Compare 30-day mortality rate following a proximal femur fracture (PFF) and SARS-CoV-2 infection versus a PFF and no SARS-CoV-2 infection.
DesignRetrospective comparative study.
SettingThree university hospitals in Biscay province (Basque Country, Spain). Patients: 77 patients over 65 years-old with PFF (AO 31-A and 31-B).
InterventionStudy conducted between 9 March and 15 April 2020. The COVID-19 group included only patients with SARS-CoV-2 infection, confirmed by a positive RT-PCR test.
Main outcome measurements30-day mortality rate and risk factors for mortality.
ResultsOf a total 77 patients, 10 were diagnosed with SARS CoV-2 infection. Mean age was 85 years. Patients with SARS-Cov-2 infection had higher BMI (29.53kg/m2) compared to patients without infection (24.09kg/m2) (p=0.001). No significant differences were found between both groups in terms of the Charlson Comorbidity Index, ASA score, use of oral anticoagulants or presence of cognitive impairment. Seven of the 10 patients in the COVID-19 group developed (viral) pneumonia, as compared to one single case (1/67) of (bacterial) pneumonia in the control group (p<0.001). Thirty-days mortality was higher (p=0.03) in COVID-19 patients (40%) than in those in the control group (11.9%). In the multivariate analysis, age ≥91 years-old, ASA class IV and BMI >25kg/m2 were significant predictors of 30-day mortality. All deaths in the COVID-19 group occurred while the patients were hospitalized.
ConclusionsSARS CoV-2 infection in patients with a PFF was seen to result in higher rates of early mortality, with COVID-19-related pneumonia being the leading direct cause of mortality.
Comparar la tasa de mortalidad a 30 días en los pacientes con fractura de fémur proximal (FFP) y coinfección por SARS-CoV-2 frente a FFP sin coinfección.
DiseñoEstudio retrospectivo comparativo.
EscenarioTres hospitales universitarios en Vizcaya (País Vasco, España).
PacientesSetenta y siete pacientes mayores de 65 años con FFP (AO 31-A y 31-B).
IntervenciónEntre el 9 de marzo y el 15 de abril de 2020. El grupo COVID-19 incluía pacientes con infección confirmada mediante el test PCR-RT.
Medidas de resultados principalesTasa de mortalidad a 30 días y factores de riesgo de mortalidad.
ResultadosDiez de los 77 pacientes presentaron coinfección por SARS-CoV-2. La edad media fue de 85 años. Los pacientes infectados presentaban un IMC mayor (29,53kg/m2) frente a los no infectados (24,09kg/m2) (p=0,001). No hubo diferencias significativas en el índice de comorbilidad de Charlson, la puntuación ASA, el uso de anticoagulantes o el deterioro cognitivo. Siete pacientes del grupo COVID-19 (7/10) desarrollaron neumonía (vírica), frente a un solo caso (1/67) de neumonía (bacteriana) en el grupo control (p<0,001). La mortalidad a 30 días fue mayor (p=0,03) en los pacientes con COVID-19 (40%) que en el grupo control (11,9%). La edad ≥91 años, la clase IV ASA y el IMC>25kg/m2 fueron predictores significativos de mortalidad a 30 días. Todas las muertes en el grupo COVID-19 ocurrieron intrahospitalariamente.
ConclusionesLa infección por SARS-CoV-2 en pacientes con PFF resultó en tasas más altas de mortalidad temprana, siendo la neumonía por COVID-19 la principal causa directa de mortalidad.
Nivel de evidencia: Estudio nivel III
From December 2019 a series of individuals in the Chinese province of Hubei were diagnosed with pneumonia secondary to a new viral disease that was given the name COVID-19.1 The causative agent was a new virus that came to be known as SARS-CoV-2. The first case of the disease in Spain was identified on 31 January 2020, and the first case in the Biscay province (Basque Country) was diagnosed on 3 March.2 Spain quickly became one of the most severely hit countries by the pandemic with 173,633 positive cases at 15 April and a mortality rate around 10%.2 In order to curb the progression of the disease, Spanish authorities declared a state of emergency as of 14 March.3 With over 100 cases per 100,000 inhabitants, Biscay province was declared a high-risk area. At 15 April, 6442 cases had tested positive for COVID-19.4
Since the first few COVID-19 cases were diagnosed, proximal femur fractures (PFF) in the elderly have become a prevalent condition prompting the development of several specific clinical guidelines.5,6 During the worst phase of the pandemic in China, 87% of fractures resulted from falls from a standing height in individuals with a mean age of 76 years; and 72.7% of patients sustained their fractures at home. Of the 453 fractures analyzed by these authors, 264 (53.8%) were fractures of the hip joint.7 Patients with a PFF may develop pulmonary infections as a result of the functional limitations they experience.8,9 Potential bronchoaspiration events and the stress associated with fractures and their treatment may result in excessive oxidative and inflammatory reactions, which typically stimulate the expression of different proinflammatory factors and cause the patients’ immune system to weaken, increasing the risk of pulmonary infection.8–10 In this regard, pulmonary complications have been reported in as many as 4.9% of patients following surgical treatment for a hip fracture.8
Given the relative prevalence of PFFs during the COVID-19 pandemic, the advanced age at which such fractures are typically sustained, and the greater proneness shown by the elderly to complications resulting from COVID-19,11,12 a concomitant SARS-CoV-2 infection could plausibly increase morbimortality in patients with a PFF. One-year mortality following a hip fracture stands around 20%,13 while mortality during the first 30 days has been reported at 7%,14 and in-hospital mortality from 2.1%15 to 4.4%.14 The goal of the present study is to analyze 30-day mortality in patients with both hip fracture and SARS-CoV-2 infection, and compare the results with those of a control group made up of patients with hip fractures without SARS-CoV-2 infection treated over the same period of time. Secondary goals included an identification of the mortality risk of the studied population as well as an analysis of their ambulatory function and the complications observed at 30 days’ follow-up.
