The main objective of this study is to analyse the one-year mortality in patients with intracapsular hip fracture who were admitted during severe social confinement in the first months of the COVID-19 lockdown and compare it with previous years.
Material and methodsRetrospective observational study in which a cohort from March 14 to June 21, 2020 (pandemic group, n=62) was compared with a control cohort on the same dates in the years 2017, 2018 and 2019 (control group, n=172). Thirty-day-mortality and one-year-mortality, orthopaedic complications, ASA grade, comorbidities, diagnosis and treatment, time to surgery and mean stay were measured.
ResultsNo significant differences were found in 30-day mortality (p=0.156; 9.7% compared to 4.7%) or in one-year mortality (p=0.47) between the pandemic group (21%) and the control one (16.9%). A decrease in surgical delay and mean stay was observed in the pandemic group, although without statistical significance.
ConclusionThe State of Alarm modified the distribution of the type of hip fracture with a predominance of intracapsular fracture. Maintaining the same hospital management as prior to the pandemic period made it possible not to increase 30-day mortality and one-year mortality in patients with intracapsular hip fracture.
El objetivo principal de este estudio es analizar la mortalidad al año en los pacientes con fractura intracapsular de cadera que ingresaron durante un severo confinamiento social en los primeros meses de la pandemia por COVID-19 y compararla con la mortalidad en los años previos.
Material y métodoEstudio observacional retrospectivo en el que se comparó una cohorte del 14 marzo al 21 de junio de 2020 (grupo pandemia, n=62) con una cohorte control en las mismas fechas de los años 2017, 2018 y 2019 (grupo control, n=172). Se midieron la mortalidad a los 30días y al año, las complicaciones ortopédicas, el grado ASA, las comorbilidades, el diagnóstico y el tratamiento, el tiempo hasta cirugía y la estancia hospitalaria.
ResultadosNo se encontraron diferencias significativas en la mortalidad a los 30días (p=0,156; 9,7% vs. 4,7%) ni en la mortalidad anual (p=0,47) entre el grupo pandemia (21%) y el grupo control (16,9%). Se objetivó un descenso de la demora quirúrgica y de la estancia media en el grupo pandemia, aunque sin significación estadística.
ConclusiónEl estado de alarma modificó la distribución del tipo de fractura de cadera, con un predominio de la fractura intracapsular. El hecho de mantener el mismo manejo hospitalario que el previo a la pandemia permitió no incrementar la mortalidad a los 30días y al año en los pacientes con fractura intracapsular de cadera.
On 11 March 2020, the World Health Organisation (WHO) declared coronavirus disease 2019 (COVID-19) a pandemic. In Spain, the first case was diagnosed on 31 January1 and a State of Emergency was declared on 14 March, which remained in force until 21 June.2 Until that time, the total number of cases in Galicia was 9174, making it the eighth autonomous community in terms of cumulative number of COVID-19 positives,3 with a cumulative incidence of 340 cases per 100,000 inhabitants.
Hip fracture represents one of the main emergencies in Orthopaedic Surgery and Traumatology (OTS) and a delay in surgery of more than 48h is associated with increased mortality.4 In addition, it has been associated with a high risk of COVID-19 infection during admission, and with a higher mortality rate if infected with COVID-19.5 Indeed, patients with hip fractures have been considered a vulnerable group during the pandemic because of their age and the comorbidities that are often associated with them.6 However, it is not entirely clear whether or not there was a reduction in the incidence of these fractures as a consequence of home confinement. Several authors in Spain reported a reduction of between 26% and 30% in admissions for hip fracture,7 however, other authors found no significant differences.8,9
The mortality rate per year of this pathology is approximately 30%10 and 7% at 30 days after surgery.11 In hip fracture patients with COVID-19 infection, the 30-day mortality rate is high, between 30% and 35%,12–14 and according to Wignall et al.15 it is 38.2%. A recent systematic review found a significant increase in 30-day mortality in COVID+ or suspected COVID patients, with an Odds ratio=6.09 (95% CI=4.75–8.59).16 However, when comparing mortality between the pandemic period versus pre-pandemic periods, a recent meta-analysis found no difference in the 30-day mortality rate.17
The primary objective of this study was to analyse mortality per year in patients admitted for hip fracture in our centre during lockdown in Spain, with severe social confinement and to compare it with mortality per year in the same periods in 2017, 2018 and 2019. The secondary objectives were to analyse mortality in the first 30 days, average length of stay and surgical delay during the lockdown period compared to previous years.
