The poor results obtained in young patients when using a conventional prosthesis led to the resurgence of hip resurfacing to find less invasive implants for the bone. Young patients present a demand for additional activity, which makes them a serious challenge for the survival of implants. In addition, new information technologies contribute decisively to the preference for non-cemented prostheses. Maintaining quality of life, preserving the bone and soft tissues, as well as achieving a very stable implant, are the goals of every hip orthopaedic surgeon for these patients. The results in research point to the use of smaller prostheses, which use the metaphyseal zone more and less the diaphyseal zone, and hence the large number of the abovementioned short stem prostheses. Both models are principally indicated in the young adult. Their revision should be a more simple operation, but this is only true for hip resurfacing, not for short stems.
Los malos resultados obtenidos en pacientes jóvenes cuando se utiliza una prótesis convencional fueron la causa que motivó el resurgir de las prótesis de superficie, en un intento de buscar implantes menos invasivos para el hueso. Los pacientes jóvenes presentan una demanda de actividad adicional, lo cual los convierte en un serio reto para la supervivencia de los implantes. Además, las nuevas tecnologías de la información contribuyen de forma determinante a la preferencia de prótesis no cementadas. Mantener la calidad de vida, preservar el hueso y las partes blandas, así como conseguir un implante muy estable, son los objetivos que todo cirujano ortopédico de cadera persigue para este tipo de pacientes. Los resultados en investigación apuntan hacia el uso de prótesis de menor tamaño, que utilicen más la zona metafisaria y menos la diafisaria, dando lugar al extenso capítulo de las mencionadas prótesis de vástago corto. Ambos modelos tienen su principal indicación en el adulto joven. Su revisión debería ser una cirugía más sencilla pero este hecho solo se cumple para las prótesis de superficie, no así para los vástagos cortos.
It may seem appropriate to talk about surface prostheses (SP) and short-stem prostheses (SSP) together, given that they share their main indication, which is use in young adults with good quality bone. However, the truth is that after this shared history they have clearly parted company, and while the use of SP or resurfacing prostheses seems to be in irreversible decline,1 SSP are only now coming into widespread use.2
Young people are increasingly becoming candidates for total hip arthroplasty (THA) to the detriment of femoral osteotomies. Because of their long postoperative recovery times the latter are not always free of morbidity, and they have been giving way to implants which have a far faster and safer recovery period.
THA is one of the most successful procedures in orthopaedic surgery. Together with the excellent results of traditional cemented prostheses, many publications praise the good long-term qualities of uncemented ones.3 Cement is a vulnerable interface in situations of intense activity and it degrades over time, even though it has been proven to give good results over the very long term. Given the bonanza of figures from national arthroplasty records about cemented prostheses, the fact that their manufacturers display less interest in research and development in connection with them is striking. The explanation for this may be purely commercial. Uncemented connections are more biological and direct, and they renew cyclically. From a technical point of view they seem to be less demanding, and they are therefore preferred by surgeons.4
In comparison with older patients, younger ones are more active in work as well as during leisure, and this is a serious challenge for implant survival. Moreover, the new information technologies have contributed decisively to this preference for uncemented prostheses. It has been calculated that a young, healthy and active patient may move their hips through approximately 5 million cycles per year. All orthopaedic surgeons have the objectives of maintaining a good quality of life, preserving the bone and soft tissue and also creating a very stable implant in patients of this type. Once again, national arthroplasty records show that implants in young adults last for far less time than they do in older individuals.5
Implant design, as well as their shape, length, materials and associated surgical technique all play important roles in the success of THA. Nowadays fixing implants has ceased to be the centre of attention, and modern friction joints generate far less relevant amounts of particles due to wear than they used to.6 Nevertheless, some questions remain to be resolved. Preservation of the bone has to be achieved at two levels: less bone should be removed during surgery, although the transmission of the load to the femur has to be optimised. Some publications have already warned of the severe loss of bone that occurs with certain stem designs over the very long term.7 All implants that are in contact with the cortical diaphysary bone and which integrate in the metaphysary part will bring about an anomalous load transfer that over the long-term will cause a loss of bone capital due to stress protection short circuiting (“stress-shielding”). All implants that exclusively anchor in the diaphysary bone may be associated with thigh pain over the short term and loss of proximal bone over the long term. Additionally, as Amstutz and le Duff8 state, extracting the implant if this becomes necessary causes major problems. Due to these and several other reasons, research (which is often industry funded) indicates that smaller prostheses should be used that make more use of the metaphysary zone and less use of the diaphysary zone. This has given rise to the long chapter about the said SSP, which follows the one on SP or resurfacings.