Material and methodsThis is a multicentre retrospective observational study conducted between 9 March and 15 April 2020 in patients older than 65 years of age with a PFF with a minimum post-fracture follow-up of 30 days. Fractures associated with multiple trauma and high-energy injuries, as well as pathological fractures secondary to tumour-mediated bone destruction and periprosthetic fractures, were all excluded. The study was carried out in the three highest-capacity hospitals of Biscay province: Cruces University Hospital (Barakaldo), Basurto University Hospital (Bilbao) and Galdakao-Usansolo University Hospital. The study was performed in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist for cohort, case-control and cross-sectional studies.16 Institutional Review Board approval was obtained, and written informed consent was obtained from all patients.
A record was made of the subjects’ demographic characteristics as well as their comorbidities. The Charlson comorbidity index17 was calculated for each patient and data on whether they were on anticoagulant agents or presented with a neuromuscular condition were collected. Anaesthetic risk was also assessed using the ASA Physical Status Classification. Ambulatory function prior to the fracture was evaluated based on 4 functional levels: unaided ambulation, ambulation with a cane, ambulation with two crutches or a walker, and inability to ambulate. The AO classification was used to categorize PFFs (31-A, 31-B).18 The study group included only patients with a diagnosis of SARS-CoV-2 infection, confirmed by a positive reverse transcription polymerase chain reaction (PCR-RT) test of the upper respiratory tract. Both probable COVID-19 cases (non-confirmed respiratory infections) and possible COVID-19 cases (no microbiological diagnosis) were excluded. The signs and manifestations associated with COVID-19 were recorded (cough, fever, chest pain, dyspnoea, fatigue, headache, dizziness, nasal congestion, abdominal pain, nausea, vomiting and anosmia) together with information about the initial symptom that appeared in each case and the treatment administered. The management of patients was similar in the 3 hospitals. Patients with SARS-CoV 2 infection were transferred to specific areas for infected patients, where they were treated not only by trauma surgeons but also by internists, pneumologists and other medical specialists dedicated to this work in order to improve medical care in these cases. Patients were treated with hydroxychloroquine in addition to oxygen therapy and corticosteroids depending on the needs due to respiratory failure. Details on the surgical delay, the operative time (h) and the treatment used to address the femoral fracture (total hip replacement, hemiarthroplasty or fracture fixation) were also complied.
Postoperative variables included transfusion requirements, time to weight-bearing, length of hospital stay and in-hospital mortality. A record was also made of ambulatory function, postoperative complications and 30-day mortality. Following Parvizi et al.,19 complications were classified into major and minor complications. Major systemic complications were the ones involving a vital risk and major local complications were those that caused some kind of functional disability or required an additional surgical procedure.
Statistical analysisAn exploratory data analysis of the recruited sample was performed: frequencies and percentages for categorical data, and means and standard deviations for continuous variables were computed. To assess the relationship between the sociodemographic and clinical variables with the study group (SARS-CoV-2 infection vs. no SARS-CoV-2 infection), the Wilcoxon non-parametric test and the Chi-square (and the Fisher's Exact test if necessary) approach were used.
