The indications on extraction of osteosynthesis material (EMO) are not well defined in the current literature deriving in relative indications, depending on experiences, customs or patient's request. The aim of this article is to assess the beliefs, indications, usual practice and perceived complications of surgeons in Spain regarding OME.
MethodsWe conducted a questionnaire of 44 questions covering general demographics, general and subjective opinion on implant removal, specific attitudes by implant type and anatomical location, and personal habits.
Results164 questionnaires were received. The most frequent indications are patellar and olecranon locks and elastic nails in children. 56% remove the implant at the patient's request, 31% always remove it in children, 28% do it in asymptomatic patients to avoid possible surgical problems, 14% to avoid a possible peri-implant fracture and 9% by simple preference. The most frequent intraoperative complications are surgery longer than expected, bone growth over the implant, rounded screw head core, cold fusion, difficulty in finding the implant and impossibility to remove part of the implant. The most frequent postoperative complication was persistence of symptoms 39.8%.
ConclusionThe results provide information to advise the patient regarding the expected clinical outcome and intra and postoperative complications. The surgeon should cautiously indicate extraction in the asymptomatic patient given the high rate of complications.
Las indicaciones sobre extracción de material de osteosíntesis (EMO) no están bien definidas en la literatura actual derivando en indicaciones relativas, en función a experiencias, costumbres o a petición del paciente. El objetivo de este artículo es valorar las creencias, indicaciones, práctica habitual y complicaciones percibidas de los cirujanos de España sobre la EMO.
Material y MétodoRealizamos un cuestionario de 44 preguntas que abarcan demográficos generales, opinión general y subjetiva sobre la retirada de implantes, actitudes específicas por tipo de implante y localización anatómica y hábitos personales.
ResultadosSe reciben 164 cuestionarios. Las indicaciones mas frecuentes son cerclajes en rótula y olecranon y clavos elásticos en los niños. Un 56% retira el implante a petición del paciente, un 31% lo retira siempre en niños, un 28% lo hace en pacientes asintomáticos para evitar posibles problemas quirúrgicos y un 14% para evitar una posible fractura periimplante y un 9% por simple preferencia. Las complicaciones intraoperatorias mas frecuentes son cirugía mas larga de lo esperado, crecimiento de hueso sobre el implante, alma de la cabeza del tornillo redondeada, fusión fría, dificultad para encontrar el implante e imposibilidad para retirar parte del implante. La complicación postoperatoria más frecuente es la persistencia de la sintomatología 39,8%.
ConclusiónLos resultados aportan información para aconsejar al paciente en cuanto al resultado clínico esperado y las complicaciones intra y postoperatorias. El cirujano debe indicar con cautela la extracción en el paciente asintomático dada la alta tasa de complicaciones.
Indications on extraction of osteosynthesis material are not well defined in the current literature, with no existing protocols to establish indication. For this reason the number of osteosynthesis material extractions (OME) varies greatly from one country to another, and in some cases accounts for 30% of elective surgical indications.1,2
For adults there is consensus regarding the removal of implants in cases of pseudo osteoarthritis, rupture, infection, allergy or soft tissue compromise. In the case of a consolidated fracture the indication comes from the actual surgeon, depending on the clinical symptoms of the patient, but also depending on their experience, beliefs and habits.2–7 This gives rise to OME indications which in many cases are relative, such as stemming from the express desire of the patient,3,5 pain attributed to the implant5, desire/habit of the surgeon,3,5 age,6,8 difficulty and /or complications for extraction, depending on the material of the implant8–11 (steel or titanium) or its anatomic location,7,12,13 attachment through joints,1,14 removal to prevent possible peri-implant fracture and refracture,1 length of time with implant,1 or risk of carcinogenesis15 or allergy to metals.16
The aim of this article was to evaluate the beliefs, indications, regular practice and complications perceived by the surgeons in Spain on the extraction of osteosynthesis material.
Material and methodsAfter conducting a systematic search in Pubmed Medline, Embase and Google Scholar of surveys relating to implant extraction,3–7 we designed a questionnaire which was similar to that of Vos et al.3 adapted to the Spanish health system, including public and private health. The said questionnaire comprised 44 questions; 4 on general demographic data, 11 on general opinion and subjective opinion on implant extraction, 17 on specific attitudes by type of implant and anatomic location and 11 on personal ideas and habits.