Surface or resurfacing prosthesesJustification of their designMetal-metal joints were widely used in the 1980s. The well-known Metasul (Sulzer AG®, Winterthur, Switzerland) with 28mm heads made of forged metal gave no problems with the liberation of metallic ions. Metallic friction with 28mm heads has not been shown to have any carcinogenic, teratogenic or renal effects. The problems emerged later with SP made of cast metal that was softer and rougher. Once design errors too are taken into account, this explains the higher rate of failures in large diameter metal–metal joints.9
The poor results obtained in young patients when a conventional THA is used were the reason why interest resurged in SP, in an attempt to find implants that are less invasive of the bone. Their indication depends on patient age, bone quality, disease and joint deformity. The revision rate for implants of this type is not inconsiderable. Nevertheless, on condition that patients are selected correctly, their working and results seem to be guaranteed. But this was not always the case, and their use is now always controversial.10 Due to this we believe that this type of implant should be covered by a separate chapter from the corresponding to SSP.
Biomechanical conceptAs their name indicates, SP have to cover the zone of damaged joint cartilage, leaving the interline at the same height and depth as it was in the native hip. I.e., the diameter of the prosthetic head has to be the same as that of the head of the femur, including the thickness of the cartilage. When the head and acetabulum are positioned correctly a surface prosthesis must permit a complete range of movement like the native hip, without this range being any larger or smaller. In degenerative hip disease the osteophytes that increase the natural edge of the acetabulum and the thickness of the neck of the femur cause the reduction in this range of mobility, by facilitating femoral-acetabular impact. These osteophytes have to be removed during surgery without damaging the actual bone. While on the one hand we obtain maximum mobility, on the other we prevent covering false bone (the osteophyte) with the implant, as it is not prepared for loading stresses.
Factors that contribute to failureSP is the most demanding type of primary THA in terms of technique. They are chiefly known for their long learning curve, the need for correct selection of the patient, selection of the design, planning and exact surgical execution. If these conditions are not met, a series of complications may emerge and contribute to the failure of SP. For example, if the acetabulum loosens then the femur neck may fracture. This is associated with notching and the use of sub-hemispherical acetabulums.
In some of the published series the failure rate is now far higher than was expected. Thus in important national arthroplasty records (England and Wales) the figures are worrying.11
As is already known,12 this increase in the SP failure rate is multifactorial and, due mainly to tribological reasons, the result depends on the greater or lesser liberation of metallic ions (principally cobalt and chrome). These cause adverse effects in tissues around the joint as well as systemic ones. Poor positioning of prosthesis components and the difficulty of the surgical technique are also factors that strongly influence the poor short term results for this type of prosthesis.13
Low wear in a metal–metal prosthesis has been defined as <1mm3 per million cycles.14 This figure has to be associated with levels of metallic ions in the blood lower than 10 parts per billion (ppb) as a whole, or less than 5ppb considered individually. At these levels the tissues around the prosthesis do not accumulate high concentrations of metallic ions, so that a balance is reached between their liberation and their elimination.15 To achieve these ideal biological conditions and a low level of wear, the centre of rotation of the head of the prosthetic femur must always coincide with the centre of rotation of the acetabular component. It is equally important that both parts are correctly positioned in the biomechanical axis. In this way the prosthesis will work under mixed lubrication (part of the weight being supported by a film of joint liquid and another part by direct contact between both prosthetic components). The proteins of the lubricating liquid will also form a thin protective film that improves the friction conditions between the metal surfaces.
During the initial period of working (bedding-in) the joint surfaces are self-smoothing (polishing) due to the friction caused by use. The layer of lubricating fluid is established and shaped. During these first months (or years) of working a high number of metallic ions are given off, but from 1 to 3 years this number falls to levels below 1mm3 per million cycles,16 and this figure is maintained during the normal use phase (steady-state).
The diameter of the femoral component also has a direct influence on rates of wear in PS.17 Thus there is less wear during the initial phases in heads larger than 46mm diameter. The smaller the micro-space between both components (clearance) the more wear is reduced, although this ceases to have any influence in the phase of normal use of the prosthesis.
Regarding the type of metal alloy, there is broad agreement and acceptance that the metal should have high carbide content and that it should be a forged alloy with different surface heat treatments.18 The rate of wear published for such alloys lies between 0.1 and 1mm3 per million cycles.
Component orientationWe surely still do not know everything in connection with the positioning of these implants, above all why SP wear quickly under imperfect biomechanical conditions. The main problem in these prostheses appears when their orientation and biomechanical conditions are not ideal. There are a series of situations in which incorrect contact may occur between the head and acetabulum. Under normal conditions the area of contact in the joint interline is aligned with the load axis of the body. However, if the acetabulum is in an excessively vertical position or has version problems, the edge of the acetabulum will articulate with the load zone of the head (edge-loading), giving rise to a high level of wear. The same thing occurs if the head has moved in relation to the axis of the neck of the femur (denominated the head–neck relationship), even when the acetabulum is in perfect position.