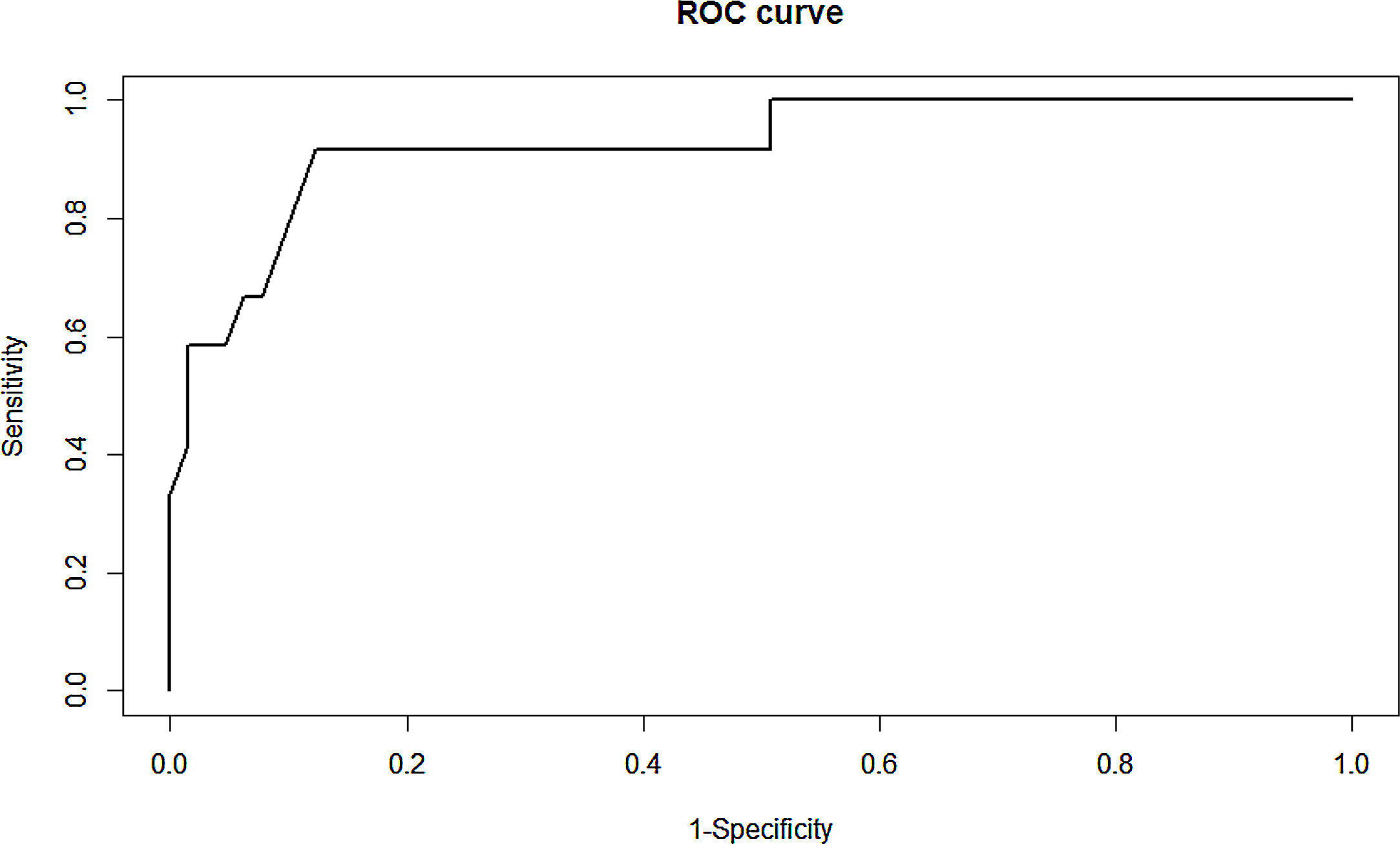
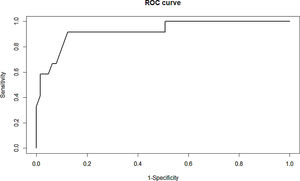
In order to determine the potential predictors for 30-day mortality, a univariate analysis was initially performed, using the Wilcoxon non-parametric and the Chi-square (the Fisher's Exact test if needed) tests. Those variables with a p-value <0.20 in the univariate procedure were entered in the multivariable logistic regression model process. Using the backward procedure, the final estimates were measured in terms of odds ratios (OR) with their confidence intervals. To assess the model robustness, the area under the ROC curve (AUC) (Fig. 1) was calculated (an AUC >0.7 is considered a good discrimination) and the Hosmer–Lemeshow test (a p-value ≥0.05 shows a good calibration) were applied. All the statistical procedures were conducted using the SAS System v9.4. A p-value <0.05 was deemed to be statistically significant.
