these patients present or have presented an advanced level of knee osteoarthritis causing them major symptoms of pain and loss of function. Furthermore, they have regularly tried different therapeutic options that have failed for some reason or another. The objective of these recommendations is to help the clinician in the management of these patients from the moment that arthroplasty is considered necessary until one year after the operation.
The following recommendations are presented grouped in 4 blocks. The first includes general recommendations to be applied to patients throughout the process, and in the other three specific recommendations are made for the preoperative, perioperative and postoperative periods. The recommendations and the results of the Delphi vote are shown in Table 1.
Recommendations and main results achieved in the Delphi including level of evidence, grade of recommendation and grade of agreement.a
| Recommendation | Responses | Median | Scoresb | LoE | GR | GA |
|---|---|---|---|---|---|---|
| R1. Means of assessment should be used that include a complete clinical assessment of the patient as well as of their adherence to the treatment plan | 63 | 9 | 5 | D | 87% | |
| R2. Central sensitisation to pain should be identified | 63 | 9.5 | 4 | C | 89% | |
| R3. The patient should be assessed for the presence of psychopathological factors affecting their treatment | 63 | 10 | 4 | C | 90% | |
| R4. Patients should be involved and made co-responsible in decision-making on their problem, and a plan agreed with them to include therapeutic objectives, treatment options – pharmacological or non-pharmacological – care and actions. Adherence to this plan and its efficacy should be evaluated periodically | 63 | 10 | 4 | C | 95% | |
| R5. The recommendations of guidelines and consensuses on pain management, maintenance of function, improvement in quality of life and mood should be followed | 63 | 9.5 | 5 | D | 97% | |
| R6. When necessary or indicated (in the event of therapeutic failure, diagnostic doubt, etc.), the doctor responsible for the patient should consult other healthcare specialists and practitioners. Clear criteria and objectives should be set for referral. | 63 | 10 | 5 | D | 95% | |
| R7. Co-ordination and collaboration should be encouraged between all healthcare professionals and the social and health resources involved in the care of these patients | 63 | 10 | 4 | C | 95% | |
| R8. One person from all the healthcare professionals in charge of these patients should be designated as primarily responsible for coordinating the entire process | 63 | 10 | 5 | D | 87% | |
| R9. The role of nurses should be enhanced in the care of patients with osteoarthritis as well as their responsibilities throughout the process | 63 | 9 | 2c | B | 84% | |
| R10. The patient should be informed about their disease and the treatment plan proposed for them, including surgery | 63 | 10 | 1b | A | 97% | |
| R11. A rehabilitation and exercise programme should be started prior to surgery | 61 | 9.5 | 1a | A | 85% | |
| R12. Pain should be treated aggressively in patients presenting moderate or intense pain levels preoperatively | 63 | 9.5 | 1a | A | 92% | |
| R13. Specific hosting protocols for admission to hospital should be implemented to prevent medical errors, improve the outcomes of surgery and ensure the necessary care | 62 | 10 | 4 | C | 95% | |
| R14. A multi-disciplinary fast track protocol for rapid postoperative recovery should be implemented | 62 | 7.5 | 1c | A | 94% | |
| R15. The joint and the patient should be mobilised and specific rehabilitation started promptly after surgery | 62 | 10 | 2a | B | 90% | |
| R16. A discharge report should be created to include detailed information of the intervention, assessment of the patient's pain level and functional capacity and the recommended treatment | 63 | 10 | 5 | D | 98% | |
| R17. Any signs or symptoms that the prosthesis is not progressing well should be strictly monitored, with special emphasis on the early detection of infection | 63 | 10 | 5 | D | 94% | |
| R18. An early evaluation should be undertaken of the signs and symptoms of localised neuropathic pain | 62 | 9.5 | 5 | D | 90% | |
| R19. A coordinated multi-disciplinary follow-up plan should be put in place adapted to the patient's needs and characteristics | 63 | 10 | 5 | D | 90% | |
| R20. Rehabilitation should be adjusted to the patient's characteristics and the available resources | 63 | 10 | 1a | A | 94% |
GA: grade of agreement; GR: grade of recommendation; LoE: level of evidence.