The importance of the position of the acetabular component in preserving the lubrication layer as well as in terms of metal ion liberation and the survival of the implant itself has already been cited in publications, in vitro19 as well as in vivo.20 In SP the interline is the most similar to the native one, although this is not the case in conventional THA. Small defects in positioning the acetabulum are counterbalanced by the fact that the neck of the prosthesis is narrower.
Surface acetabulums do not have the same design as those in conventional prostheses. According to Naal et al.,21 they should be somewhat larger than the latter. They should also be at a different angle to favour the lubrication of both parts. While a conventional acetabulum should be at an angle of approximately 45°, this is not the most appropriate angle for SP.
According to the works of Grammatopoulos et al.,22 impact in the SP is the cause of edge-loading, with loss of lubrication and possible wear of material. The risk of impact between the femur and the acetabulum in a surface hip depends on factors due to both components (combined anteversion) and the mobility of the hip in question.
There is a trigonometric relationship between head–neck offset and the angle at which impact occurs. A reduction in offset of 0.1 means that impact will occur 5° beforehand. Women have a greater head-neck offset than men (1.33 and 1.24, respectively). This means that they have a range of movement 11° greater than men. As the size of the neck does not change during the operation to put into place a SP, the size of the head is usually changed and the offset is reduced. This is due to the fact that surgeons tend to save bone on the side of the acetabulum. The greater the native offset, the surgeon has more possibility of reducing the size of the head. But if we reduce the size, we lose range of movement and increase the possibilities of impact.
For a surface acetabulum coxometry must be above the following figures: inclination 40°, anteversion 17°. In any case, it must always be adapted according to the values of the healthy hip. An abduction angle of more than 55 and an anteversion of more than 30 must be avoided, as they may cause wear of the edge and failure within the short term.
The combined anteversion must be personalised in each case, adapting the positioning of the acetabulum according to the head-neck offset and the cervical-diaphysary angle. According to Wan et al.,23 the concept of combined anteversion in a total hip prosthesis originated with Ranawat at the start of the 1990s. It is defined as the sum of the femoral neck anteversion angle plus the acetabulum anteversion angle. According to these authors, its value stands at 37, with a range of ±12. A paper by Schmalzried and Tiberi24 warns of the danger involved in increasing the combined anteversion in a SP. These authors associate the appearance of pseudotumours with this type of technical error.
The orientation of the acetabular component must also take into account possible individual variations in the angle of the pelvis, as Wolf et al. foresaw in their 2005 paper.25 According to Zhu et al.26 a pelvic angle of 10° will lead to an absolute error of 8° in the positioning of the acetabulum in the coronal plane. Moreover, when calculating the combined anteversion an additional error may be committed in the positioning of the femoral component. We know that safe combined anteversion is 37±12. If the pelvic angle is higher than 10, the error may have major clinical implications. These authors insist that combined anteversion must be quantified according to the pelvic angle of each individual, and that it lies between 25 and 50. Additionally, the state of the lumbosacral spine in each patient may involve a particular pelvic positioning during the 3 basic mechanical situations: supine decubitus, sitting and standing. What is known as pelvic incidence (the sum of the slope of the sacral platform and the pelvic inclination in the saggital plane) is particular to each individual. The difference between the pelvic angle of incidence and Cobb's angle corresponding to lumbar lordosis has to be kept below 10°.27 This rule is not always followed, as it varies depending on the degree of flexibility and the degenerative lumbar disease affecting each patient. Nowadays it is known that the positioning of the acetabulum has to follow these lumbopelvic parameters. If this is not done, it increases the possibility that the loaded area of the joint will move and concentrate in zones very close to its edge. This may cause impact and edge loading in SP, with loss of lubrication and possible wear of the material.28
A structure that may be able to help us in aligning the acetabulum component is the transverse acetabular ligament (TAL).29 According to this author, the edge of our acetabulum should be parallel to it. But controversy has also arisen, such as that mentioned by Epstein, who states that it is not always possible to identify the TAL, so that using it as a guide is no better than simple visual estimation.
The use of navigation systemsThe use of navigation systems to ensure a more exact positioning of the acetabular component is increasingly described in publications, as is the case with Krüger et al.30 and other authors.