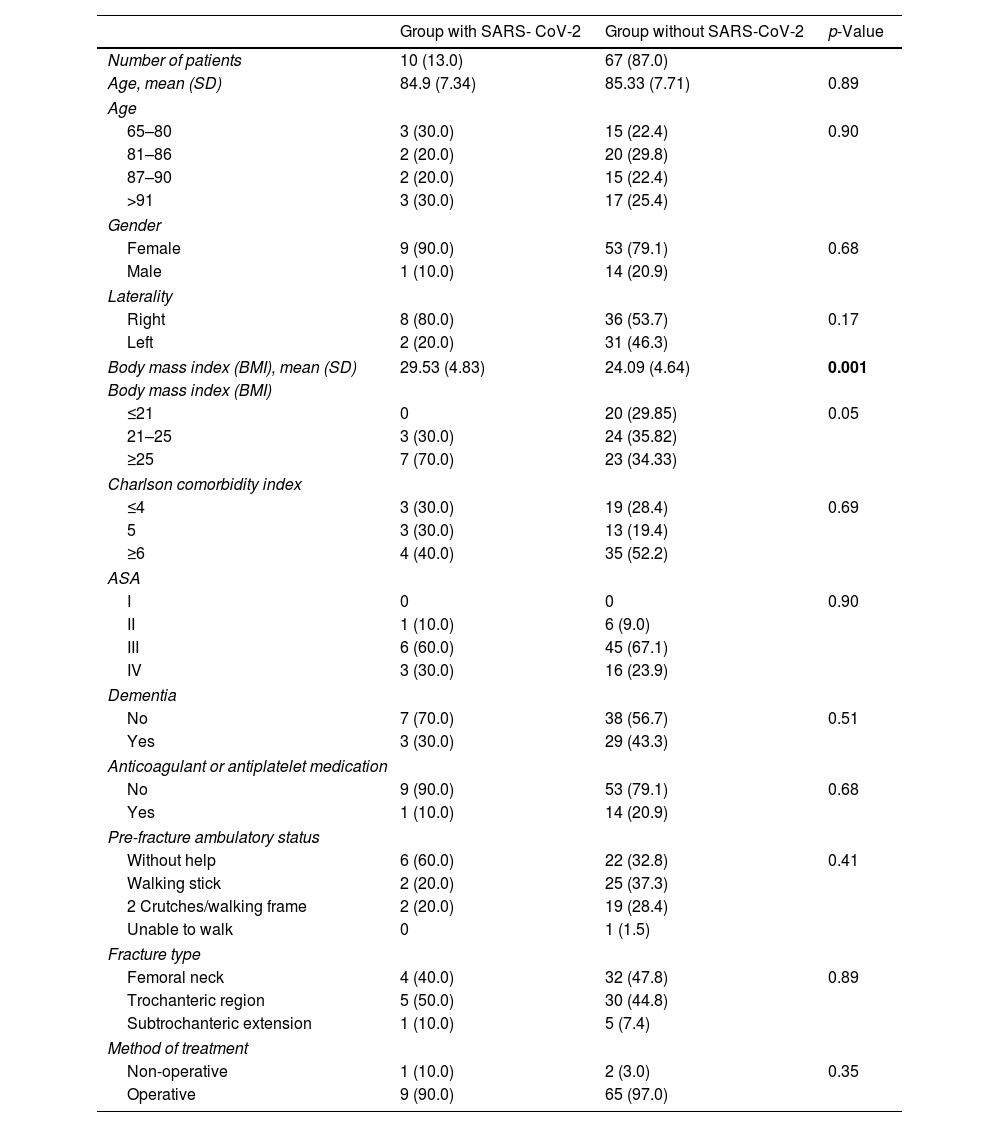
ResultsThe total number of subjects studied was 77, of whom 10 had a SARS-CoV-2 infection apart from a PFF. All of them were diagnosed within one week after sustaining the fracture, except for one patient who was diagnosed at the emergency room following the discovery of bilateral infiltrates on the chest radiograph performed. No patient presented with SARS-CoV-2 infection at the end of follow-up. Table 1 shows the demographic variables of patients with and without a SARS-CoV-2 infection. Sixty-two of the 77 patients were women (80.52%). The mean age of the sample was 85 years (range: 65–102 years). Demographic characteristics were evenly distributed in both the SARS-CoV-2 and the non-infected group. No significant differences were found between the groups in terms of age, sex, different comorbidities, Charlson score, ASA score, use of oral anticoagulants or presence of neuromuscular conditions. However, there was a clear difference between the groups regarding body mass index (BMI). Over 70% of patients in the SARS-CoV-2 group had a BMI of 25 or higher, while 65% of the patients in the non-infected group had a BMI lower than 25. Patients with SARS-CoV-2 infection had a mean BMI of 29.53kg/m2 compared to patients without infection (24.09kg/m2) (p=0.001). As regards pre-fracture ambulatory function, 71.4% of patients was able to ambulate either unaided or with the help of a cane or a crutch. A total of 27.3% could ambulate with two crutches or a walker and slightly over 1.3% were unable to walk at all. No significant differences were observed between the groups in this regard either.
Demographic variables of patients with and without a SARS CoV 2 infection.