We hypothesised in our study that, given the social and mobility restrictions and the overload of hospital activity, the one-year mortality of hip fracture would have been increased.
Material and methodDesignA retrospective observational study was conducted on a prospective database, comparing two cohorts. The first cohort (pandemic group) included intracapsular hip fractures occurring in a pandemic scenario of social confinement, during the first three months of social confinement (14 March to 21 June 2020, the lockdown period). It was compared with a control group, which included intracapsular hip fractures from the same period in 2019, 2018 and 2017. The study was conducted at the Hospital Álvaro Cunqueiro (Vigo), a tertiary referral centre in southern Galicia, Spain. The findings were reported according to the ‘STrengthening the Reporting of OBservational studies in Epidemiology (STROBE)’ guidelines for retrospective cohort studies.18
Inclusion criteria- 1.
Patients treated in our hospital with intracapsular hip fracture.
- 2.
Patients with a closed hip fracture.
- 3.
Patients aged 65 years or older at the time of fracture.
For comparability of outcomes, t was decided to include only intracapsular fractures in the study, since during the pandemic period, in our centre. They represented 92.5% of the total fractures, while they accounted for 51.5% of the fractures in the control group.
Variables and tools of measurementThe primary variable studied was one-year mortality. As secondary variables, 30-day mortality was measured, as well as rates of orthopaedic complications: infection, dislocation, osteosynthesis failures and peri-implant or periprosthetic fractures.
The following data were collected for all patients: baseline and demographic characteristics (age, gender, laterality), American Society of Anesthesiologists (ASA) classification, preoperative factors such as Charlson Comorbidity Index (CCI), comorbidities, fracture type and therapeutic management, surgical delay measured in hours (difference between the time and date of surgery and the time and date of admission) and hospital stay measured in days (difference between the date of discharge and the date of admission).
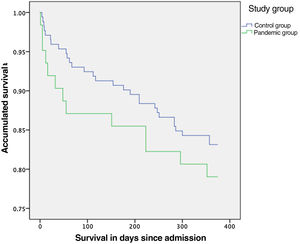
Statistical analysisA descriptive analysis of the variables was carried out with frequencies (percentages) and measures of central tendency (mean, median, 95% confidence intervals and interquartile range). The Kolmogorov–Smirnov test was used to analyse the normality of the distribution of the variables. X2 and Student's t-test were performed for comparison of normally distributed variables, while the Wilcoxon signed-rank test was used to compare median surgical delay times. The Kaplan–Meier method was used to analyse survival, both overall and specific, and the log-rank test was used to compare survival. Cox regression was used to analyse factors associated with mortality and expressed as hazard ratios (HR) with their 95% CIs. Data were analysed with SPSS 24.0 software and the accepted level of significance for all hypothesis tests was considered to be .05.
Ethical aspectsAll data were obtained from the patients’ electronic medical records. The data were recorded from the database of the National Hip Fracture Registry (RNFC), to which our hospital is attached and whose collection protocol has been approved by the Research Ethics Committee of our institution (CAAV/2016/22 – 2020/322). The researchers respected the fundamental principles of the Declaration of Helsinki and the Council of Europe Convention on Human Rights and Biomedicine, as well as all current legislation related to the study.