The demographic data requested by the survey included age range, sex, place of work (public or private health and hospital size) and sub-speciality to which they were mostly dedicated.
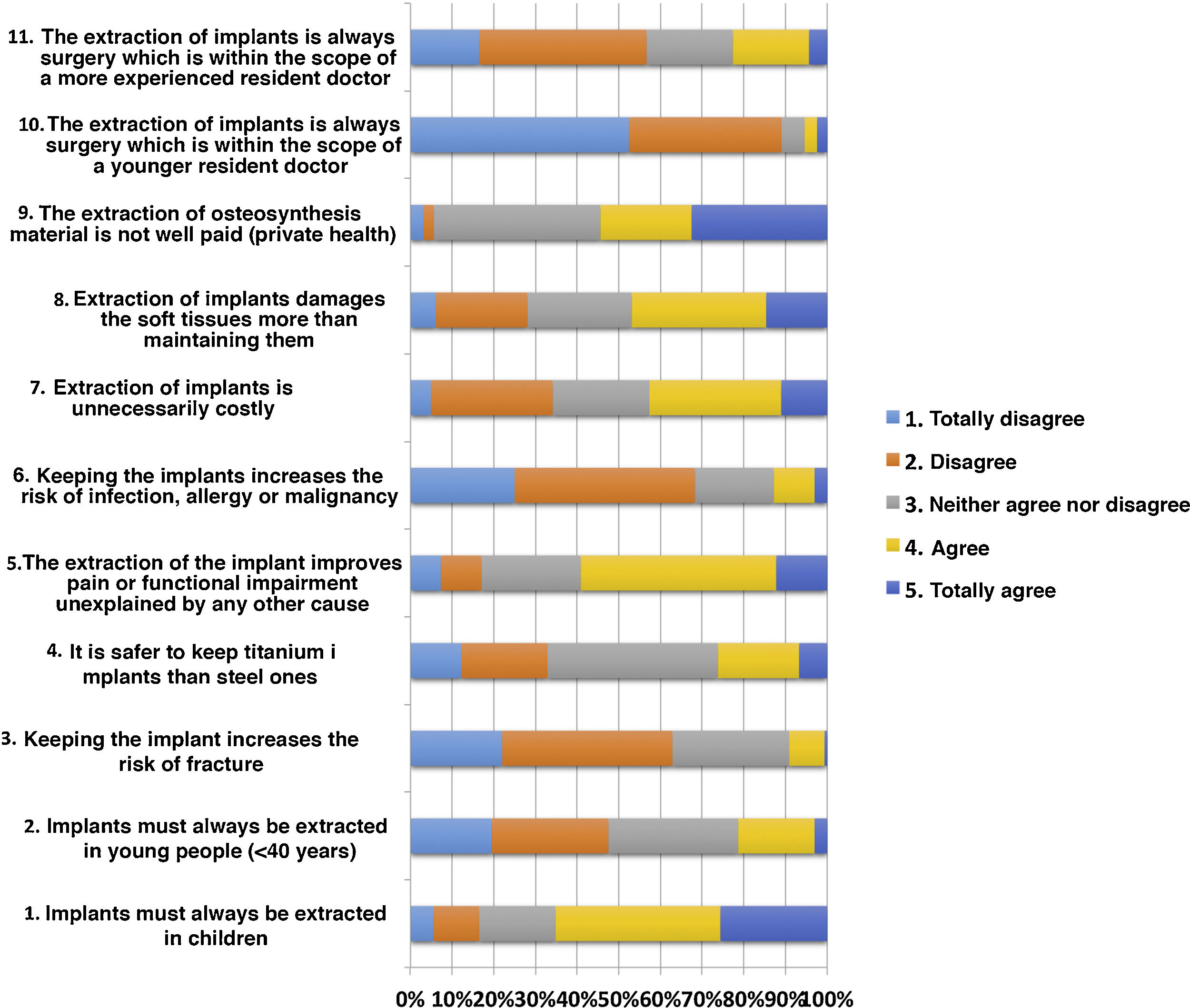
The general opinion and evaluation of surgery (11 items) was measured using the Likert subjective evaluation scale on the subject, with 5 response options, of which only one could be chosen: totally disagree, disagree, neither disagree nor agree, agree, totally agree.
The questions on specific attitude by type of implant and locoation (17 items) was measured using a Likert scale of subjective assessment with 5 response options, of which only one could be chosen: never, sometime, frequencly, always, no comment.