| Group with SARS- CoV-2 | Group without SARS-CoV-2 | p-Value | |
|---|---|---|---|
| Number of patients | 10 (13.0) | 67 (87.0) | |
| Age, mean (SD) | 84.9 (7.34) | 85.33 (7.71) | 0.89 |
| Age | |||
| 65–80 | 3 (30.0) | 15 (22.4) | 0.90 |
| 81–86 | 2 (20.0) | 20 (29.8) | |
| 87–90 | 2 (20.0) | 15 (22.4) | |
| >91 | 3 (30.0) | 17 (25.4) | |
| Gender | |||
| Female | 9 (90.0) | 53 (79.1) | 0.68 |
| Male | 1 (10.0) | 14 (20.9) | |
| Laterality | |||
| Right | 8 (80.0) | 36 (53.7) | 0.17 |
| Left | 2 (20.0) | 31 (46.3) | |
| Body mass index (BMI), mean (SD) | 29.53 (4.83) | 24.09 (4.64) | 0.001 |
| Body mass index (BMI) | |||
| ≤21 | 0 | 20 (29.85) | 0.05 |
| 21–25 | 3 (30.0) | 24 (35.82) | |
| ≥25 | 7 (70.0) | 23 (34.33) | |
| Charlson comorbidity index | |||
| ≤4 | 3 (30.0) | 19 (28.4) | 0.69 |
| 5 | 3 (30.0) | 13 (19.4) | |
| ≥6 | 4 (40.0) | 35 (52.2) | |
| ASA | |||
| I | 0 | 0 | 0.90 |
| II | 1 (10.0) | 6 (9.0) | |
| III | 6 (60.0) | 45 (67.1) | |
| IV | 3 (30.0) | 16 (23.9) | |
| Dementia | |||
| No | 7 (70.0) | 38 (56.7) | 0.51 |
| Yes | 3 (30.0) | 29 (43.3) | |
| Anticoagulant or antiplatelet medication | |||
| No | 9 (90.0) | 53 (79.1) | 0.68 |
| Yes | 1 (10.0) | 14 (20.9) | |
| Pre-fracture ambulatory status | |||
| Without help | 6 (60.0) | 22 (32.8) | 0.41 |
| Walking stick | 2 (20.0) | 25 (37.3) | |
| 2 Crutches/walking frame | 2 (20.0) | 19 (28.4) | |
| Unable to walk | 0 | 1 (1.5) | |
| Fracture type | |||
| Femoral neck | 4 (40.0) | 32 (47.8) | 0.89 |
| Trochanteric region | 5 (50.0) | 30 (44.8) | |
| Subtrochanteric extension | 1 (10.0) | 5 (7.4) | |
| Method of treatment | |||
| Non-operative | 1 (10.0) | 2 (3.0) | 0.35 |
| Operative | 9 (90.0) | 65 (97.0) | |
Data are expressed as frequency and numbers in brackets are the percentages.
Thirty-six (46.8%) of the 77 fractures were femoral neck fractures (AO 31-B) and 41 (53.2%) intertrochanteric (AO 31-A), without any significant differences between infected and non-infected patients regarding the type of fracture sustained. Only 3 patients of the total sample did not undergo surgery on account of their poor prognosis: one had severe respiratory failure, another pulmonary thromboembolism, and the other one a brain stroke. Of the 74 patients treated surgically, 6 were implanted a total hip prosthesis and 28 a hemiarthroplasty; the other 40 were treated with internal fixation (1 with a dynamic hip screw [DHS], 31 with a short cephalomedullary nail, and 8 with a long cephalomedullary nail). All patients in the SARS-CoV-2 group underwent surgery, except for one individual who belonged to the terminally-ill group mentioned above. In 7 of the remaining 9 patients, the diagnosis was established postoperatively due to respiratory symptoms or fever >38°C. Mean time from fracture to COVID-19 diagnosis was 4 days. Mean time from fracture to surgery was 43h (SD 26) in the SARS-CoV-2 group and 44h (SD 26) in the COVID-19-free group, with no statistically significant differences between both groups. Surgery was performed under spinal anaesthesia in all suspected and confirmed SARS CoV-2 infection cases. The remaining patients were operated under either spinal anaesthesia (54 cases) or general anaesthesia (11 cases).
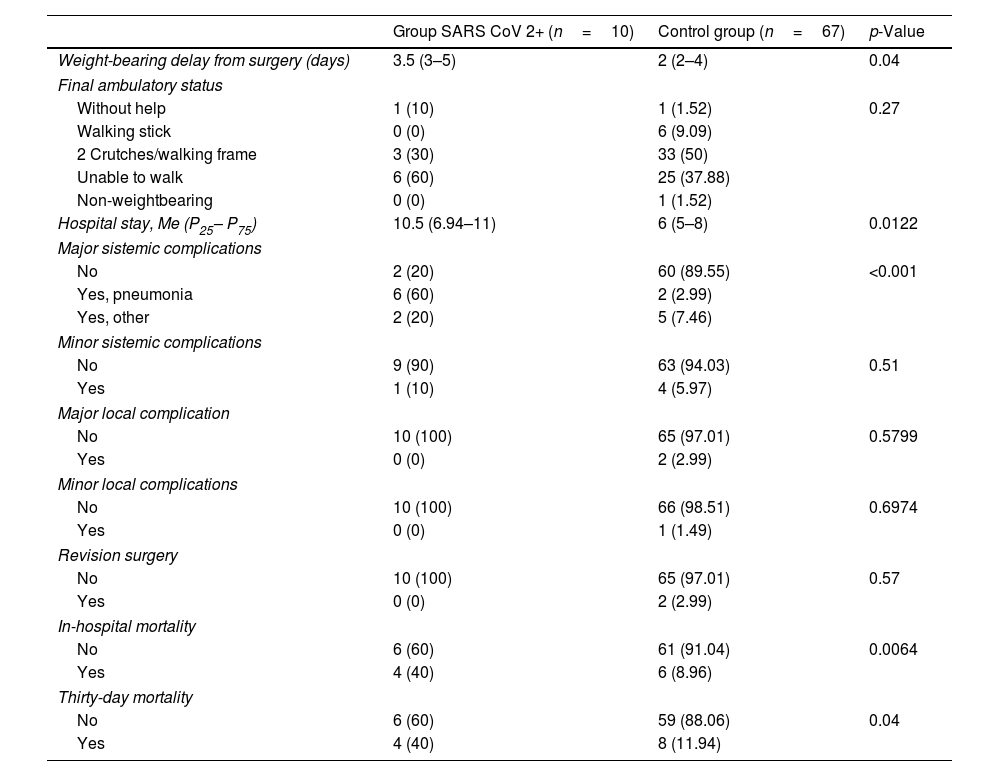
Table 2 shows outcomes of patients with and without a SARS CoV2 infection. No significant differences were observed between the two groups as regards major or minor local complications, or minor systemic complications. However, statistically significant differences were observed regarding major systemic complications. These included the presence of viral pneumonia in 7 of the 10 patients infected with SARS-CoV-2, as compared with a single case (1/67) of bacterial pneumonia in the infection-free group (p<0.001). Mean hospital stay was also significantly longer in the SARS-CoV-2 group than in the COVID-19-free group, with mean lengths of stay of 10 (SD 6) and 7 (SD 4) days respectively (p=0.0122). Two patients from the non-infected group required a revision surgery following failure of primary fracture fixation. Both cases were treated with a new open reduction and internal fixation (ORIF) procedure. At the end of follow-up, 40% of infected patients were able to ambulate (either independently or with the help of a walking aid) and the mean time to weight-bearing was 3.5 days (range, 3–5). In contrast, the percentage of non-infected patients who were able to ambulate was 60%, with a mean time to weight-bearing of 2 days (range, 2–4). However, differences were not statistically significant. We found no statistical differences in post-fracture short-term ambulatory status as a function of the method of treatment (arthroplasty vs. fixation).