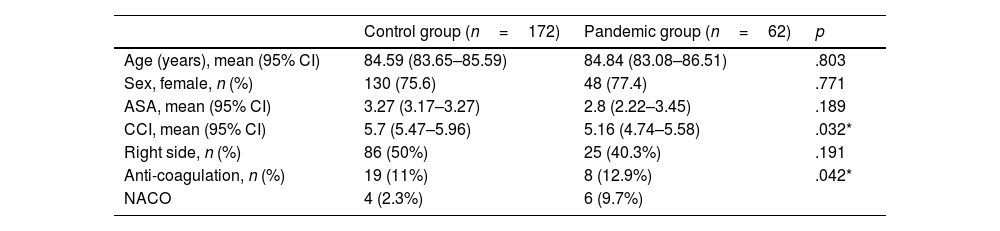
ResultsDemographyA total of 234 patients with intracapsular hip fracture were analysed: 62 patients in the pandemic group (admitted from 14 March to 21 June 2020) and 172 patients in the control group (admitted on the same dates in 2017, 2018 and 2019). There were no statistically significant differences between the two groups with respect to mean age, ASA grade or sex (Table 1). Statistical significance was found (p=.032) when comparing the ICC between the pandemic group (5.16) and the control group (5.7); as well as in the use of anticoagulants (p=.042), being higher in the pandemic group (12.9% taking acenocoumarol and 9.7% taking new oral anticoagulants [NOAC]) than in the control group (11.3% acenocoumarol, 2.3% NOAC).
Clinical baseline and sociodemographic characteristics.
| Control group (n=172) | Pandemic group (n=62) | p | |
|---|---|---|---|
| Age (years), mean (95% CI) | 84.59 (83.65–85.59) | 84.84 (83.08–86.51) | .803 |
| Sex, female, n (%) | 130 (75.6) | 48 (77.4) | .771 |
| ASA, mean (95% CI) | 3.27 (3.17–3.27) | 2.8 (2.22–3.45) | .189 |
| CCI, mean (95% CI) | 5.7 (5.47–5.96) | 5.16 (4.74–5.58) | .032* |
| Right side, n (%) | 86 (50%) | 25 (40.3%) | .191 |
| Anti-coagulation, n (%) | 19 (11%) | 8 (12.9%) | .042* |
| NACO | 4 (2.3%) | 6 (9.7%) |
CCI: Charlson comorbidity index; 95% CI: 95% confidence Interval; NACO: new anticoagulants.
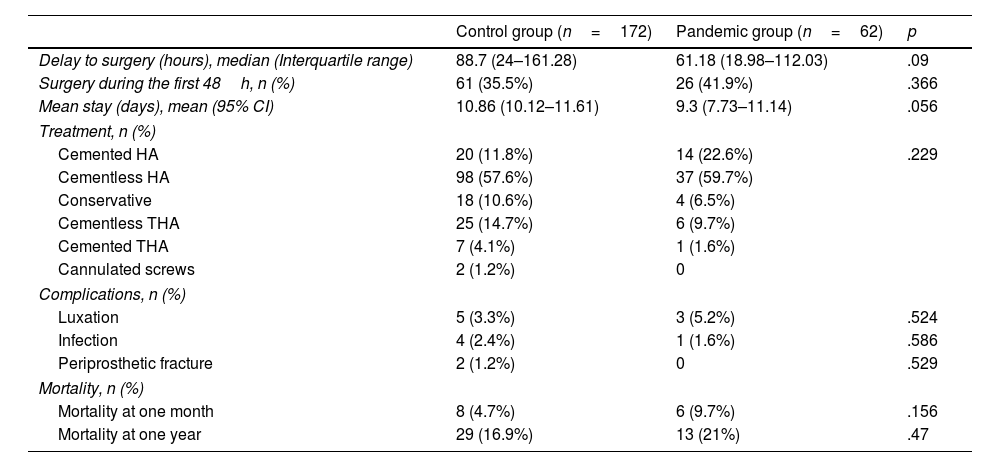
The most commonly used implant in both groups was the cementless hemiarthroplasty: 59.7% in the pandemic group and 57.6% in the control group (Table 2). With regard to time to surgery, in the control group 35.5% of patients underwent surgery before the first 48h, while in the pandemic group 41.9% of patients with hip fracture underwent surgery within the first 48h, without finding statistically significant differences (p=.366). Nor were differences found in the data for surgical delay (p=.09) and mean hospital stay (p=.056), although in both cases they were lower in the pandemic group, as can be seen in Table 2.