Responses on personal ideas and habits (12 items) were responded to with “yes” or “no”, depending on whether the surgeon agreed with the proposed opinon and several options for each section could be chosen.
The questionnaires were sent by email to different hospitals in Spain, inviting participants to complete it in Google forms. No financial or any other incentive was offered for questionnaire completion. All responses were analysed using a descriptive statistical analysis.
ResultsOf the questionnaires sent to the different hospitals, to be completed by members of the service, a total of 164 were received in Google forms.
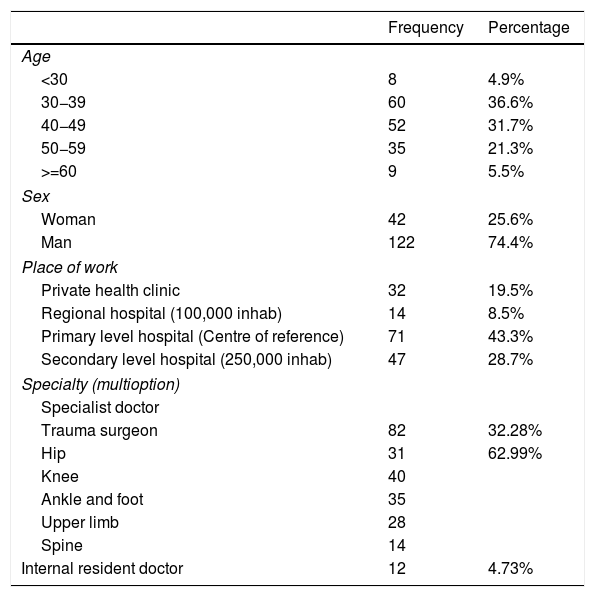
Demographic data are contained in Table 1.
Demographich data.
| Frequency | Percentage | |
|---|---|---|
| Age | ||
| <30 | 8 | 4.9% |
| 30−39 | 60 | 36.6% |
| 40−49 | 52 | 31.7% |
| 50−59 | 35 | 21.3% |
| >=60 | 9 | 5.5% |
| Sex | ||
| Woman | 42 | 25.6% |
| Man | 122 | 74.4% |
| Place of work | ||
| Private health clinic | 32 | 19.5% |
| Regional hospital (100,000 inhab) | 14 | 8.5% |
| Primary level hospital (Centre of reference) | 71 | 43.3% |
| Secondary level hospital (250,000 inhab) | 47 | 28.7% |
| Specialty (multioption) | ||
| Specialist doctor | ||
| Trauma surgeon | 82 | 32.28% |
| Hip | 31 | 62.99% |
| Knee | 40 | |
| Ankle and foot | 35 | |
| Upper limb | 28 | |
| Spine | 14 | |
| Internal resident doctor | 12 | 4.73% |
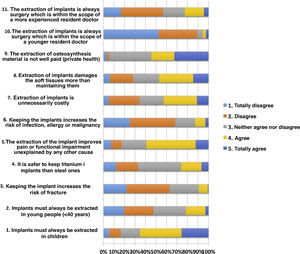
Fig. 1 shows the results of the “general opinion” questionnaire which comprises 11 items and shows very graphically the huge disparity of opinions existing on this issue in the same location.