It also has to be said that the role of such systems during surgery of this type has yet to be fully defined in the literature, although the papers31 in question only describe navigation in connection with the femoral component. Many papers have been written in favour of navigation and against detractors of the system. They not only state that it increases precision in the orientation of the acetabulum, but that it also reduces the number of outliers (values outside average ones) in combined anteversion.32
However, the use of navigation can also lead us to commit errors. Pelvic inclination is defined as the difference between the coronal plane and the antero-posterior (AP) pelvic plane. The coronal is functional (dynamic) and follows the axis of the body. On the other hand, the AP pelvic plane is a static (anatomical) plane. Navigators nowadays position the acetabulum three dimensionally in association with the AP pelvic plane (the anterior–superior iliac spine and the pubic symphysis), which is a static and non-functional plane. Measurements should be based on the functional plane, which is the one that the subject uses to walk and which includes the femur and pelvis. It is the most similar plane to radiography of the pelvis.
Revision surgery in surface prosthesesComparing a SP to a conventional prosthesis may be debatable. SP may seem to be a reasonable step prior to a conventional prosthesis, and even more so if, as Eswaramoorthy et al.33 state, when the switch from a SP to a conventional one takes place in the absence of aseptic lymphocyte-dominated vasculitis-associated lesion (ALVAL), the results are similar to those of a primary prosthesis. The argument about preservation of the acetabular bone in SP compared to conventional prostheses is irrelevant, given that the differences are minimum. However, in terms of the preservation of bone mineral density there is sufficient evidence that SP are better than conventional ones.34,35
What is important is the number of revisions that a young patient will need throughout their life. As Richardson says, with proper patient selection and rigorous surgical technique, SP have a role to play, particularly in younger males. As this author states, the road to “glory” will involve fewer steps. Their role in women is less convincing, although it may be justified in certain cases.
Surface prostheses at the current timeIn September 2010 the Spanish Medicine and Healthcare Product Agency issued a warning about the use of ASR model SP (Depuy Johnson & Johnson®, Warsaw, IN, USA). The warning included the same model for the joint surface but with a stem (ASR XL), referring to large diameter heads by the same brand. This warning was due to the high rate of failures and the possibility that a level of ions (chrome and cobalt) in the blood could be produced with toxic implications. This warning also covered the high number of debris particles of these metals in the tissues around the joint. The angle of coverage of the acetabular component is also an important parameter. Designs in which this angle has been reduced are at greater risk of failure.36
Other countries around the world have done the same, and Australia was the first country to raise the alarm.37 This was why the other SP models in the market were subjected to exhaustive monitoring. Although the problems with them were not equally serious, they were similar in many of them. Finally the suspicion arose that metal on metal friction in these joints could be in itself the cause of many replacements of these prostheses. The rate of revision due to all reasons at 10 years was 7%, and this figure is considered to be unacceptable.
In the same year the Spanish Society for Hip Surgery published an algorithm for the evaluation of patients with a SP, thereby providing a document to help surgeons who see patients of this type.38
Nevertheless, many unanswered questions remained: how to interpret the figures corresponding to metal ions in the blood; how to interpret imaging tests in connection with prostheses of this type; how to treat adverse reactions in the tissues around the joint and how to manage the most problematical cases in clinical terms. All of these subjects are currently being investigated, and attempts have been made in some points to arrive at an international consensus. However, there is as yet insufficient scientific evidence for agreement to be accepted by everyone.38
ConsensusesThe two main consensus documents published in the European and American continents39,40 now seem to agree on the majority of the aspects they study. Nevertheless, all of the aspects relating to long-term studies have yet to be resolved, as these studies are on-going and will not give results for several years.
When considering the implantation of a SP, surgeons will have to obtain the document in which they give their “signed consent”, showing all of the risks that are accepted with this type of implant is used.
Regarding patient selection for prostheses of this type, the first thing that has to be considered is their sex and biological age, based on their activity level and bone quality. Bone mineral density studies have to be used at borderline ages, and the latter differ for men and women. The age limit for men is 65 years old, while for women it is 55 years old (and never after the menopause). Nevertheless, some specialised manufacturers now make use in women conditional on the diameter of the femoral head. Use is contraindicated when femur head diameter is less than 46mm (Smith & Nephew®, Memphis, TN, USA). This size is due to the need to obtain appropriate coverage of the head to prevent wear of the edge. It is also contraindicated in women of fertile age, given the possibility that during pregnancy metal ions may cross the barrier of the placenta. However, it has yet to be proven that metal ions are teratogenic, and this is also the case for the systemic effects of these metals in very long-term carriers.
