To compare the mechanical failure of the Dresden technique for Achilles tendon repair with the double modified Kessler technique controlled repair technique. The maximum resistance of the two repair techniques are also compared.
Material and methodsA total of 30 Achilles tendon ruptures in bovine specimens were repaired with an Ethibond® suture to 4.5cm from the calcaneal insertion. Each rupture was randomly distributed into one of two surgical groups. After repair, each specimen was subjected to a maximum traction test. The mechanical failure (tendon, suture, or knot) rates (proportions) were compared using the exact Fisher test (α=.05), and the maximum resistances using the Student t test (α=.05).
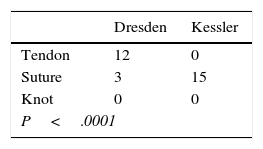
ResultsThere was a difference in the proportions of mechanical failures, with the most frequent being a tendon tear in the Dresden technique, and a rupture of the suture in the Kessler technique.
DiscussionThe repair using the Dresden technique performed in the open mode, compared to the Kessler technique, has a more suitable mechanical design for the repair of middle third Achilles tendon ruptures on developing a higher tensile resistance in 58.7%. However, its most common mechanical failure was a tendon tear, which due to inappropriate loads could lead to lengthening of the Achilles tendon.
Comparar el fallo mecánico de la técnica Dresden para la reparación del tendón de Aquiles respecto a la técnica de reparación control Kessler doble modificada. Secundariamente, comparar la resistencia máxima de la técnica de reparación Dresden respecto a la técnica de reparación control Kessler doble modificada.
Material y métodosUn total de 30 roturas de tendón de Aquiles en especímenes bovinos fueron reparadas con sutura Ethibond® a 4,5cm desde la inserción calcánea. Cada rotura fue distribuida de modo aleatorio en uno de 2 grupos quirúrgicos. Una vez reparadas, cada espécimen se sometió a una prueba de tracción máxima. Mediante una prueba exacta de Fisher (α=0,05) se compararon las tasas (proporciones) de fallo mecánico (tendón, sutura o nudo), y mediante una prueba t de Student (α=0,05), las resistencias máximas.
ResultadosLas proporciones de fallo mecánico entre las reparaciones fueron diferentes, siendo el fallo mecánico más frecuente el desgarro del tendón en la técnica Dresden y la rotura de la sutura en la técnica Kessler. La reparación Dresden desarrolló 245,4N y la reparación Kessler desarrolló 154,6N.
DiscusiónLa reparación con técnica Dresden realizada de modo abierto respecto a la técnica Kessler posee un diseño mecánico más apropiado para la reparación de roturas de tercio medio del tendón de Aquiles al desarrollar mayor resistencia tensil en un 58,7%. No obstante, su fallo mecánico más frecuente fue el desagarro tendinoso, que frente a cargas inapropiadas puede favorecer el alargamiento del tendón de Aquiles.
Rupture of the middle third of the Achilles tendon has an incidence of 18 cases per 100,000 inhabitants-year, and it mainly affects amateur sportsmen aged from 30 to 50 years old.1
It was traditionally repaired using open surgery and techniques such as those of Krackow, Kessler or Bunnell.2–8 Nevertheless, there is controversy as to whether the comorbidity associated with tissue damage following open surgical repair is greater than is the case with a percutaneous repair.9–12 There is also controversy as to whether the mechanical design of repair of the middle third of the tendon using a percutaneous procedure gives a suitable level of stability and rate of mechanical failure under traction.
A mechanically stable tendon repair technique is essential to guarantee suitable tendon connection after surgery. This is not always achieved naturally following rupture of the Achilles tendon, given the elastic retraction of the tendon ends. Additionally, suitable connection of the tendon makes it possible to re-establish its length at close to physiological values, while failure to ensure this may lead to future alterations in the relationship between the strength and length of the plantiflexor mechanism.13 On the other hand, a technique which leads to inappropriate failure such as failure of the tendon does not guarantee that the supporting points of the suture on the tendon (the tendon-suture interface) will not lead to structural damage under traction and secondarily lead to a change in the length of the tendon. Mechanical designs differ in this respect, as they favour suture deformation so that it generates more tensile dissipation.