Surgical aspects, complications and mortality.
| Control group (n=172) | Pandemic group (n=62) | p | |
|---|---|---|---|
| Delay to surgery (hours), median (Interquartile range) | 88.7 (24–161.28) | 61.18 (18.98–112.03) | .09 |
| Surgery during the first 48h, n (%) | 61 (35.5%) | 26 (41.9%) | .366 |
| Mean stay (days), mean (95% CI) | 10.86 (10.12–11.61) | 9.3 (7.73–11.14) | .056 |
| Treatment, n (%) | |||
| Cemented HA | 20 (11.8%) | 14 (22.6%) | .229 |
| Cementless HA | 98 (57.6%) | 37 (59.7%) | |
| Conservative | 18 (10.6%) | 4 (6.5%) | |
| Cementless THA | 25 (14.7%) | 6 (9.7%) | |
| Cemented THA | 7 (4.1%) | 1 (1.6%) | |
| Cannulated screws | 2 (1.2%) | 0 | |
| Complications, n (%) | |||
| Luxation | 5 (3.3%) | 3 (5.2%) | .524 |
| Infection | 4 (2.4%) | 1 (1.6%) | .586 |
| Periprosthetic fracture | 2 (1.2%) | 0 | .529 |
| Mortality, n (%) | |||
| Mortality at one month | 8 (4.7%) | 6 (9.7%) | .156 |
| Mortality at one year | 29 (16.9%) | 13 (21%) | .47 |
95% CI: 95% confidence interval; HA: hemiarthroplasty; THA: total hip arthroplasty.
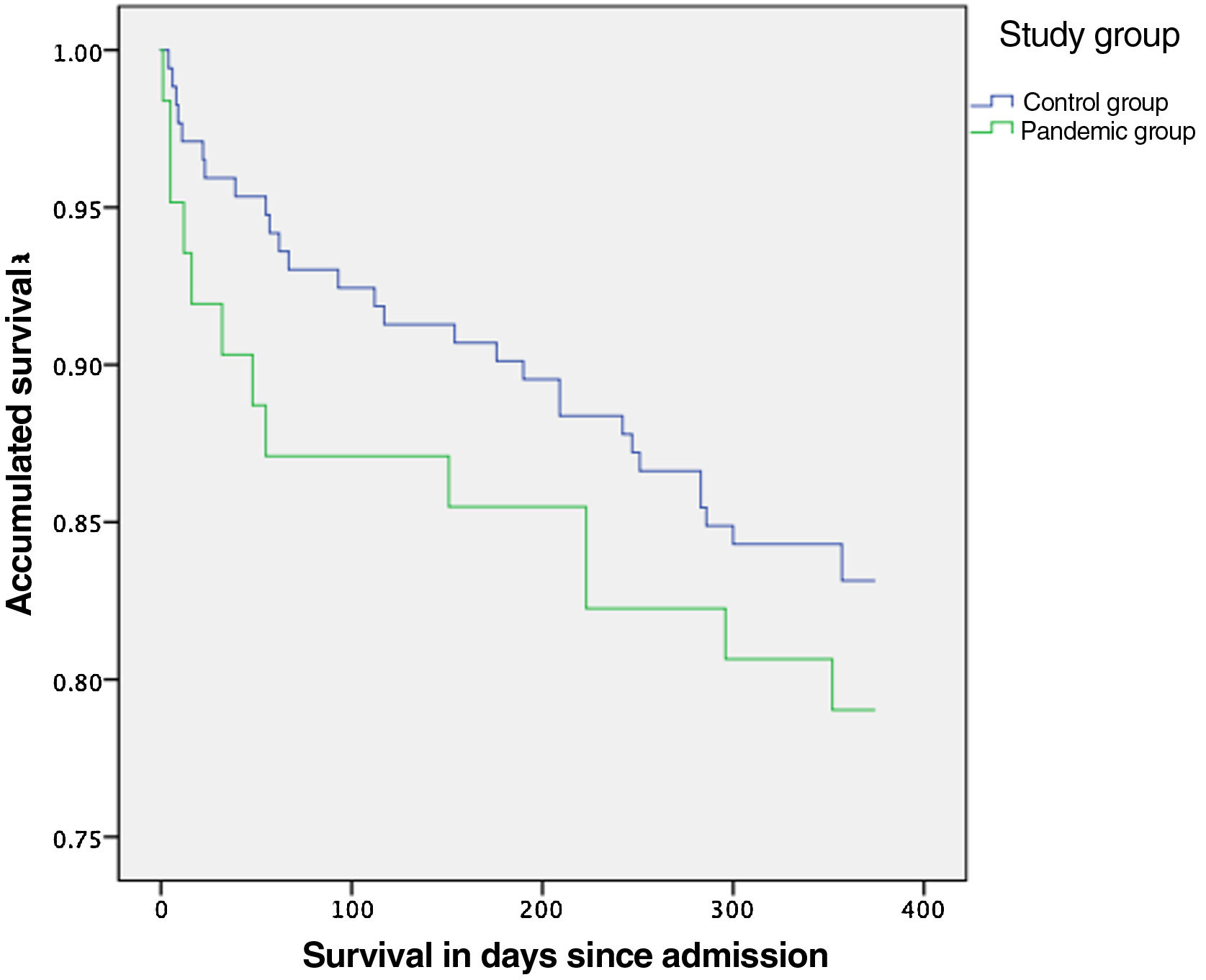