Surgery has to be properly planned to give satisfactory results. It is recommended that this procedure be reserved for experienced surgeons who perform it at least 20 times per year, as its learning curve is far slower than is the case for conventional THA. Recent studies indicate that surgery assisted by navigation may reduce the learning curve, and that navigation may be the key to guaranteeing the best results with this prosthesis.32,41
Nevertheless, doubts have been raised about the preservation of acetabular bone, which is one of the chief advantages of this prosthesis. Some authors state this bone loss is similar to or even greater than that in conventional THA.42 This argument has recently been overturned in other prospective studies which found that bone loss is no greater than it is in conventional THA.43
Another major advantage of SP is the transfer of loads towards the femoral diaphysis. SP has been found to transmit loads in a more physiological way directly onto the neck of the femur and thereby preventing bone remodelling (stress shielding) as is seen over the long term in conventional prostheses.44
There is no doubt that, as their diameter is very similar to that of the native femoral head, SP reduce the risk of luxation. Large-headed hip prostheses (with heads measuring from 36mm to 54mm) are associated with lower rates of luxation than prostheses with conventional heads (from 22mm to 32mm). In different long-term series luxation was found to be less frequent than it is with conventional THA. The same reason also explains their greater range of movement. SP permit significantly higher levels of activity and a longer arc of movement in comparison with conventional THA.45
Regarding normal gait, in a prospective randomised study that compared operated legs with the other one, Girard et al.46 found that SP reproduce native offset and leg length more faithfully than conventional THA. In another study of walking, Mont et al.47 showed that functionality and kinematics were better in patients with SP than they were in those with conventional THA for patients with similar characteristics in both groups.
At another level SP aid prosthesis implantation in the case of femoral deformities or if previously implanted material is present.48 The ease of a hypothetical change is also comprehensible. If the femoral component fails, it is possible to cut the neck and implant a conventional large-headed prosthesis without too many problems. The extraction of the acetabular component does not give rise to too many problems since the specific instrument known as Explant (ZimmerBiomet®, Warsaw, IN, USA) became available.
ConclusionsTo summarise and round off this paper, we are able to state that the idea that SP have vanished and will never return is unreal. On the other hand, it is correct that they are a type of prosthesis which has to be implanted by experienced surgeons in high volume hospitals. Patients have to be rigorously selected, and they also have to sign a specific document giving their informed consent. I believe that once it is possible to change the friction joint (to ceramic-ceramic, for example), SP will once again enter our therapeutic arsenal, as they have done several times in the past.
Short-stem prosthesesIntroductionThe use of SP is strongly restricted by its requisites in terms of bone quality, patient sex (as it is hardly recommendable for women), joint deformity and the fact that it liberates metal ions into the blood. All SP manufacturers are rushing to commercialise SSP to counterbalance these limitations. Anchoring prostheses exclusively in the metaphysary part close to the femur, without invading the subisthmic medullar cavity seems to be a more reasonable option in terms of transmitting loads to the diaphysis. For young patients, SSP are implants that seem to be half-way between SP and THA, as they have the advantages of the one while avoiding the drawbacks of the other. Their revision rate, without adjusting for patient age, is slightly higher than it is for conventional THA, with 95% survival at 10–15 years.49,50
Rational design historyIt is by starting at the beginning that we will better understand the present. In 1917, Koch51 proposed his famous model of the load mechanics in the femur. Following Wolf's laws, Koch assigns compression and tension zones along the whole femur. Koch's model was considered to be definitive for more than 70 years, and it was used as the basis for the development of the vast majority of femoral stems from the 1960s onwards.
Nevertheless, Koch's model was static and did not take into account the different soft structures that interact with the femur during walking. Thus this model was revised and updated year later by Fetto et al.52 According to these authors, while bodyweight is being supported by one leg, it is thanks to a static tension band (the iliotibial band) and another band under dynamic tension (the gluteal medius-vastus lateralis complex) in the external part, that compression forces are transmitted from the greater trochanter towards the distal femur, through the medial as well as the lateral part.