Clinical features of patients with and without a SARS CoV 2 infection.
| Group SARS CoV 2+ (n=10) | Control group (n=67) | p-Value | |
|---|---|---|---|
| Weight-bearing delay from surgery (days) | 3.5 (3–5) | 2 (2–4) | 0.04 |
| Final ambulatory status | |||
| Without help | 1 (10) | 1 (1.52) | 0.27 |
| Walking stick | 0 (0) | 6 (9.09) | |
| 2 Crutches/walking frame | 3 (30) | 33 (50) | |
| Unable to walk | 6 (60) | 25 (37.88) | |
| Non-weightbearing | 0 (0) | 1 (1.52) | |
| Hospital stay, Me (P25– P75) | 10.5 (6.94–11) | 6 (5–8) | 0.0122 |
| Major sistemic complications | |||
| No | 2 (20) | 60 (89.55) | <0.001 |
| Yes, pneumonia | 6 (60) | 2 (2.99) | |
| Yes, other | 2 (20) | 5 (7.46) | |
| Minor sistemic complications | |||
| No | 9 (90) | 63 (94.03) | 0.51 |
| Yes | 1 (10) | 4 (5.97) | |
| Major local complication | |||
| No | 10 (100) | 65 (97.01) | 0.5799 |
| Yes | 0 (0) | 2 (2.99) | |
| Minor local complications | |||
| No | 10 (100) | 66 (98.51) | 0.6974 |
| Yes | 0 (0) | 1 (1.49) | |
| Revision surgery | |||
| No | 10 (100) | 65 (97.01) | 0.57 |
| Yes | 0 (0) | 2 (2.99) | |
| In-hospital mortality | |||
| No | 6 (60) | 61 (91.04) | 0.0064 |
| Yes | 4 (40) | 6 (8.96) | |
| Thirty-day mortality | |||
| No | 6 (60) | 59 (88.06) | 0.04 |
| Yes | 4 (40) | 8 (11.94) | |
Data are presented as frequency and column percentages in brackets.
Me (P25 – P75): Median (25th and 75th percentile).
Thirty-day mortality was significantly higher among infected patients (40%) than among non-infected ones (11.9%) (p=0.04). In-hospital mortality showed a similar pattern, with all deaths in the COVID-19 patient group occurring while patients were hospitalized as compared with 9% of in-hospital deaths in the non-infected group. Three of four deaths in the COVID group occurred in the first 7 days. No deaths occurred in the COVID-19 group between discharge and the end of follow-up, while 2 non-infected patients died over that period. Mortality among patients not undergoing surgery was 67% (2 of 3). Other risk factors of thirty-day mortality were also analyzed. There was no significant difference with regard to surgical delay (<24h vs. >24h) or the method of treatment (arthroplasty vs. fixation).