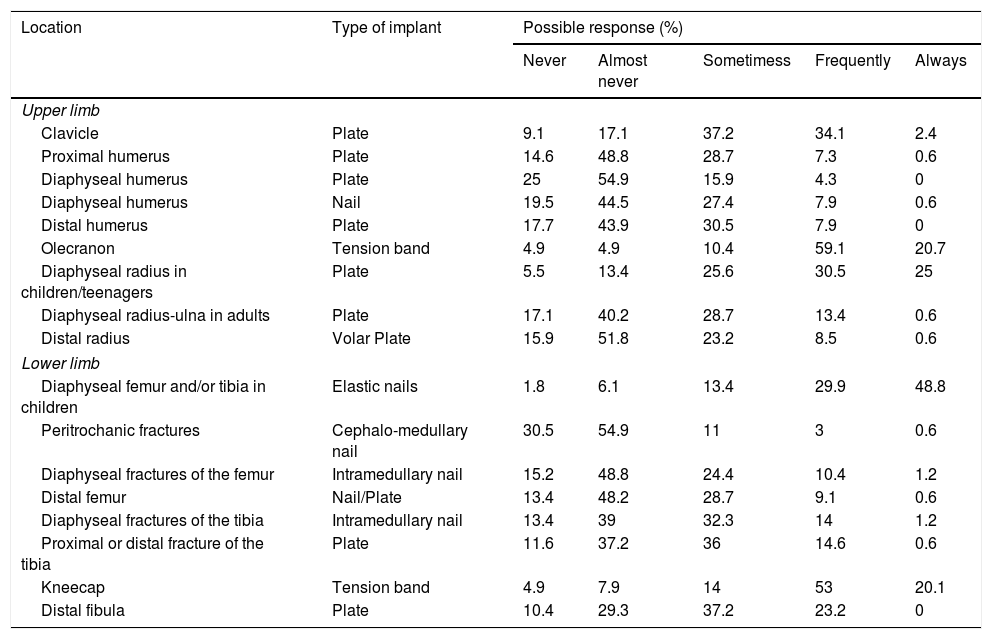
Table 2 shows the attitude and indications made by the Spanish orthopaedic surgeons depending on the type of implant to be extracted and its location. This survey consisted of 17 different situations, in which a relative consensus was appreciated regarding the extraction of patellar and olecranon cerclage wires and elastic nails in children, with a more irregular distribution in the remainder of situations.
Tendency regarding removal by type of implant and location.
| Location | Type of implant | Possible response (%) | ||||
|---|---|---|---|---|---|---|
| Never | Almost never | Sometimess | Frequently | Always | ||
| Upper limb | ||||||
| Clavicle | Plate | 9.1 | 17.1 | 37.2 | 34.1 | 2.4 |
| Proximal humerus | Plate | 14.6 | 48.8 | 28.7 | 7.3 | 0.6 |
| Diaphyseal humerus | Plate | 25 | 54.9 | 15.9 | 4.3 | 0 |
| Diaphyseal humerus | Nail | 19.5 | 44.5 | 27.4 | 7.9 | 0.6 |
| Distal humerus | Plate | 17.7 | 43.9 | 30.5 | 7.9 | 0 |
| Olecranon | Tension band | 4.9 | 4.9 | 10.4 | 59.1 | 20.7 |
| Diaphyseal radius in children/teenagers | Plate | 5.5 | 13.4 | 25.6 | 30.5 | 25 |
| Diaphyseal radius-ulna in adults | Plate | 17.1 | 40.2 | 28.7 | 13.4 | 0.6 |
| Distal radius | Volar Plate | 15.9 | 51.8 | 23.2 | 8.5 | 0.6 |
| Lower limb | ||||||
| Diaphyseal femur and/or tibia in children | Elastic nails | 1.8 | 6.1 | 13.4 | 29.9 | 48.8 |
| Peritrochanic fractures | Cephalo-medullary nail | 30.5 | 54.9 | 11 | 3 | 0.6 |
| Diaphyseal fractures of the femur | Intramedullary nail | 15.2 | 48.8 | 24.4 | 10.4 | 1.2 |
| Distal femur | Nail/Plate | 13.4 | 48.2 | 28.7 | 9.1 | 0.6 |
| Diaphyseal fractures of the tibia | Intramedullary nail | 13.4 | 39 | 32.3 | 14 | 1.2 |
| Proximal or distal fracture of the tibia | Plate | 11.6 | 37.2 | 36 | 14.6 | 0.6 |
| Kneecap | Tension band | 4.9 | 7.9 | 14 | 53 | 20.1 |
| Distal fibula | Plate | 10.4 | 29.3 | 37.2 | 23.2 | 0 |
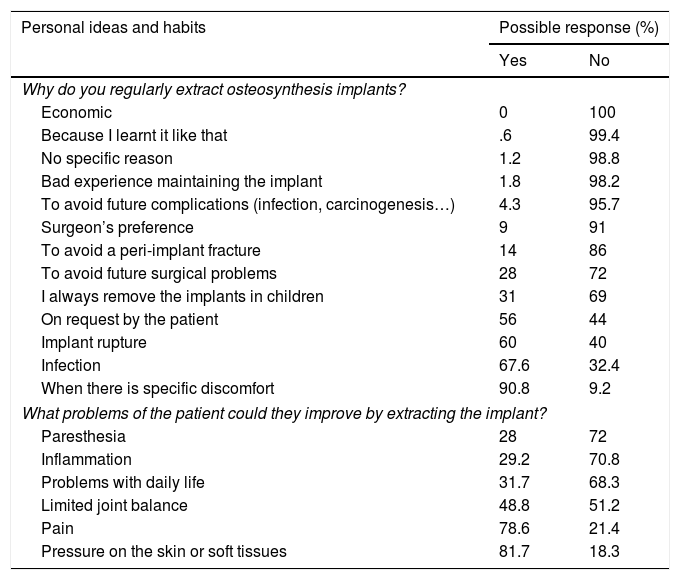
Table 3 summarsies the main reasons why OME was indicated. It explores 12 reasons and we see that with the exception of “implant rupture” which usually means a lack of consolidation, “infection” and “specific discomfort caused by the implant”, the other indications such as “on request of the patient”, “surgeon’s preference” or “to avoid possible future problems”, could be classed as subjective.