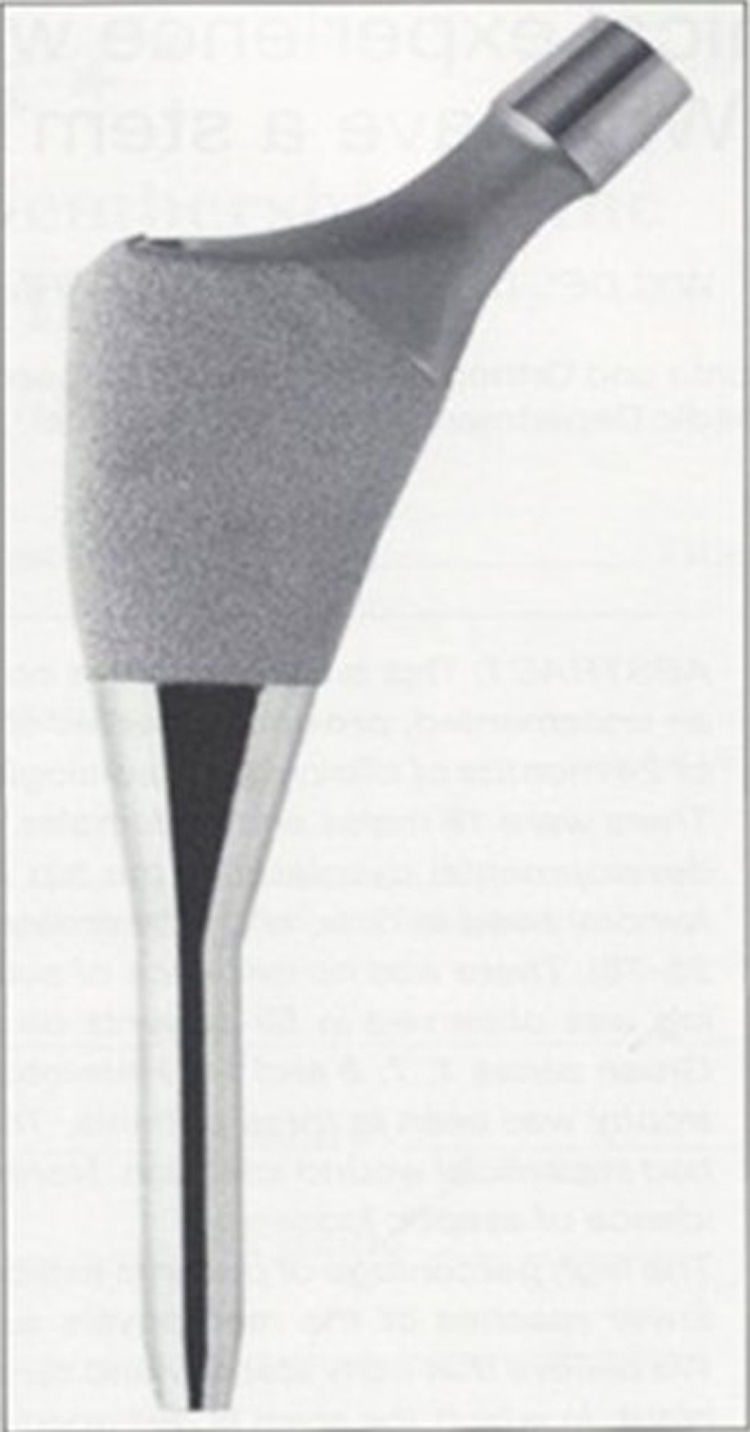
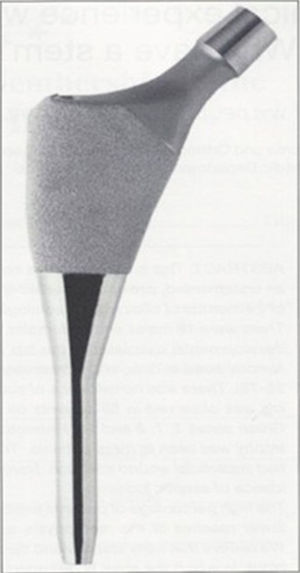
In 1999 Walker53 discovered that when the stem is anchored in the trochanteric part, loads are distributed by the proximal metaphysary part. On the contrary, if the stem lacks this expansion towards the trochanteric zone, loads are transmitted towards the distal half of the femur, in the diaphysary zone. The authors conclude that femoral stems should make contact with the external cortical metaphysary bone as an additional area of support. This prevents it from sinking into the cavity, preventing stress-shielding and the resulting loss of bone in the proximal femur. This fact was also demonstrated radiographically in 2002 by Leali et al.,54 New York (of the same school as Fetto et al.52). This gave rise to a change in the classical model of stems, which progressed to have a more metaphysary support such as the well-known IPS design (Depuy, Leeds, United Kingdom).55 The chief particularity of this design is that it attempts to prevent distal osteointegration (Fig. 1) to improve thigh pain which appears due to the frequent “point effect”.
At the start of the new millennium, Morrey et al.,56 of the Mayo Clinic (Rochester, MN, USA), burst into the literature with the excellent results obtained with the use of small-stemmed prosthesis. Years later, other authors supported the theories of Morrey et al. with similar results.57,58 They were actually introducing a conceptual shift. New shorter designs that are able to make far less use of the diaphysary bone, concentrating their anchorage exclusively in the metaphysary part. Years later, in 2006, Kulkarni et al.59 published a crucial question: “Why do we have a stem?”: the excellent results arising from the use of the IPS stem (Depuy, Leeds, United Kingdom) lead us to think that there is a natural evolution towards a short implant without a stem.60 This responded to the new tendency towards minimally invasive surgery, in which a shorter stem was easier to insert into the medullar cavity. Thus in 2010 Santori and Santori61 published excellent results after 8 years, with 5 loosenings in 129 cases, using an adhesive-free design known as the Proxima stem (Depuy®, Leeds, United Kingdom). However, and in spite of its good results and due to purely commercial reasons this stem ceased to be commercialised in 2013.