No statistically significant differences were found when comparing dislocation, infection and periprosthetic fracture rates (Table 2). The annual mortality rate in the pandemic group was 21%. This mortality rate was 16.9% in the control group, with no statistically significant difference (p=.47) between the two. There was also no significant difference in the risk of mortality during the first year (HR=.77 [95% CI: .39–1.47]; p=.425) between the two groups (Fig. 1). Mortality at 30 days was 9.7% in the pandemic group and 4.7% in the control group (p=.156).
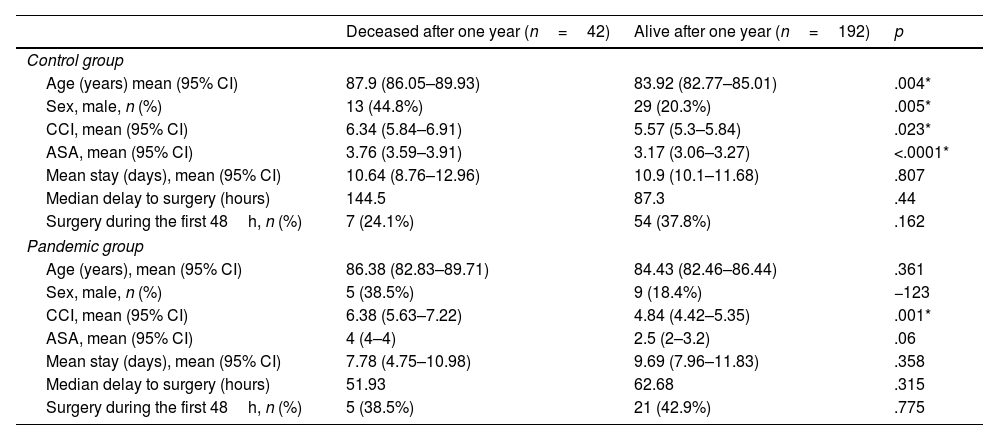
With regard to mortality, and analysing each of the groups separately, it was observed that, in the control group, those who died during the first year also had a higher CCI (p=.023), greater age (p=0.004), a greater degree of ASA classification (p<.0001) and there was a greater proportion of males (p=.005) than in the group of patients alive at one year, as can be seen in Table 3. In the pandemic group, statistically significant differences were only found in the CCI between the deceased group and those alive at one year after the fracture (p=.001) (Table 3).