Reason why they regularly extract osteosynthesis implants.
| Personal ideas and habits | Possible response (%) | |
|---|---|---|
| Yes | No | |
| Why do you regularly extract osteosynthesis implants? | ||
| Economic | 0 | 100 |
| Because I learnt it like that | .6 | 99.4 |
| No specific reason | 1.2 | 98.8 |
| Bad experience maintaining the implant | 1.8 | 98.2 |
| To avoid future complications (infection, carcinogenesis…) | 4.3 | 95.7 |
| Surgeon’s preference | 9 | 91 |
| To avoid a peri-implant fracture | 14 | 86 |
| To avoid future surgical problems | 28 | 72 |
| I always remove the implants in children | 31 | 69 |
| On request by the patient | 56 | 44 |
| Implant rupture | 60 | 40 |
| Infection | 67.6 | 32.4 |
| When there is specific discomfort | 90.8 | 9.2 |
| What problems of the patient could they improve by extracting the implant? | ||
| Paresthesia | 28 | 72 |
| Inflammation | 29.2 | 70.8 |
| Problems with daily life | 31.7 | 68.3 |
| Limited joint balance | 48.8 | 51.2 |
| Pain | 78.6 | 21.4 |
| Pressure on the skin or soft tissues | 81.7 | 18.3 |
Regarding time from osteosynthesis to extraction, 64.4% of respondents waited over 12 months and 31.7% waited between 6 and 12 months.
The ease with which the material was extracted depending on its composition is significant for 62.8% of respondents. They suggest that stainless steel is easier to extract than titanium, 26.8% find no difference between them or have no experience and only 10.4% think that titanium is easier to extract.
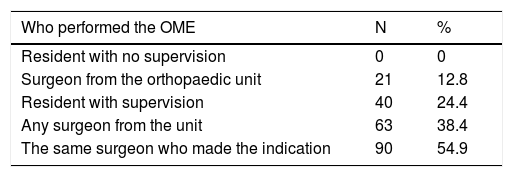
In most centres, extraction was performed by the same surgeon who made the indication and never by a resident with no supervision. However, in 38% of cases this removal could have been performed by any surgeon of the unit (Table 4).
For the respondents, there is a clear relationship between the appearance of complications and the level of experience and subspecialty of the surgeon. Thus, 64% of respondents believe that complications increase when there is a lower level of experience and 54.9 believe that the subspecialty of the surgeon is also a determining factor. Only 8% find there is no relationship with the level of experience and 32% with the speciality.
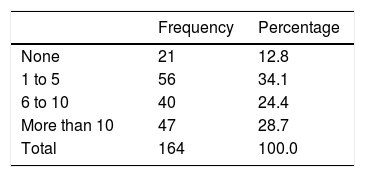
The amount of times where the presence of an osteosynthesis implant has conditioned indication for elective surgery seeks to discover the indications made to prevent a problem which may possibly never occur. An example of this is the removal of a femur nail to prevent removing it if the patient requires a hip arthroplasty or the removal of tibial plateau plates in case the patient needs a knee arthroplasty. In the survey, up to 71.3% of respondents had not experienced this situation more than ten times throughout their professional career.
When planning surgery, when extractions were foreseeably complex, most surgeons (141) used the implant surgical technique, but whilst half (70) also used the literature and articles on techniques and tips, the other half (74) of the surgeons improvised when extraction became complicated. Regarding specific material in preoperative planning, only 26.8% of respondents had a specific OME box. 69.5% of respondents requested it if they believed it would be difficult and 3.7% improvised with the specific material of the operating theatre (Table 5).