Westphal et al.,62 of Morlock's Hamburg group, also compared the Santori stem with conventional ones. They found that the short stem system is less rigid than the long stem system. This indicates a more physiological transmission of loads, in spongy as well as cortical bone. Patel et al.63 found better bone remodelling in Gruen zones 2, 3, 5 and 6, indicating more physiological load transfer and less stress-shielding.
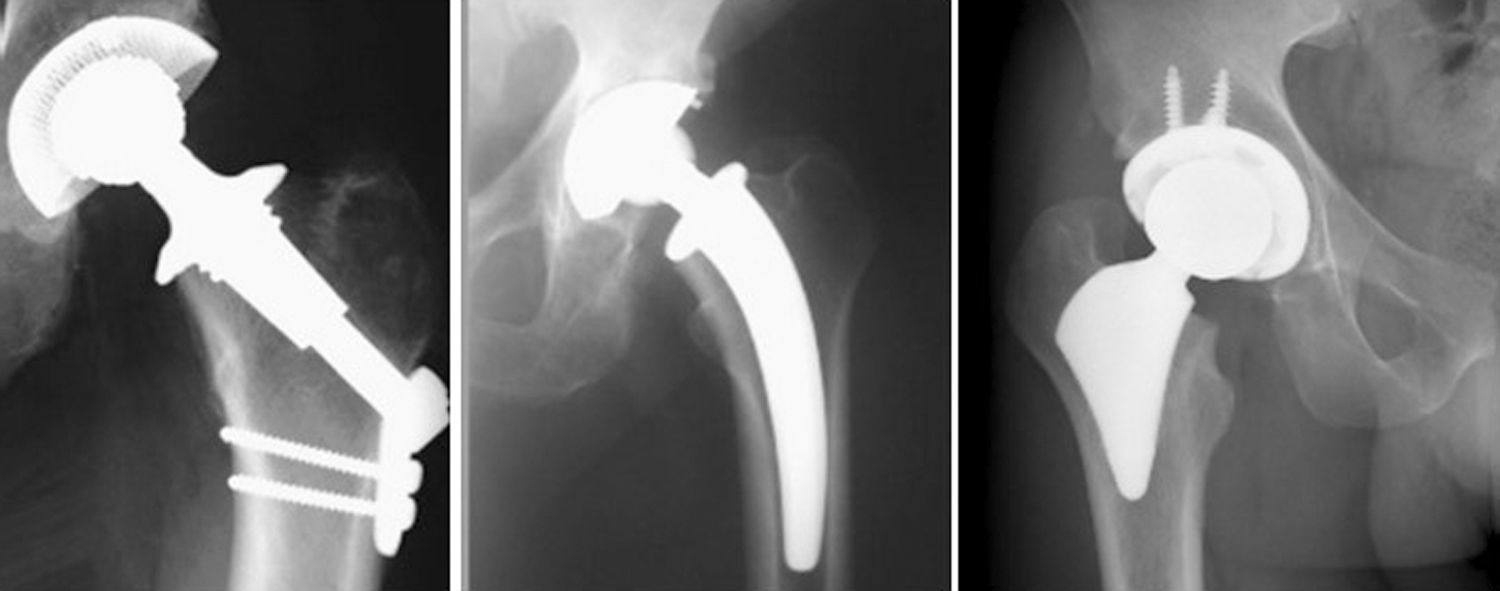
Short-stemmed prosthesis classificationThere are several classifications for the different short stem concepts. One of the most widely used in practice is Learmonth's.64 In general, bone preservation stems may be divided into 3 categories (Fig. 2):
- 1.
Implants that expand into the trochanteric zone.
- 2.
Implants supported in the femoral neck.
- 3.
Implants supported in the external cortex.
X-ray appearance of types of short stem, according to Learmonth.64
The studies by the Italian Pipino65 of his femoral neck stem are well-known. Although these very long-term studies are spectacular, we should not forget that he designed the system. With the same stem other authors have not encountered such fantastic results. One example of this is the study by Pons,66 indicating that a certain learning curve is necessary when using stems of this type. Nevertheless, Briem et al.67 found very good results with a 6-year follow-up, with only one change in 155 cases.
A recent meta-analysis by Rometsch et al.68 of 460 papers on 14 types of short stem survival and taking the end point as revision due to any cause, found a revision rate of 0.38% at the end of a follow-up lasting for at least 2 years.