In the pre and post-operative period it is recommended that patients with knee osteoarthritis should be assessed using specific scales and questionnaires that evaluate their most relevant health aspects. Only the systematic use of validated scales will enable satisfactory assessment of the outcomes of the procedures performed.
Objective evaluation of the pain levels is recommended (using the visual analogue scale [VAS]),15 the use of specific joint function scales (such as the Western Ontario and McMaster Universities Osteoarthritis Index [WOMAC]),16,17 evaluating with a specific knee scale such as the American Knee Society Score (AKSS)18 or that of the Hospital for Special Surgery (HSS)19 and using a general quality of life evaluation scale (SF-36, SF-12, OAKHQOL).20 Similarly, the evaluation of other psychosocial elements should be considered such as anxiety, depression and catastrophising (Hospital Anxiety and Depression Scale and Pain Catastrophizing Scale),21–23 evaluating compliance and adherence to treatment (such as the Morisky-Green test),24,25 and adverse events.26
R2. Central sensitisation to pain should be identified (LoE 4; GR C; GA 89%)Central sensitisation to pain is a complex phenomenon that occurs in the central nervous system (from the dorsal horn of the spinal cord to the brain). It regularly appears in patients with chronic pain of moderate or severe intensity, and is common in patients with osteoarthritis.27 It is shown clinically and pathophysiologically in the form of allodynia and hyperalgesia, which extend beyond the affected joint, and is associated with disability and major deterioration in quality of life.28
Central sensitisation to pain can be assessed by quantitative sensory testing.29 The degree of central sensitisation in a subject is associated with the intensity and onset time of their pre and postoperative pain.30
In patients with pain for whom arthroplasty is indicated, it is essential to prevent this phenomenon by appropriate control of perioperative pain.31
R3. The patient should be assessed for the presence of psychopathological factors affecting their treatment (LoE 4; GR C; GA 90%)There are psychopathological factors (dysthymia, obsessive compulsive tendencies, rigid and non-adaptive confrontational skills, psychotic characteristics of schizoid or paranoid personality disorder)32 that should be considered before deciding the surgical plan, either to evaluate possible psychiatric-psychological interventions, or to interpret the results of surgery performed, or both.
Patients with catastrophising thoughts tend to magnify facts and their negative consequences33 and present a high risk of developing chronic postoperative pain.34 Intervention prior to surgery is recommended.
Subjects with unexplained hyperactivity, irritability and aggressiveness might require a more structured functional rehabilitation programme, although they will continue to be at greater risk of developing a less predictable response in relation to postoperative pain.35
R4. Patients should be involved and made co-responsible in decision-making on their problem, and a plan agreed with them to include therapeutic objectives, treatment options–pharmacological or non-pharmacological—care and actions. Adherence to this plan and its efficacy should be evaluated periodically (LoE 4; GR C; GA 95%)With regard to co-responsibility in approaching the disease, it has been demonstrated that giving the patient personalised evidence-based information enables shared decision-making, creating more realistic expectations about treatments, and thus optimising choice of treatment. Furthermore, adherence, active coping and satisfaction of both patients and practitioners has been improved in this way.36–39
Evaluation of efficacy, safety and adherence to the various treatments before and after surgery is essential for osteoarthritis.3,24,25 Once an action plan has been established, it should be evaluated initially after 2–4 weeks, or even before for elderly or polymedicated patients or those with associated comorbidities.26 This first assessment should focus on detecting adverse events and evaluating the need for analgesic dose titration in relation to the response obtained.