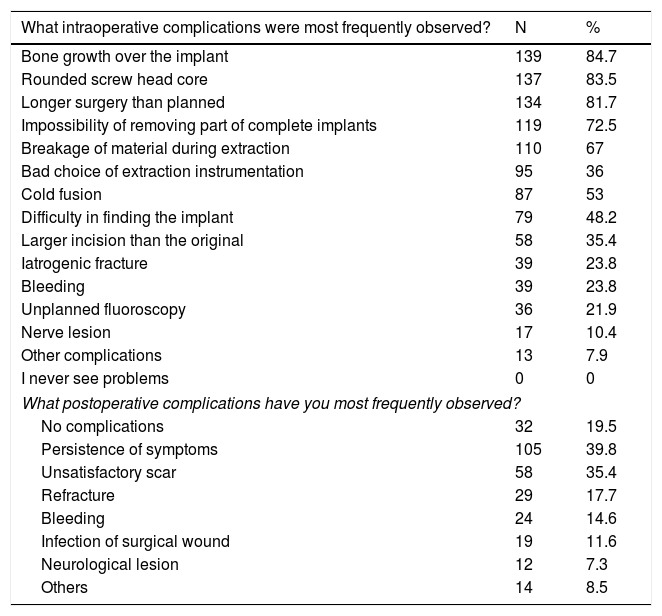
Intra and postoperative complications observed with greater frequency are contained in Table 6. Among these it is notable that all participants have observed some of the complications described, and that among the postoperative ones, 40% found the persistence of symptoms to be among the most common complications.
Intra and postoperative complications observed after the removal of osteosynthesis implants.
| What intraoperative complications were most frequently observed? | N | % |
|---|---|---|
| Bone growth over the implant | 139 | 84.7 |
| Rounded screw head core | 137 | 83.5 |
| Longer surgery than planned | 134 | 81.7 |
| Impossibility of removing part of complete implants | 119 | 72.5 |
| Breakage of material during extraction | 110 | 67 |
| Bad choice of extraction instrumentation | 95 | 36 |
| Cold fusion | 87 | 53 |
| Difficulty in finding the implant | 79 | 48.2 |
| Larger incision than the original | 58 | 35.4 |
| Iatrogenic fracture | 39 | 23.8 |
| Bleeding | 39 | 23.8 |
| Unplanned fluoroscopy | 36 | 21.9 |
| Nerve lesion | 17 | 10.4 |
| Other complications | 13 | 7.9 |
| I never see problems | 0 | 0 |
| What postoperative complications have you most frequently observed? | ||
| No complications | 32 | 19.5 |
| Persistence of symptoms | 105 | 39.8 |
| Unsatisfactory scar | 58 | 35.4 |
| Refracture | 29 | 17.7 |
| Bleeding | 24 | 14.6 |
| Infection of surgical wound | 19 | 11.6 |
| Neurological lesion | 12 | 7.3 |
| Others | 14 | 8.5 |
The most significant thing about this survey is that, regardless of its limits, it shows the huge disparity of opinions and treatment guidelines existing in Spain. Also, similarly to surveys conducted in other countries,3–7 it also shows how a large number of indications are subjective, and have little scientific rigour, such as “on request of the patient”, “according to the surgeon’s preference”, “bad previous experience”, “habit” or “paediatric age”. This contrasts with the large quantity of intra and postoperative complications which were perceived by participants (Tables 3 and 6).
This is reflected in detail in Table 3, where we see that with the exception of “implant rupture”, “infection” and “specific implant discomfort”, the remainder of indications are subjective, conditioned by previous learning, beliefs, preferences or to avoid situations which may perhaps never happen…. However, this is constant in the literature, where Reith et al.5 refer to the most common indication (in 68%) being the surgeon’s recommendation or Vos et al.3 refer to 68% as the express request of the patient and 42% to avoid possible future surgical problems or peri-implant fractures in patients who practice high risk sports.