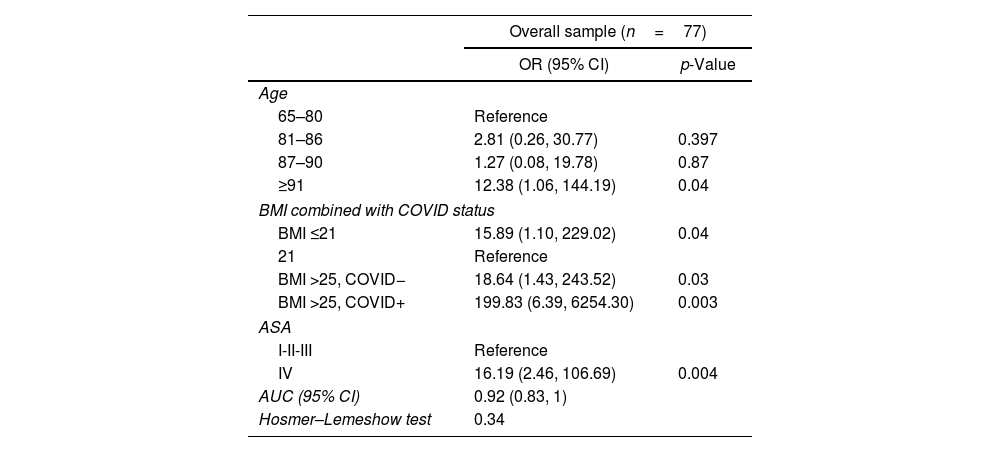
In the multivariate analysis (Table 3), patient factors were assessed for association with 30-day mortality. Among all patient variables, age ≥91 years-old (odds ratio 12.38; 95% confidence interval, 1.06–144.19, p=0.04) and ASA class IV (odds ratio 16.19; 95% confidence interval, 2.46–106.69, p=0.004) were also independently associated with mortality. BMI >25kg/m2 was a significant predictor of 30-day mortality and more precisely combined with SARS-CoV-2 positive status (odds ratio 199.83; 95% confidence interval, 6.39–6254.30, p=0.003); that is, patients with a BMI higher than 25 and being SARS-CoV-2 positive were more likely to die within 30 days compared with patients with a normal BMI.
Multivariate analysis with odds ratios demonstrating the increased risk for 30-day mortality.
| Overall sample (n=77) | ||
|---|---|---|
| OR (95% CI) | p-Value | |
| Age | ||
| 65–80 | Reference | |
| 81–86 | 2.81 (0.26, 30.77) | 0.397 |
| 87–90 | 1.27 (0.08, 19.78) | 0.87 |
| ≥91 | 12.38 (1.06, 144.19) | 0.04 |
| BMI combined with COVID status | ||
| BMI ≤21 | 15.89 (1.10, 229.02) | 0.04 |
| 21 | Reference | |
| BMI >25, COVID− | 18.64 (1.43, 243.52) | 0.03 |
| BMI >25, COVID+ | 199.83 (6.39, 6254.30) | 0.003 |
| ASA | ||
| I-II-III | Reference | |
| IV | 16.19 (2.46, 106.69) | 0.004 |
| AUC (95% CI) | 0.92 (0.83, 1) | |
| Hosmer–Lemeshow test | 0.34 | |
OR (95%ci): Odds ratio with their confidence interval at 95th confidence level.
AUC (95% CI): Area under the ROC curve with confidence interval at 95th confidence level.
BMI: Body Mass Index.
COVID-19 is a new pandemic that has spread rapidly throughout Spain, where the first case was reported on 31 January 2020. Biscay province (Basque Country), with a population of 1,152,000 inhabitants, had its first case sometime later (on 3 March 2020). Since then, the number of infected cases in the province significantly increased reaching 6442 confirmed cases and 467 deaths on 15 April 2020.4 The present study was conducted in the 3 university hospitals of Biscay province, which have an overall capacity of 1910 beds. The pandemic radically transformed the routine of the departments of orthopaedic and trauma surgery in the three hospitals involved and forced the progressive cancellation of all elective procedures from 16 March. From that date onwards, orthopaedic surgery was reserved for patients sustaining traumatic injuries or those with malignant tumours or severe complications, such as infections. Patients with hip fractures were individually examined in conjunction with the Department of Anaesthesiology, and an independent circuit was established for those with a confirmed or suspected SARS-CoV-2 infection. Although at the time of writing this report all patients scheduled for surgery are subjected to an RT-PCR test, in the course of the study period RT-PCR tests were reserved for patients presenting with symptoms suggestive of COVID-19 (cough, fever or dyspnoea). According to the therapeutic algorithm developed by the British Orthopaedic Association for the management of orthopaedic patients during the COVID-19 pandemic, the care of patients suffering from lower limb fragility fractures should be considered urgent and a surgical priority.20 In our series, mean time from hip fracture to surgery was similar in the SARS-CoV-2 and the infection-free group.
Use of regional anaesthesia is recommended during surgery in order to avoid manipulation of the airway, which could cause cough during intubation and extubation.21 Not manipulating the airway prevents direct contact with the aerosolized agent and the dispersion of viral particles. Sixty-three patients of the total sample were operated using spinal anaesthesia (including two cases of suspected SARS CoV-2 infection and all confirmed COVID-19 cases). Eleven patients were operated with general anaesthesia (patients on platelet antiaggregants or oral anticoagulants operated before the effect of the drugs had time to wear off), and 3 patients did not undergo surgery. Use of personal protective equipment (PPE) is imperative when contacting infected patients, both for diagnosis and treatment.6,8
Pneumonia is one of the most devastating systemic complications experienced by patients sustaining a fracture of the hip joint.8 Pneumonia has serious implications for patients with a hip fracture, being associated with an 8-fold increase in the readmission rate, an 8-fold increase in the risk of sepsis, and a 3-fold increase in mortality.8 Lv et al., studied 1429 geriatric patients with hip fractures and reported a 4.9% indicence of postoperative pneumonia. The mortality rate was higher in patients with pneumonia.10 Eight of the 77 patients in our study developed pneumonia (10.4%). Seven of those patients belonged to the SARS-CoV-2 group and only one belonged to the (COVID-19-free) control group (1.5%). This patient developed a bacterial pneumonia. Catellani et al. recently published the results of a study of 16 patients with interstitial pneumonia secondary to SARS-CoV-2 infection and a PFF.22 Three patients died of respiratory failure and 13 patients underwent surgery. Twelve of the 13 operated patients showed an improvement of their ventilatory and oxygen saturation parameters, which could denote a benefit of surgical treatment. Nonetheless, 4 of those patients died within 7 days of surgery. It seems that, as reported by Catellani et al.,22 after the first 7–10 days post-op COVID-19 patients tend to exhibit an improvement in their respiratory function, which reduces their mortality rate. In our study, 3 of 4 deaths in the COVID-19 group occurred in the first 7 days.