R5. The recommendations of guidelines and consensuses on pain management, maintenance of function, improvement in quality of life and mood should be followed (LoE 5; GR D; GA 97%)There are currently many clinical guidelines to help practitioners in the management of patients with osteoarthritis. The main national and international rheumatology and orthopaedic scientific organisations such as the Osteoarthritis Research Society International (OARSI),3 the American College of Rheumatology (ACR),40 the European League Against Rheumatism (EULAR)41,42 and the American Academy of Orthopaedic Surgeons (AAOS) (together with the Appropriate Use Criteria (AUC), included on the AAOS website) have devoted effort and resources to developing complete and well documented guidelines.43 The recommendations of the Spanish Rheumatology Society (SER) (SER)44 and the Spanish Society of Family and Community Medicine (SEMFyC) are also available.39
The recommendations in these guidelines (pharmacological and non-pharmacological) are based on the best available scientific evidence and the consensus of different practitioners such as rheumatologists, nurses, orthopaedic surgeons, rehabilitation specialists and psychologists, and thus offer a holistic and multidisciplinary approach to the disorder.40,41 Furthermore, the guidelines offer procedures and recommendations so that healthcare professionals can offer a clearer explanation of the proposed treatment and follow-up and their reasons. Therefore, both the patient and their families or carers can gain information that is better adjusted to their features and needs, which increases the likelihood of success.45
Finally, the advisory nature of these guidelines and consensuses should be highlighted. It is essential that with this available information, a consensus is reached between the healthcare practitioner and the patient on the approach to be taken.
R6. When necessary or indicated (in the event of therapeutic failure, diagnostic doubt, etc.), the doctor responsible for the patient should consult other healthcare specialists and practitioners. Clear criteria and objectives should be set for referral (LoE 5; GR D; GA 95%)It is recommended that the primary care physician (PA), or any other health professional responsible for the patient, in cases where they consider it necessary (especially if there is ineffective pain control or relevant impact on the patient's functionality and/or quality of life) should consider referral to another practitioner. This can take place at any time in the clinical progress of the disease and the patient can be referred to the rheumatologist, orthopaedic surgeon, rehabilitation specialist, physiotherapist, clinical psychologist, to a pain clinic, etc.
Even though it is difficult to define valid or generally feasible criteria for referral due to the different care organisations within Spain's autonomous regions or districts, given the available evidence, the following criteria for referral from AP to specialised care are recommended46–49: a diagnosis of osteoarthritis under the age of 40 years, diagnostic doubt or suspected secondary osteoarthritis, symptoms, warning signs, deformity with severe functional limitation, articular block, incapacitating pain or insufficient response to treatment, assessment that surgery is indicated, and the need for diagnostic tests or procedures that are not available in the area of PA.
R7. Co-ordination and collaboration should be encouraged between all healthcare professionals and the social and health resources involved in the care of these patients (LoE 4; GR C; GA 95%)Osteoarthritis is a chronic and complex disease, the care of which routinely involves different healthcare professionals, who often assess and treat these patients independently. This can mean that tests are duplicated, that contradictory messages are conveyed, and that the risk of adverse events is increased, etc.50
Co-ordinated, multidisciplinary care is recommended to ensure integral care and continuity of care for patients with osteoarthritis who are to undergo an arthroplasty. This interdisciplinary care requires models of communication, interaction and “shared objectives and care” to enable appropriate information exchange for decision making. It requires flexible agreement and consensus within the competence framework of each professional, and interventions must be optimised to prevent duplication of services and to maximise healthcare outcomes.47,51–53
R8. One person from all the healthcare professionals in charge of these patients should be designated as primarily responsible for coordinating the entire process (LoE 5; GR D; GA 87%)It is recommended that one of the practitioners involved in the care of the osteoarthritis patient should be in charge of integrating and coordinating their care throughout the care process, including surgical treatment.
Perhaps the PC physician is the most appropriate, not only because PC is the main access route to the healthcare system, but also because of their accessibility, their knowledge of the patient's bio-psycho-social environment (integral vision) and their experience in managing and coordinating chronic processes and sharing the management of care with other health professionals.7,54,55
Improved information flow and care shared with all the practitioners involved in the management of patients with osteoarthritis should be their primary objective.56
R9. The role of nurses should be enhanced in the care of patients with osteoarthritis as well as their responsibilities throughout the process (LoE 2c; GR B; GA 84%)This can be achieved through creating and implementing a standardised and individualised nursing care plan in PC for patients with osteoarthritis, adapted to the features of each centre or district.57–59
This plan should include integral and individualised assessment of the patient to obtain the relevant clinical information about their physical, mental, social aspects and their environment in an organised manner. This will enable the situation to be analysed and ensure personalised and empathetic nursing care.57–60
After the integral assessment of the osteoarthritis patient, the patient and their family/carers should received education adapted to their needs and features (activities that cause greater joint overload, life-style, etc.). Similarly the patient will be taught and advised about the process of their disease so that they become more involved in the treatment plan and the outcomes of surgery, if indicated, can be improved.61–63 The aim of educating the patient, among others, is to treat the anxiety and/or despair associated with chronic pain.64
Given all the above, a specific nursing care plan can be designed (special care for multi-pathology patients, with cognitive problems, low WOMAC score, lacking family support, etc.).