The Dresden percutaneous repair technique as described by Amlang et al.9,10 has been described as giving positive clinical results.9,10,14 Other authors have also found similar clinical advantages in the use of this technique.15,16 Its main characteristics in comparison with open surgical techniques are a reduced sural nerve lesion and a low level of re-rupture due to the preservation of the paratendon, tissue which plays an important role in the tendon repair process.9,10,14
Nevertheless, it is not known whether the Dresden technique is a suitable mechanical alternative of choice for the repair of ruptures of the middle third of the Achilles tendon, as opposed to the techniques which are usually used. These include the double modified Kessler repair,17 which has proven to be a frequently chosen technique thanks to its suitable levels of tensile strength,3,5 its reproducibility, the fact that it has fewer negative effects on tendon microcirculation and that it is less invasive than other open techniques.3 Our aim is therefore to compare the mechanical failure rate of the Dresden technique for Achilles tendon repair to the double modified Kessler control technique. Secondarily, our objective is to compare the maximum strength of the Dresden repair technique to that of the double modified Kessler control technique. Our hypotheses are: (1) That the Dresden and double modified Kessler techniques give rise to equal mechanical failure rates due to traction, and (2) that the Dresden and double modified Kessler repairs have the same tensile strength against traction.
Material and methodStudy designAn experimental – comparative study was conducted from June 2014 to June 2015 in the biomechanical unit of the “Instituto Traumatológico Teodoro Gebauer Weisser” (Santiago, Chile). This study was approved by the Ethics Committee of the “Instituto Traumatológico Teodoro Gebauer Weisser” (Santiago, Chile).
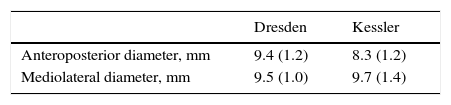
SpecimensA total of 30 ruptured Achilles tendons in bovine specimens (Table 1) were obtained from animals under the age of 2 years old and frozen at −18°C during the first 24h after sacrifice. Each piece was unfrozen at random by remaining in a defrosting room at ambient temperature during 12h before the biomechanical test was performed.