A recent study by the Spanish Hip Fracture Register (RNFC) reported an in-hospital mortality rate of 4.4%, and a 30-day mortality rate of 7.6%.14 In a multicentre study conducted in Spain, Muñoz Vives et al. found a short-term mortality rate of 30.4% (7 out of 23 patients) in patients with a hip fracture and SARS CoV-2 infection, as compared with 5.3% (6 out of 113) for patients who either tested negative or were not tested due to a lack of symptoms.23 In 12 of the 136 patients in that study, the fracture was treated conservatively, with a mortality rate of 67%. According to the epidemiological analysis carried out by the Basque Country since the beginning of the epidemic, mortality among infected patients from 80 to 89 years of age has been found to be 23.7%.24 The present study found a high 30-day mortality rate in patients with confirmed SARS-CoV-2 infection (40%). In other words, the mortality found in the association between SARS-CoV-2 infection and PFF, seems to increase not only the mortality rate with respect to isolated PFF, but also the mortality rate in infected patients with absence of PFF. This poor prognosis in patients with both, PFF and SARS-CoV-2 infection, can be attributed to a combination of factors rather than purely attributed to a single factor. Lim and cols. postulate that coagulopathy in SARS-CoV-2 infection associated with lack of physical activity and reduced mobility in hip fractures predispose to a higher risk of thromboembolic complications. Furthermore, injuries and associated surgical procedures required in these patients can cause inflammation and subsequent release of inflammatory cytokines which potentiate COVID-19 induced inflammation, likely leading to a storm of cytokines that can result in an acute respiratory distress syndrome (ARDS) and multiple organ dysfunction (e.g. acute liver injury, acute kidney injury), which are possible causes of inpatient mortality.25
In our study, thirty-day mortality in patients with confirmed SARS-CoV-2 infection (40%), was significantly higher (p<0.05) than in the infection-free group (12%). SARS-CoV-2 patients who developed pneumonia exhibited a mortality rate of 57% (4 in every 7). Mortality among patients not undergoing surgery was 67% (2 in every 3).
Surgical delay from admission greater than 24h has been related to an increased risk of complications, including risk of 30-day mortality.26 However, in the present study there was no significant difference with regard to surgical delay (<24h vs. >24h). In our study, no significant differences were seen in terms of surgical delay between both groups, with a mean delay of 43h in the infected group and 44h in the infection-free group. Despite the lack of habitual resources (operating theatres, anaesthetists, nurses, etc.) and the absence of clearly established new circuits at the beginning of the pandemic, this surgical delay is considerably lower than the general delay observed in Spain according to a recent study (64.6h) 14.
The present study suffers from several limitations. Firstly, there are limitations associated with the retrospective nature of the analysis. Also, the sample size is small, which makes it difficult to generalize the findings obtained. Moreover, a 30-day-follow-up might underestimate the actual overall mortality in the studied cohort. On the other hand, the strength of the study lies in the fact that it is representative of an area that is home to over one million inhabitants, with a high prevalence of COVID-19 over the period studied. It will be necessary to carry out larger-scale analyses of larger patient cohorts to determine the way in which SARS-CoV-2 infection affects patients with a PFF and establish a proper perioperative algorithm capable of reducing short-term mortality.
ConclusionThe present study found a much higher 30-day in-hospital mortality rate in patients with both a PFF and SARS-CoV-2 infection than in infection-free patients with a PFF. Pneumonia was the main direct cause of mortality in patients infected with SARS CoV-2. In the multivariate analysis, age ≥91 years-old and ASA class IV were also independently associated with mortality. BMI >25kg/m2 was a significant predictor of 30-day mortality in patients with SARS-CoV-2 positive status.
Level of evidenceLevel III study.
Conflicts of interestDr Jimenez-Telleria declares no conflicts of interest.
Dr Urra declares no conflicts of interest.
Dr Fernandez-Gutierrez declares no conflicts of interest.
Dr Aragon declares no conflicts of interest.
Mr Aguirre declares no conflicts of interest.
Dr Foruria declares no conflicts of interest.
Dr. Moreta serves as a paid consultant to MBA Surgical Empowerment, JRI Orthopaedics and Ethicon (Johnson and Johnson).
The authors thank Pablo Roza Miguel and the MBA Institute for their assistance.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.