In recent years a certain degree of confusion has arisen when talking about short stems. This problem is due to the lack of a clear division between those that are supported by a certain degree of scientific evidence and those which are not. This division is equivalent to the one between those which can be recommended and those which cannot.
In 2014 Khanuja et al.69 tried to answer the above question in their paper. Given the existence of different types of proximal anchorage in these short “bone preservation” stems, a classification system that makes it possible to compare their clinical results is essential.
They classify them into 4 large groups which, in turn, are sometimes classified into subgroups: type 1 A, prosthesis supported exclusively on the trapezoid cross-section neck; type 1 B, prosthesis supported exclusively on the neck with a rounded geometry and with strias for rotational stability; type 1 C, prosthesis supported exclusively on the neck with spiral geometry for rotational stability; type 2 A, prosthesis that applies load to the trapezoid cross-section calcar and with a wedge design; type 2 B, prosthesis that applies load to the rounded cross-section calcar with preservation of the femoral neck; these may also have strias; type 2 C, neck preservation stem with threaded anchorage on the lateral metaphysary cortex; type 2 D, thrust plate or screw-plate design that compresses the calcar against the external cortical metaphysary; type 3, rods with lateral trochanteric expansion, and type 4, a stem with a conventional design but shorter in length, with the aim of solely metaphysary anchorage in the proximal femur (Fig. 3).
The types of short stem proposed by Khanuja et al.69
Classification of degrees of recommendation of the most accepted treatment was proposed by Wright et al.70 In this he suggests the following 4 types: A, good evidence (level I) in favour or against; B, medium evidence (levels II–III) in favour or against: B, medium evidence (levels II–III) in favour or against; C, poor evidence or evidence with a conflict of interests (levels of evidence IV–V) and weak routine recommendation; I insufficient evidence, making it impossible to recommend routine. Based on this classification the recommendation to use short stems, given current publications, would be as follows:
- -
Type I degree of recommendation (i): some stems IIA (Nanos, Smith & Nephew®, Memphis, TN, USA), some IIC, III and IV only as updates or innovation (Taperloc Microplasty, Zimmer Biomet®, Warsaw, IN, USA).
- -
Type C degree of recommendation: other rods IIA (Metha, Waldemar Link®, Hamburg, Germany) (Mayo, Zimmer Biomet®, Warsaw, IN, USA), IIB (CUT, ESKA Orthodynamics®, Lübeck, Germany) and IID (TPP, Aesculap AG®, Tuttlingen, Germany).
- -
There is insufficient degree of recommendation for the other types of design.
As is the case with SP, SSP too are technically demanding. The reason for this often lies in the lack of a tutor in the distal part of the implant. The high prevalence of poor orientation, size, sinking and intraoperative fractures means that stems of this type are now feared in some way by some surgeons. Stronger clinical evidence is needed, including randomised prospective multicentre trials that compare THA with these new designs, before they can be recommended for general use.
In connection with the preservation of the soft tissues, current tendencies are marked by the search for new access routes that are less invasive of the groups of muscle around the joint (intermuscular surgical routes). Due to this the Watson-Jones, Kocher-Langenbeck and Hueter route variants will without doubt be often used by new generations of orthopaedic surgeons. Although the anterior direct route requires overcoming a steep learning curve, its postoperative results are spectacular. In some very high level contexts this is leading to implantation in day hospital regime. The maximum preservation of the anatomical structures with nerves that play a crucial role in proprioceptive sensitivity (the posterior cotiloid labrum, according to Ganz) and the use of large diameter heads make prosthetic joints more functional, while also reducing the probabilities of luxation.
In a recent study71 the London group of Fares Haddad found that the efficacy of a short, conical and porous stem proved very favourable in comparison with a conventional uncemented standard length component, in terms of the functional results perceived by patients. Although the early radiological findings are positive, long-term follow-up is necessary to evaluate the impact of short stem alignment and migration to be able to talk about survival.
ConclusionsGiven the above, and taking into account the fact that there is no clear answer to the question “what does being young consist of?”, to conclude the personal opinion of the authors is that many questions still have to be resolved and require future studies, even though the short-term results are promising. It is a reasonable question that, given that this type of prosthesis is only used in younger patients, we may be contradicting what is ethically permissible. This possibility is amplified if we taken into account the fact that adults are living for longer and longer.
Level of evidenceLevel of evidence v.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Gallart X, Riba J, Fernández-Valencia JA, Bori G, Muñoz-Mahamud E, Combalia A. Las prótesis de cadera en el adulto joven. Prótesis de superficie y prótesis de vástago corto. Rev Esp Cir Ortop Traumatol. 2018;62:142–152.