Recommendations for patients with osteoarthritis of the knee considered candidates for total knee arthroplastyR10. The patient should be informed about their disease and the treatment plan proposed for them, including surgery (LoE 1b; GR A; GA 97%)Providing patients with information about their diseases, the available treatment and involving them in treatment decisions is their right under the General Health Act (art. 10.5), in the Law on the Autonomy of Patients and Rights and Obligations with regard to Clinical Information and Documentation (Law 41/2002 of 14 November) and in the Code of Medical Ethics and Deontology (art. 11.1).
In addition to being a right, information improves adherence to treatment,65 reduces the anxiety associated with surgery62 and increases patients’ satisfaction with the intervention.66,67 If the information supplied has an educational component not only does it reduce anxiety, it also improves the postoperative indicators such as pain and function and adverse events diminish. This is particularly important in patients with unrealistic expectations as to outcome, or who have a history of anxiety or depression.62
All of this information should always be clear, objective, realistic and adapted to the features, circumstances and needs of the patient. Similarly the patient should be informed of the consequences of not undergoing surgery and the possibilities of recovery and rehabilitation.46
R11. A rehabilitation and exercise programme should be started prior to surgery (LoE 1a; GR A; GA 85%)With arthroplasty of the knee, there is currently some controversy as to the efficacy of preoperative intervention such as physical exercise. This is due in part to the heterogeneity and variability of the interventions published. There is no evidence to support the systematic implementation of these interventions in obtaining better postoperative outcomes. It has been observed in a systematic review68 that preoperative exercises improve postoperative results short term (at least) in arthroplasty of the hip, but not the knee.
Furthermore, it has been demonstrated that poor presurgical functional status is strongly associated with greater postoperative pain after knee arthroplasty,6 and less pain and better function beforehand predict better outcomes in terms of pain and function after knee arthroscopy.69 Therefore, acting prior to surgery on these factors with exercises or other physical measures might potentially improve the outcomes of arthroplasty.
In addition, the clinical practice guidelines for the management of knee osteoarthritis recommend that education and exercise programmes should be used to improve functional status and pain.70 Patients who are waiting for operations are the ideal candidates for these types of programmes.
R12. It is recommended that pain should be treated aggressively in patients presenting moderate or intense pain levels preoperatively (LoE 1a; GR A; GA 92%)Patients undergoing knee arthroplasty presenting with more preoperative pain69,71–74 or greater functional limitation75 tend to achieve greater benefits from the intervention.6 Given that there are safe and effective treatment alternatives for controlling symptoms, treating pain can have a positive effect on the outcome of the operation. If the treatment chosen is effective, it should be prolonged up until surgery, since it can help to control postoperative pain.76
The use of topical or oral non-steroidal anti-inflammatory drugs (NSAIDs) is recommended in this group of patients, since they are of proven efficacy in the management of osteoarthritis symptoms. Selective cyclooxigenase 2 (COX-2) inhibitors have a better gastrointestinal safety profile than traditional NSAIDs and a cardiovascular safety profile similar to that of ibuprofene and diclofenac.77 Furthermore, their low effect on platelet aggregation means that they can be used up until the day of operation.78 The use of intra-articular infiltration with corticosteroids in patients who do not respond to NSAIDs is also recommended.79,80
When other alternatives have failed, the use of the major opioids is recommended.81 The role of drugs such as glucosamine, chondroitin sulphate or intra-articular hyaluronic acid in these patients is very limited and recent guidelines do not recommend them.79,3,82 The safety/efficacy balance of paracetamol83 and tramadol84 means that their role in this group of patient is under discussion.81 It is likely that multimodal analgesia, with various drugs at the same time, is the most effective option.