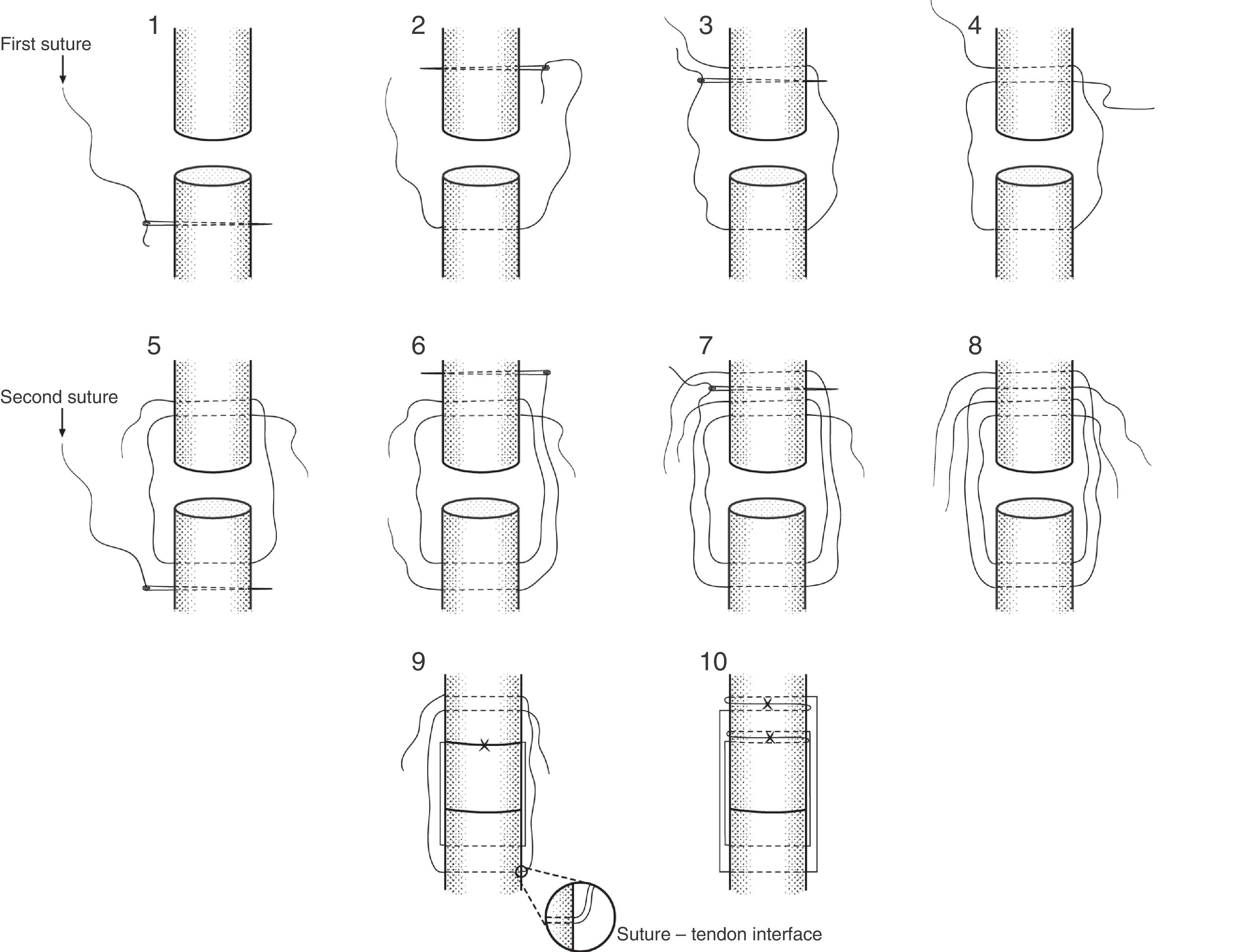
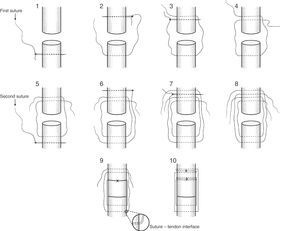
ProcedureEach specimen was dissected until the whole Achilles tendon was exposed (Fig. 1). The Achilles tendon was then completely ruptured at 4.5cm from the calcaneus bony prominence by making a cut with a number 21 scalpel perpendicular to the fibres, with the aim of simulating a rupture in its middle third. A Dresden tenorrhaphy was then performed at random under the repair principles described by Amlang et al.9,10 or the double modified Kessler procedure according to Sebastin et al.17 (Fig. 1), using Ethibond Excel® no. 1 braided synthetic non-absorbable suture (Ethicon endo-surgery Inc., Somerville, U.S.A.).
The Dresden technique was performed in open mode, with symmetrical points of support and balanced on the body of the Achilles tendon (Fig. 2). The experimental design included a first suture using a straight needle that passed through the central part of the Achilles tendon from the medial to the lateral plane at a distance of 1cm distally from the rupture. The same suture immediately passed through from the lateral to the medial plane at 0.8cm from the rupture and the free thread passed through from the lateral to the medial plane of the central part of the Achilles tendon and the free thread passed through from the lateral to the medial plane in the central part of the Achilles tendon at 1.0cm from the rupture. Subsequently a second suture using a second straight needle passed through from the medial plane to the lateral plane in the central part of the Achilles tendon, parallel to the first suture at a distance of 1.5cm distally to the rupture. This second suture immediately passed through from the lateral to the medial plane at 1.3cm from the rupture and the free thread passed through from the lateral plane to the medial plane in the central part of the Achilles tendon, at 1.5cm from the rupture. Once the sutures had passed through the tendon, the first suture was tensed until the tendon ends had connected termino-terminal, creating a first double knot followed by 5 simple knots. The second suture was immediately tensed and checked to ensure that the ends of the tendon connected in termino-terminal mode, ending with a first double knot followed by 5 simple knots, as shown in Fig. 2.