Comparison in both study groups between the deceased patients during the first year and those who remained alive one year after the fracture.
| Deceased after one year (n=42) | Alive after one year (n=192) | p | |
|---|---|---|---|
| Control group | |||
| Age (years) mean (95% CI) | 87.9 (86.05–89.93) | 83.92 (82.77–85.01) | .004* |
| Sex, male, n (%) | 13 (44.8%) | 29 (20.3%) | .005* |
| CCI, mean (95% CI) | 6.34 (5.84–6.91) | 5.57 (5.3–5.84) | .023* |
| ASA, mean (95% CI) | 3.76 (3.59–3.91) | 3.17 (3.06–3.27) | <.0001* |
| Mean stay (days), mean (95% CI) | 10.64 (8.76–12.96) | 10.9 (10.1–11.68) | .807 |
| Median delay to surgery (hours) | 144.5 | 87.3 | .44 |
| Surgery during the first 48h, n (%) | 7 (24.1%) | 54 (37.8%) | .162 |
| Pandemic group | |||
| Age (years), mean (95% CI) | 86.38 (82.83–89.71) | 84.43 (82.46–86.44) | .361 |
| Sex, male, n (%) | 5 (38.5%) | 9 (18.4%) | −123 |
| CCI, mean (95% CI) | 6.38 (5.63–7.22) | 4.84 (4.42–5.35) | .001* |
| ASA, mean (95% CI) | 4 (4–4) | 2.5 (2–3.2) | .06 |
| Mean stay (days), mean (95% CI) | 7.78 (4.75–10.98) | 9.69 (7.96–11.83) | .358 |
| Median delay to surgery (hours) | 51.93 | 62.68 | .315 |
| Surgery during the first 48h, n (%) | 5 (38.5%) | 21 (42.9%) | .775 |
95% CI: 95% confidence interval; CCI: Charlson comorbidity index.
A total of six patients in the pandemic group (9.7%) were tested after the diagnosis of hip fracture. Of the two patients in this group who died during the first year, one case tested positive and the other negative. In the remaining four patients, three patients tested negative (75%) and only one patient tested positive (25%).
DiscussionThe main finding of our study is that there was no statistically significant difference (p=.47) between the one-year mortality of intracapsular hip fractures occurring in a pandemic setting (21%) compared to the annual mortality of fractures in the previous three years (16.9%). We have found no other studies analysing the annual mortality of hip fractures occurring in a pandemic period. On the other hand, the overall mortality per year in patients who suffer a hip fracture varies, depending on the study to which we refer, between 15% and 36%,19 being three to four times higher than that expected in the general population.20
Social confinement, which began in Spain on 14 March 2021 by virtue of the proclamation of the State of Emergency, prohibited any non-essential activity, reducing trips out of the home to a minimum. In fact, until 2 May, people over 70 were not allowed to leave their homes for recreational activities, clearly limiting patients’ mobility and capacity for rehabilitation. However, these limitations have not translated into increased mortality at one year, despite the fact that lack of mobilisation of hip fracture patients has been postulated as an independent risk factor for both in-hospital and long-term mortality.21,22
A recent Spanish study evaluated epidemiological variations in fracture occurrence during the period of confinement,8 Although they described a drastic decrease in the total number of fractures, they noted that there was no difference in the number of osteoporotic hip fractures requiring surgical treatment.
The orthogeriatric unit remained in operation in our centre throughout the pandemic period. Integrated orthogeriatric care has been related to a reduction in mortality in patients with hip fracture, in the average length of stay, surgical delay and post-surgical length of stay, thus being related to significant financial savings and an improvement in the quality of care and resulting in a more effective and efficient model of care.23
With regard to 30-day mortality, we also found no differences between the two groups (9.7% in the pandemic group, 4.7% in the rest of the fractures; p=.156), a finding consistent with previous studies.15,24–26. Tripathy et al.,17 in a recent meta-analysis, also found no statistically significant differences in 30-day mortality between the pandemic and pre-pandemic periods in patients with hip fracture.