Recommendations for the peri-surgical period in patients with osteoarthritis of the knee undergoing total knee arthroscopyR13. Specific hosting protocols for admission to hospital should be implemented to prevent medical errors, improve the outcomes of surgery and ensure the necessary care (LoE 4; GR C; GA 95%)Once an arthroplasty has been indicated the patient might become more anxious as the date of their surgery approaches and this might affect the desired outcomes. In order to reduce this anxiety there should be hosting protocols or guidelines specific to each hospital. These should explain in detail all the stages that the patient will undergo from entering the admission ward up until their discharge, including those that generate the most anxiety, such as everything to do with their operation and the pain that they might experience.
These guidelines should include the patient safety protocols, such as checklists,85 marking the limb to be operated to reduce the risk of surgery to the wrong side,86 identification of comorbidities, protocols to detect and avoid medication errors and other procedures,87,88 protocols for recording and detecting adverse events, prevention of ulcers, falls and protocols for reducing anxiety,89,90 etc. These guidelines should be explained to the patient as important elements for their safety; this will also increase their trust and satisfaction with the process, and will improve the final outcomes.
R14. A multi-disciplinary fast track protocol for rapid postoperative recovery should be implemented (LoE 1c; GR A; GA 94%)Implementing fast-track programmes helps to reduce hospital stay without increasing postoperative complications, reduce the costs of the process and increase patient satisfaction.11,91–93 There are indirect data (lower opioid consumption) that suggest that, at least in the short term, these programmes can also have a beneficial effect on pain control.
There is great variability in the characteristics of fast-track programmes. Most include (in addition to everything to do with the surgery) presurgical actions such as patient education, pre-operative analgesia and prompt rehabilitation (after surgery).
Therefore, multidisciplinary collaboration is recommended for drafting standardised protocols and clinical guidelines for pre, peri and post-operative care, patient education programmes, the optimisation of surgical approach routes, fast rehabilitation with early mobilisation and optimal pain management and criteria for discharge and follow up.94–96
R15. The joint and the patient should be mobilised and specific rehabilitation started promptly after surgery (NE 2a; GR B; GA 90%)Early joint mobilisation after total knee arthroplasty involves continuous passive/assisted motion (CPM) started within the first 24h after surgery with the aim of reducing the risk of subsequent complications.
Although continuous passive motion is a widespread recommendation due to its potential physiological affect on haemarthrosis, peri-articular oedema and prevention of joint stiffness, the evidence on its effectiveness is limited.97,98 CPM has demonstrated no differences in articular range compared to standard treatments at one year after surgery.97,98 However, a slightly better range of joint mobility in the early postoperative period has been detected.99–101 Furthermore, inflammation recovery (interpreted as a reduction in joint perimeter) is slightly delayed when CPM is used.102,103 The results are contradictory or insufficient, if not non-existent, regarding pain,102,104 length of hospital stay,101,105,106 quality of life,99,107 knee functionality and patient satisfaction when attempting to demonstrate that it offers advantages over standard treatment. Therefore quality studies are required on each of the variables mentioned.97,98
Despite all the above, the use of CPM is warranted if the patient's healthcare centre is in possession of this resource and/or poor adherence to the rehabilitation protocol is predicted.
R16. A discharge report should be created to include detailed information of the intervention, assessment of the patient's pain level and functional capacity and the recommended treatment (LoE 5; GR D; GA 98%)The discharge report should contain, in addition to the essential data specified in the basic minimum data set (BMDS), data regarding the surgery (including the prosthesis model and manufacturer) and the peri-operative period. The post-operative outcomes should be included with a description of the examination on discharge, the patient's degree of pain and mobility. It is also essential that the discharge report should include a detailed description of the treatment plan and follow-up recommended for the patient.
Recommendations for the post-operative period for patients undergoing total knee arthroplastyR17. Any signs or symptoms that the prosthesis is not progressing well should be strictly monitored, with special emphasis on the early detection of infection (LoE 5; GR D; GA 94%)During this monitoring, it is vitally important that the surgical wound is checked. If there is erythema, swelling, dehiscence or exudation, a series of precautions should be taken, such as slowing down the rehabilitation process, local treatment and taking samples for culture, which if positive might involve antibiotic treatment. Furthermore, persistent joint pain (especially if at rest and/or nocturnal), joint effusion, difficulty in gaining mobility and fever can also be indicative of infection of the prosthesis (however, isolated increased local temperature, is constant in knees with prostheses).