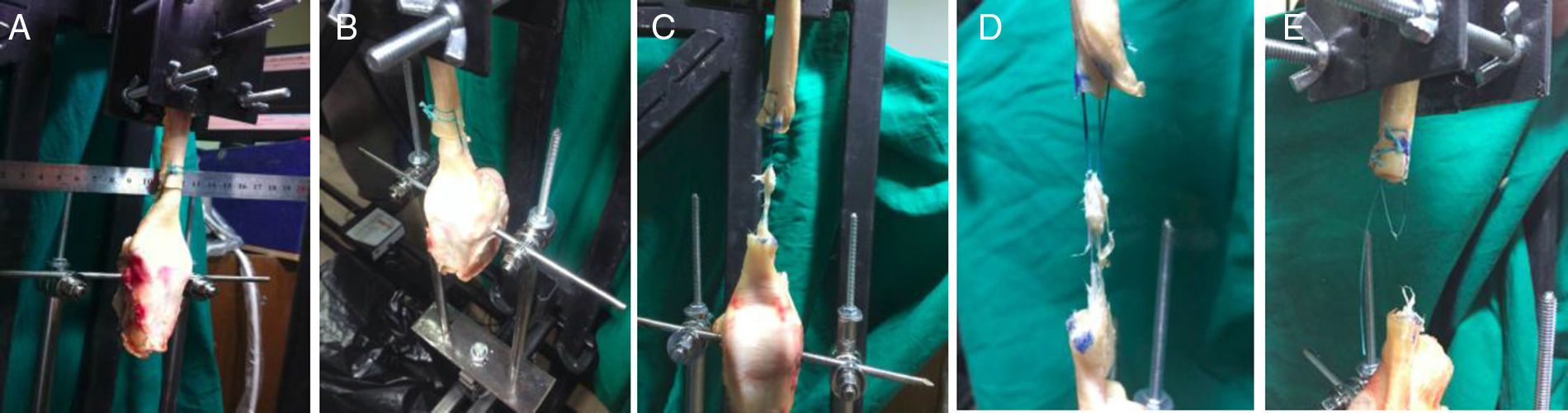
Biomechanical testEach specimen was mounted in a traction mechanism (Fig. 3) where it was subjected to a maximum traction test at 6mm/s.18 The mechanism was composed of the 7000N device (Linear ActuatorWorld, China) controlled by Matlab7.1 software (Mathworks Inc., U.S.A.). A toothed compressive clamp was placed at the distal end of the device (Fig. 3) to hold the proximal part of the tendon end.3 The bone (distal) end of the specimen was attached to a power sensor (RevereTransducer Inc., U.S.A.) using a 5mm surgical steel nail to obtain the strength data. The latter were acquired at a rate of 1000 data per second and stored in a in a matrix of strength and time×samples.
MeasurementsBefore performing the biomechanical test the anteroposterior and mediolateral diameter in the rupture zone was recorded (Table 1) using a slide gauge with a precision of 0.01mm.
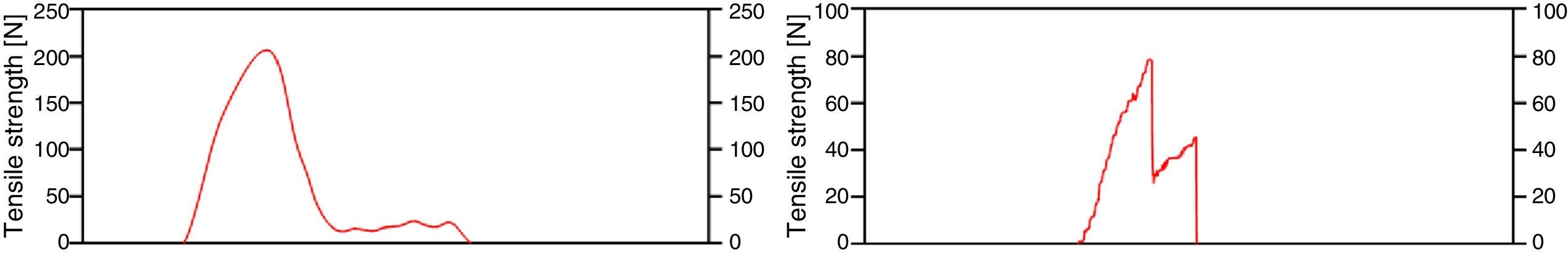
For the maximum traction test the load-time curve was recorded for each specimen (Fig. 4), obtaining the maximum resistance variable (peak force). The mechanical failure variable was categorised as knot if there was knot failure, suture if the suture tore or tendon if the tendon ruptured in the first drop in maximum resistance in the load – time curve (Fig. 4).
Data analysisThe data were described using the arithmetic mean and standard deviation. Data normality was then checked using the Shapiro–Wilk test. To compare the proportions of mechanical failure a 3×2 contingency table was created and Fisher's exact test was used with 2 tails and type I error of 5%. To compare the arithmetic means of the maximum strengths a 2 tail Student's t-test was used with a type I error of 5%. All statistical calculations were developed using STATA 12 software (StataCorp LP, Texas, U.S.A.).
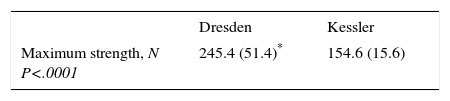
ResultsThe data presented a normal distribution (P>.05). The tendon characteristics prior to the biomechanical test are shown in Table 1. The proportions of mechanical failure of the repairs area shown in Table 2, and the most frequent was tearing of the tendon for the Dresden technique and rupture of the suture for the Kessler technique. Finally, the results obtained in the maximum traction tests are shown in Table 3, in which the Dresden repair attained a strength 58.7% greater than the Kessler repair.