Relative indication: paediatric ageOne of the main factors taken into account when making the indication is the patient’s age. In the paediatric patient, most indications are related to the removal of screws, Kirschener wires, and elastic nails, to surgery which in the literature is associated with a low level of complications.17 Although there is some consensus about these indications, there is still discordance for the OME indication among non paediatric surgeons,3 whose indication is mostly based on avoiding future complex extractions due to bone growth over the implant or aimed at possible reconstructive surgery in adult age, and the paediatric surgeons,6 who are more reluctant to remove material from an asymptomatic patient. Despite this, there is currently no evidence to support maintaining or removing implants from children.8
Paediatric surgeons defend a judicious indication, because when the indication is made the implant does not cause discomfort, and depending on the location, an extremely high rate of complications may occur, up to 40% in the case of the removal of plates in forearm fractures,13 or the removal of nails after epiphysiolysis of the femoral head. Ilchmann18 describes how time in surgery is doubled for extraction to that of implantation, for peri-implant fractures and difficulty in material extraction. For their part, other authors such as Swiontkowski19 describe greater difficulties for the extraction, in 61% of patients, Jabo20 in 27% and Khale21 in 42%.
In a more recent study, Raney et al.8 describe an OME rate of complications in paediatric patents which is 10%, raising these figures to 34% in the case of epiphysiolysis of the femoral head. Based on these figures, the indications in the asymptomatic paediatric patient should be studied in detail.
Relative indication: young patient and possible future surgical problem (due to peri-implant fracture or arthroplasty)In the young adult (<40 years) the main potential problem determining indication is possible reconstruction surgery in adult age, hip and knee arthroplasties being the most frequent, and the risk of peri-implant fracture in the case of sports.
In our survey, 28% of participants referred asymptomatic patients for surgery to prevent possible surgical problems, in this case related to hip or knee arthroplasty. However, the amount of times which participant surgeons had been faced with the dilemma of having to perform an OME followed by a difficult arthroplasty in one or two stage surgery was low, since up to 71.3% of respondents had not experienced such a circumstance more than ten times throughout their professional careers.
In the case of hip arthroplasty there are authors22 who advocate a two-stage surgical process, firstly extracting the material and secondly performing arthroplasty. This means that on many occasions the advantage of extracting the material in patients of paediatric age or a young patient would not reduce the number of operations. However, if we take the case of tibial plateau fractures and the need for knee arthroplasty, although it is true that the probability increases after the fracture, after 10 years only 7.3% of patients require arthroplasty.23 In this case, a routine OME would not be justified in over 90% of patients who did not need knee arthroplasty. However, it could be indicated in the symptomatic patient, since removal of the implant and arthroplasty in a single stage could be associated with a higher rate of infection, and prior material extraction to a knee arthroplasty could relieve the clinical symptoms.
This could suggest that maybe the number of asymptomatic patients for whom OME is indicated (number of patients to treat) and whose complications are considered is too high to justify the benefit obtained.
Indication to surgery due to the risk of peri-implant fracture during sports is also relative, since this risk is extremely low,24 and should therefore not be a reason for extraction. This is a highly interesting point, since even in the subgroup of sportspeople, fire-fighters, and soldiers the risk of peri-implant fracture does not justify this indication.25
Complications (Table 6)One of the most frequently observed intraoperative complications is longer surgery than expected, the consequence of common complications such as bone growth over the implant, rounded screw head core, cold fusion, difficulty in finding the implant, to remove part or all of it. Due to the frequency of these complications, it is notable that for only 26% of respondents was a specific material extraction box available in their hospital and less than half of them referred to the scientific literature on this issue, whilst improvising when complications arose.
The most relevant postoperative complications, frequently reflected in the questionnaire were neurological lesions, refracture, wound infection and persistence of symptoms.
Neurological lesion (11% in our survey) has been described in the literature and is mostly associated with forearm fractures. In the series of 55 patients of Langkamer et al.13 they described 40% complications, of which 17 corresponded to neurological problems and 4 to infections. In one meta-analysis of 635 cases, Evers et al.26 described a frequency of 11.5%of iatrogenic neurological lesions following the removal of plates in the forearm.
Refracture (17.7%): in refractures, the radius and ulna diaphyseal plates in children deserve special attention since although the main indication for their extraction is refracture this is uncommon when the plates are maintained. Both Clement27 and Vopat28 described a rate of 7% peri-plate fractures in paediatric patients where they were not removed, concluding that maintaining the plate did not increase the risk of refracture compared with removal. In the studies conducted after the removal of plates, Mih29 reported a rate of 11.3% refracture, and Evers,26 in a meta-analysis of 635 cases, that of 7.7%, significantly associated with the use of 4.5 mm plates, OME before 12 months, open fractures and poor anatomic reduction.