If joint effusion appears, or if normal postoperative effusion does not reduce progressively or is accompanied by one of the abovementioned symptoms, this might indicate arthrocentesis.108 The appearance of turbid fluid means that monitoring should be increased, but purulent liquid might not mean infection, but an adverse reaction to the prosthetic parts (although this usually occurs later, not so much in the acute phase). The differential diagnosis of this will be confirmed by appropriate analysis and culture of intra-articular fluid.
The patient should not be treated empirically with oral antibiotics if acute infection is suspected. The infection should be proven or there should be very high clinical suspicion before such treatment.
R18. An early evaluation should be undertaken of the signs and symptoms of localised neuropathic pain (LoE 5; GR D; GA 90%)Postoperative localised neuropathic pain due to injury to the peripheral nervous system is a poor prognostic factor for pain, disability and quality of life for these patients. It is very important, if the preventive strategy has failed, to establish an early diagnosis of the condition and start anti-hyperalgesic treatment and prevent the pain from persisting.109
There are many questionnaires specifically for assessing neuropathic pain (LANSS, Pain DETECT, DN4, NPQ), with sensitivity ranging from 67% to 85% and specificity from 74% to 90%.110
R19. A coordinated multi-disciplinary follow-up plan should be put in place adapted to the patient's needs and characteristics (LoE 5; GR D; GA 90%)The process of knee arthroplasty does not end after discharge from hospital. The recovery period will take several months and therefore clear and concise instructions on the steps to follow and the warning signs and symptoms to monitor should be given. In each case and at all stages, there should be an awareness of the natural evolution of the process and the approaches to treatment. The orthopaedic surgeon is most involved at this point, they should indicate the guidelines to follow and design an individualised treatment plan, both pharmacological and non-pharmacological, which also includes the functional objectives Other professionals such as the rehabilitation physician, physiotherapist, nurse and family practitioner play a very important role in this process.
The patient should be given written information on their follow-up with a schedule of the periodic checks to be made, explaining the points to assess at each scheduled check, from monitoring the wound in the first appointments and its progress, to the radiological and functional evaluation at the six-monthly and/or annual checks, according to each team's protocol.111–114
R20. Rehabilitation should be adjusted to the patient's characteristics and the available resources (LoE 1a; GR A; GA 94%)The advantage of early rehabilitation after knee arthroplasty has been demonstrated. It improves function and pain, reduces post-operative complications and hospital stay.94,115,116
A multi-disciplinary approach to the intervention is important. This enables us to establish an action protocol without losing the possibility of approaching it in an individualised manner, according to the patient's personal characteristics.117
The method of delivering these programmes should adapt to the patient, and the organisational system of each health area, and the available resources (supervised home-care programme118 or as an outpatient in the hospital or physiotherapy support units within the health centres). Information and communication techniques (ICT) can also be used to help in implementing and developing care programmes.119
DiscussionThe patient with knee osteoarthritis to such an extent that their doctors believe that they will, sooner or later, require placement of a knee prosthesis faces a complex process which often, but not always,120 ends in the recovery of function of the affected limb. This document sets some basic recommendations, on which there is clear consensus that might facilitate this process. First, the process must start with a complete assessment of the patient to include not only the physical aspects of the disease but also identify whether their pain has become chronic and assess various psychopathological parameters. The patient should be placed at the centre of the entire process. They should be kept informed to the highest degree possible but, above all, they must understand that they are an essential participant in treatment decisions. It is vital to define the process explicitly, establish a complete diagnostic and treatment scheme for these patients to include the recommendations of the various clinical guidelines, and the specific roles of each healthcare tier in the care of these patients to prevent duplications and gaps in care. Finally, it is essential to understand that knee replacement surgery for osteoarthritis is a complex procedure which, in order to succeed, requires attention to detail and a multi-disciplinary approach before, during and after the procedure.