Although the median surgical delay from admission during the pandemic period was lower (Table 2), no significant differences were found, nor were there significant differences in the percentage of hip fractures operated on in the first 48h, which was 41.9% during confinement and 35.5% in previous years. The maintenance of the fast-track hip fracture protocol in our centre made it possible to avoid delays in time to surgery during pandemic times. Delaying hip fracture surgery beyond the first 24h after admission is associated with increased 30-day mortality.11 The hip fracture protocol involves accelerating the preoperative study from the Emergency Department, allowing the patient to be in an optimal surgical situation in the first 48h, with the collaboration of the Anaesthesiology and Resuscitation and Orthogeriatrics departments.23 Greensmith et al.24 also found no difference in the time from admission to surgery, however Wignall et al.15 did detect a significant increase in surgical delay during confinement (43.7h) compared to previous times (34.6h on average), just as Segarra et al.27 also found an increase in surgical delay during the pandemic (from 1.5 days to 1.8 days). On the other hand, the low incidence of COVID-19 in our area, the maintenance of the fast track hip and the reorganisation of the limited surgical resources available at that time towards urgency, allowed our centre to maintain the surgical delay times prior to the pandemic or even reduce them, although without reaching statistical significance, increasing in turn the percentage of fractures operated on in the first 48h. Hall et al.14 reported that 65% of their patients studied during confinement were operated on within the first 36h, while in the period prior to confinement 70% of surgeries were performed within 36h of admission, without finding statistically significant differences.
With respect to the mean length of stay of the patients, in our case, during confinement, we found that it was shorter (9.3 days), but no significant differences were obtained with respect to the mean length of stay prior to confinement (10.86 days). This differs from previous studies where significant differences were found.8 Hall et al.14 found a significantly shorter mean stay during confinement (7.8 days vs. 11.3 days), similar to Greensmith et al.24 (6.5 vs. 12 days) and Wignall et al.15 (15 vs. 16.6 days). However, in a recent meta-analysis that analysed more than 1500 patients with hip fractures, no differences were found, as in our study, in the mean length of stay.17
Despite the overload on the health system, we understand that, contrary to our initial hypothesis, the fact of having maintained the protocols in health care for hip fracture and comprehensive orthogeriatric care, despite the overload on the health system, meant that the usual surgical delay times and the average length of stay did not increase. This has meant that there has been no increase in mortality in the first 30 days or one year after intracapsular hip fracture.
Our study has the inherent limitations of being an observational study. One of its main limitations is that patients with pertrochanteric or subtrochanteric fractures were not included in the final analysis, due to the absolute dominance we found in intracapsular fractures in the pandemic period. Analysing hip fracture from a general perspective, the latest RNFC published in Spain in the year 2019, showed a prevalence of pertrochanteric fractures (51.8%) over intracapsular fractures (38.2%).28 This substantial increase in intracapsular fractures found in our study during the pandemic period may be due to the effects of the absolute social confinement experienced during the months of March to May. Intracapsular fractures, compared to extracapsular fractures, have been related to low-energy falls or even to the absence of trauma29 and, moreover, it has recently been seen that hip fractures during the first months of the pandemic were largely the result of stumbling inside the home, rather than slips and falls outside the home.30 In other words, falls were typically low-energy.
Analyses for COVID-19 infection were scarcely performed, as during the period studied (March–May 2020) there was no protocol with standardised PCR testing for all admitted patients in our centre, and this test was only performed in cases with clear symptoms of COVID-19 disease. It should also be noted that this is a study conducted in an area with a low relative incidence in terms of number of cases and admissions for COVID-19, so the results may not be comparable with those of other studies conducted in areas with a high incidence.
Our study strengths are that it was the first study to analyse mortality per year in patients with hip fracture in a pandemic environment and restriction of mobility. Also, it was undertaken in the largest hospital in the main city of Galicia, which at the time of the study presented the same restrictions as the rest of Spain, as it was a lockdown situation. In addition, thanks to the global nature of the electronic medical record system for all health centres in the region, we had access to data on all health care to assess comorbidities and events studied, allowing total and global traceability of all patients included in the study.
ConclusionLockdown changed the distribution of hip fracture type with a predominance of intracapsular fracture. Maintaining the same hospital management as before the pandemic did not increase 30-day and 1-year mortality in patients with intracapsular hip fractures.
Level of evidenceLevel of evidence III.
FundingNone of the study participants received any funding of any kind.
Conflict of interestsThe authors certify that they have no business associations (e.g. consultancies, stock ownership, shareholdings, patent/licensing agreements, etc.) that may pose a conflict of interest in relation to this article.