Surgical wound infection (11.6%). Surgical wound infection, observed by 11.6% of respondents, is one of the most common postoperative complications. These rates observed are consistent with the literature,30–32 which describes surgical wound infection rates of 6%–12%, even in simple procedures such as the removal of a transyndesmal screw.
Persistence of symptoms (39.8%): result expected by the surgeon/perceived patient resultWhen making an indication for the extraction of osteosynthesis material of a consolidated fracture, it is important to consider the degree of improvement the patient is going to experience. At present there is still no action plan based on the literature, since clinical and functional results after the OME are highly variable. Results in similar studies may range from an improvement of 50%–100%.5,33,34
Patients who present with a clear compromise of soft tissues as a consequence of the material (cerclage screws of the patella or the olecranon, clavicle fracture….) would probably experience relief of symptoms.35,36
In the case of extraction of material of an internal attachment with plates in ankle fractures, Brown et al.37 referred to several rates of improvement of lateral pain of the ankle to 50%. Better results were obtained by Pot et al.38 and Jacobsen et al.,39 with reduction of pain in 71% and 75%. It should be noted that this leaves a substantial number of patients with persistence of pain.
In the case of tibial plateau plates, Garner40 found there were better clinical outcomes in patients when the plates had been removed, and therefore recommended their removal in patients who were unhappy with the functional outcome of their knee.
In the case of intramedullary femur and tibia nails, improvement of pain is unpredictable. On the one hand, in a retrospective study in a series of 80 patients with a femoral fracture, Dodenhoff et al.41 described an improvement in only 11 patients of 17 whose implant had been extracted. In 2004, in a study of 109 patients, Gosling et al.42 stated that of the 58 patients with previous pain, in 78% the discomfort improved and in 7% it worsened. Of the 51 asymptomatic patients, in up to 20% the clinical symptoms got worse. For this reason, extraction of implants in asymptomatic patients is never recommended. Toms et al.43 recommended removal in the case of persistence of pain based on a series of 34 patients where the improvement was 100%.
In tibia implants, knee pain is one of the main indications for material extraction. In this case, the literature also describes variable results, with an improvement of pain in the knee between 72% and 96% (Keating et al.,44 Court-Brown45 and Sidky et al.46). However, other authors describe improvements in only 55% (Boerger et al.47 and Karladani et al.48), and 25% of patients who were previously asymptomatic and who develop knee pain.
It is also important to think that a percentage of cases which improve after OME may be related to low grade infections. In patients with intramedullary implants who present with unwarranted pain, or in the case of a history of open fractures, implant infection and wound infection is more common, and nail sonication may help to diagnose implant colonization which may require specific treatment.49,50 Esteban et al.49 stated that a subclinical infection or a low grade infection cannot be ruled out unless the implant is extracted and sonicated. In their series, all the patients with positive implant cultures improved their symptoms, whilst in those where cultures were negative, 1/3 did not improve, thus relating the low grade infection with the pain unexplained by other causes. Furthermore, they found there was a significant relationship between positive cultures after sonication and previous local superficial infection.
Study limitations: this study has several limitations. Firstly, it is a survey which only describes the opinions and practices of some surgeons from different hospitals, which does not constitute operational standards. The questionnaires may be regarded as biased by decisions or complications from recent medical cases. Although the results from this study do not provide action guidelines regarding the extraction of material in a consolidated fracture, they do provide information to the surgeon performing the operation, to advise the patient about the expected clinical outcome, and the intra and postoperative complications which may occur.
To conclude, in the case of discomfort, OME does not ensure an improvement in pain but it may suggest an indication for extraction if no other cause for pain may be found. Given that improvement in pain is variable, the surgeon should cautiously indicate extraction, especially in the asymptomatic patient, warning them that there is no guarantee that the pain will improve and that it could even get worse.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors wish to thank the AOTrauma España for their collaboration in distributing the survey. They would also like to thank Dr. Juan Antonio Alonso del Olmo, MSc, FRCS (Tr⩔th), Orthopaedic and Traumatology Surgery Service of the Hospital Clínico Universitario de Valladolid, Spain for his critical reading and comments which helped to optimise the manuscript.
Please cite this article as: Mingo-Robinet J, Pérez Aguilar M. Retirada de material de osteosíntesis: resultados de encuesta sobre indicaciones y prácticas de los cirujanos ortopédicos en España. Rev Esp Cir Ortop Traumatol. 2021;65:331–339.