Society faces a major health problem in the treatment of patients with knee osteoarthritis. Given that the currently available treatments are merely symptomatic, the number of knee arthroplasties are projected to increase almost exponentially.121 However, knee arthroplasty has limitations in meeting the needs of our patients, and the rate of dissatisfaction with the procedure ranges from 20% to 30%.120,122 In a prior consensus undertaken by GEDOS-SECOT factors were identified where intervention could take place to improve the outcomes of arthroplasty.81 However, this consensus was restricted to the immediate preoperative period. It is worth considering, therefore, that a more thorough and extensive study of the process that starts at the moment surgery is first suggested until one year after the operation might help to improve the quality of care and outcomes.
This poses a considerable challenge, since it is a process that should be approached multi-laterally, across all the healthcare tiers, including managers, specialists, PC physicians and nursing staff. Ensuring that these professionals, who often have very different problems, concerns and needs, collaborate and arrive at common objectives is extremely difficult. The object of this consensus, driven by GEDOS-SECOT, is to attempt to find common points between these professionals in approaching a highly prevalent problem which causes high morbidity, namely osteoarthritis of the knee.
The Delphi methodology was used to achieve common points of consensus between these professionals. This strategy is based on a panel of experts123 and was initially developed as a systematic and interactive communication method. The methodology has some intrinsic limitations: the quality level of the evidence shown is, ultimately, grade 5: expert recommendations. In this case we tried to control this limitation as far as possible by 3 systematic reviews and reviews of the most recent publications in the literature,79,80 which enabled us to present many of the recommendations with the highest levels of evidence: five of the recommendations are grade 1, two grade 2 and five grade 4, leaving only nine with a grade 5. Furthermore it is intrinsic to the Delphi system to produce “expert recommendations” where there is no other evidence of higher quality. Despite these limitations, this methodology has been chosen by various scientific societies as a suitable tool to establish therapeutic recommendations124–126 and create lines of opinion on controversial clinical matters.127
A grade of agreement of at least 70% was achieved for the 20 recommendations proposed by the steering group (a universally accepted limit for this type of methodology).128 This shows that, despite the diversity of origins and interests of the writers, the recommendations made were received with great interest by all the professionals and very high levels of consensus were established. It can be claimed that this high level of consensus is due to the fact that the recommendations presented should simply be “common sense”. However, the effort of the authors should not be undervalued; they managed to summarise this “common sense” (the least common of the senses) in a series of easy-to-read recommendations of rapid access and well documented.
Care process for the candidate for knee arthroplastyThere was a clear consensus among the panel members for the need to formally establish this process (recommendations 1 and 5 and 9). The undeniable fact is acknowledged that the success of the process does not lie in isolated action on the part of the “operator” on the day of surgery, but there are very many opportunities, from long before the operation, to improve the results of the surgical procedure. The agreement of various physicians is necessary for this (PC physicians, rehabilitation and orthopaedic specialists, etc.), as well as that of the nursing staff. This key role for nurses must be explicitly recognised, since it has a grade 2 level of evidence. Moreover, there is some evidence (grade 4) that all the practitioners involved should attempt to work in a coordinated manner to obtain the best outcomes. The consensus also established recommendations with a level of evidence 5 on the need to appoint a formal multidisciplinary team leader, to define a referral protocol between the various practitioners and to faithfully follow the recommendations in the various clinical practice guidelines on the therapeutic management of these patients. To conclude, the need is also highlighted for periodic assessments of the protocol and the patients included, also with a level of evidence of 5, in order to increase quality.
Role of the patient in the process of knee arthroplastyIf there is a key tendency in current medicine it is to attempt to place the patient at the centre of all care processes, and this is clear in recommendations 4 and 10. There was a clear consensus of the need to provide the patient with precise and complete information on their diagnostic and treatment process (level of evidence grade 1a). Furthermore, it was agreed that the patient should be involved and made co-responsible for their decision-making plan, and that there should be periodic assessment of adherence to this plan and its effectiveness. This was considered advisable but with a lower level of evidence (grade 4).