Maximum strength of the repairs.
| Dresden | Kessler | |
|---|---|---|
| Maximum strength, N P<.0001 | 245.4 (51.4)* | 154.6 (15.6) |
In spite of the enormous range of Achilles tendon repair techniques19 and the secondary comorbidities following open repairs, there is still a lack of knowledge about whether the new techniques with positive clinical results developed over recent years, such as the Dresden repair9,10,14–16 have a suitable mechanical design to withstand tensile loads in comparison with other repairs that had proven successful in the past from a mechanical point of view. Our study therefore compared the proportion of mechanical failures with the Dresden technique in comparison with the double modified Kessler control repair technique. Additionally and secondarily the maximum strength of the Dresden repair technique was compared to that of the double modified Kessler control repair.
Our main finding was the difference in proportions of mechanical failure between the repairs, as tendon tear was the most frequent failure mechanism in the Dresden repair, while rupture of the suture was the most frequent mechanism for the Kessler repair. Secondarily, our study found that the Dresden technique gives a higher tensile strength than the Kessler technique. These results suggest that stress is dissipated better over the suture threads in the Dresden repair combined with the suture-tendon interface (Fig. 2). This makes it possible to create greater tensile strength than is the case in the Kessler repair, which, given the results, seems to have reached the maximum permissible deformation of one of its sutures, leading to its tearing early in comparison with the Dresden repair, as is shown by the double sawtooth pattern in Fig. 3. Nevertheless, the greater strength of the Dresden technique is accompanied by structural damage to the tendon (Fig. 5) to the degree in which it reaches the region of non-proportional plastic behaviour, as is denoted by the smoothed pattern of Fig. 3, where it may lead to increased tendon length13 before causing a repeat rupture, unlike the Kessler repair. This phenomenon suggests that use of the Dresden technique in combination with tensile loads applied unsuitably, as may occur during early rehabilitation,13,20 could cause silent changes in tendon length during rehabilitation and leading to reduced plantiflexor efficiency of the gastrosoleus mechanism13 in spite of the higher strength of the mechanical design of the Dresden repair. On the other hand, use of the double modified Kessler technique suggests that, in combination with unsuitable tensile loads, re-rupture may occur at loads 58.7% lower than is the case for the Dresden repair, leading to plastic deformation predominantly of the sutures, unlike the Dresden technique. This suggests that there is more damage to the tendon in the Dresden technique, in the form of repeat rupture caused by tensile loads (Fig. 5).
Studies undertaken in finger flexor tendons suggest that one of the most important factors for tensile strength is the number of sutures which pass between the 2 ends of the tendon, together with surgical technique.21–23 Due to this, an increase in the threads used for the Dresden repair may give rise to better stress distribution. This could be a way of preventing tendon lengthening phenomena during early rehabilitation, together with damage caused by stress concentration at the tendon-suture interface and repeat rupture; nevertheless, this would have to be checked by future studies. On the other hand, an asymmetrical load on the sutures leads to worse control of the tensile balance, as the results with the Kessler repair suggest. However, this study has only compared both repairs in open mode, and it is not known whether a percutaneous Dresden repair has a negative effect on the type of failure and mechanical resistance, so that new research would be needed to explore the said effect.
The literature reports maximum values for the Dresden repair using 628N Fiberwire 2.0 suture (Arthrex, Naples, U.S.A.),24 and for the Kessler repair when 137N PDS-1 is used (Ethicon endo-surgery Inc., Somerville, U.S.A.).5 This contrasts with our results, and it is interesting that the type of suture material used affects obtaining the maximum strength, as is shown in the literature when it describes the results of using the same technique with different suture materials.5
Finally, in spite of the continuing lack of agreement on the optimum procedure following the acute rupture of the middle third of the Achilles tendon,14,20,25,26 our research suggests that repair using the Dresden technique in open mode is a more suitable mechanical design than the double modified Kessler technique for traction.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed are according to the ethical regulations of the responsible human experimentation ethics committee, and that they are also according to the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their centre of work governing the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflicts of interestThe authors have no conflict of interests to declare.
Please cite this article as: de la Fuente C, Carreño-Zillmann G, Marambio H, Henríquez H. ¿Es la técnica Dresden un diseño mecánico de elección apropiado para la reparación de roturas de tercio medio del tendón de Aquiles? Ensayo biomecánico. Rev Esp Cir Ortop Traumatol. 2016;60:279–285.