Assessment of the candidate for knee arthroplastyThere was clear consensus among the participants in underlining the importance of complete and integral assessment of the patient who is to undergo this process (recommendations 1 to 3). The need for complete initial assessment of the patient was established at a level of evidence grade 5, and at a grade 4 level of evidence it was established that this assessment should not be limited to the purely mechanical joint part or physical health, but should also include an assessment of key parameters. Firstly, it is recommended that central sensitisation to pain should be assessed, and the mechanism for the chronification of pain, which, if present, is associated with poor outcomes.129 Secondly, it is also recommended that the patient should be assessed for psychopathology and catastrophising, both factors are also associated with poor results.
Surgical procedure for knee joint replacementA total of 10 recommendations (from 11 to 20) focus on the time around the surgical procedure, which is of course the key element of the entire process. With a level of evidence grade 1, three recommendations were established: starting an exercise and rehabilitation programme before the intervention, adjusting the entire rehabilitation process realistically to the patient's needs and the available resources, and that pain should be treated aggressively before surgery (this recommendation was already established in the consensus document of 2014).81 With a high level of evidence (grade 1c) a recommendation was established on the progressive implementation of fast track protocols in centres, since they have demonstrated efficacy in controlling costs, maintaining safety and improving patient satisfaction. The importance of early rehabilitation after surgery is shown in the grade 2a recommendation. A recommendation with a level of evidence grade 4 establishes the need for a specific hosting protocol when the patient arrives at the centre where the surgery is to take place.
Finally, four recommendations with a level of evidence 5 focus on the postoperative phase that starts on discharge of the patient. A complete discharge report is necessary and clear guidelines on the next steps that the patient should follow. On discharge a schedule of multidisciplinary visits should be arranged to enable postoperative recovery and strict monitoring for any signs or symptoms that the prosthesis is not progressing correctly, with special emphasis on the early detection of infection and timely identification of signs and symptoms of localised neuropathic pain.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that neither human nor animal testing have been carried out under this research.
Confidentiality of dataThe authors declare that no patients’ data appear in this article.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
FundingThe preparation of this document was financed by Grünenthal Pharma S.A.
Conflict of interestThe authors have no conflict of interest to declare.
Miguel Almaraz Guntín, Jesús Betegón Nicolás, M. del Pino Calderín Morales, Ernesto Candau Pérez, Ion Carrera, Vicente J. Casa de Pantoja, Roberto Colomer Garrido, Daniel Comesaña Bastero, Carlos Debán Miguel, Ricardo de Felipe Medina, David de la Rosa Ruiz, Miguel Ángel Esparza Pagán, Rubén Estella Nonay, Ernesto Franco Peris, Miguel Ángel Froufe, Luis Gallego, Antonio Jesús Garbayo Marturet, David García Aguilera, Juan Carlos García de la Blanca, Pablo García Parra, Vicente Giner Ruiz, Fernando González del Castillo Campos, Francisco Javier Gordillo López, Carlos E. Hernández Guerrero, Fernando León Vázquez, Tomás Llinares Galiana, José M. Lomo Garrote, Juan Luis López Alcázar, Aránzazu López Villalvilla, Iago Martínez Melián Xavier Mas Garriga, María Medina Abellán, Jorge Merlo Arroyo, Damián Mifsut Miedes, Ramón Navarro Ortiz, Enrique Nieto Pol, Francisco Pedro Ortiz Carrellán, Blanca Palomino Aguado, Marta Pérez Lescure, Rubén Pérez-Mañanes, Álvaro Pérez Martin, Agustín Pina Medina, Eduard Ribas i Forcadell, Luis Javier Roca Ruiz, Germán Rodríguez Rosales, Javier Romero Fernández, Eduardo Salvador González, Miguel Sánchez Prieto, María Santos, Clarisa Simón Pérez, Mariano Soler Albert, Alberto Touza, Francisco Vargas Negrín.
Please cite this article as: Ruiz Iban MA, Tejedor A, Gil Garay E, Revenga C, Hermosa JC, Montfort J, et al. Consenso GEDOS-SECOT sobre el proceso de atención a pacientes con artrosis de rodilla e indicación de artroplastia. Rev Esp Cir Ortop Traumatol. 2017;61:296–312.