To compare medium- and long-term postoperative surgical results, especially the adjacent syndrome rate, adverse event rate, and reoperation rate, of patients operated on with cervical arthroplasty or anterior cervical arthrodesis in published randomized clinical trials (RCTs), at one cervical level.
MethodsSystematic review and meta-analysis. Thirteen RCTs were selected. The clinical, radiological and surgical results were analyzed, taking the adjacent syndrome rate and the reoperation rate as the primary objective of the study.
ResultsTwo thousand nine hundred and sixty three patients were analyzed. The cervical arthroplasty group showed a lower rate of superior adjacent syndrome (P<0.001), lower reoperation rate (P<0.001), less radicular pain (P=0.002), and a better score of neck disability index (P=0.02) and SF-36 physical component (P=0.01). No significant differences were found in the lower adjacent syndrome rate, adverse event rate, neck pain scale, or SF-36 mental component. A range of motion of 7.91° was also found at final follow-up, and a heterotopic ossification rate of 9.67% in patients with cervical arthroplasty.
ConclusionIn the medium and long-term follow-up, cervical arthroplasty showed a lower rate of superior adjacent syndrome and a lower rate of reoperation. No statistically significant differences were found in the rate of inferior adjacent syndrome or in the rate of adverse events.
Comparar a mediano y a largo plazo los resultados quirúrgicos postoperatorios, sobre todo la tasa del síndrome adyacente, la tasa de eventos adversos y la tasa de reoperación, de los pacientes operados con artroplastia cervical o artrodesis cervical anterior en los ensayos clínicos aleatorizados (ECA) publicados de un nivel cervical.
MétodosRevisión sistemática y metaanálisis. Se seleccionaron 13 ECA. Se analizaron los resultados clínicos, radiológicos y quirúrgicos, tomando como variables primarias la tasa del síndrome adyacente, la tasa de eventos adversos y la tasa de reoperación.
ResultadosFueron 2.963 los pacientes analizados. El grupo de artroplastia cervical mostró una menor tasa de síndrome adyacente superior (p<0,001), una menor tasa de reoperación (p<0,001), un menor dolor radicular (p=0,002) y una mejor puntuación en el índice de discapacidad cervical (p=0,02) y en el componente físico SF-36 (p=0,01). No se encontraron diferencias significativas en la tasa del síndrome adyacente inferior, en la tasa de eventos adversos, en el dolor cervical ni en el componente mental SF-36. En la artroplastia cervical se halló un rango de movilidad medio de 7,91 grados en el seguimiento final y una tasa de osificación heterotópica del 9,67%.
ConclusiónEn el seguimiento a mediano y a largo plazo, la artroplastia cervical mostró una menor tasa de síndrome adyacente superior y una menor tasa de reintervención. No se hallaron diferencias estadísticamente significativas en la tasa del síndrome adyacente inferior ni en la tasa de eventos adversos.
Ever since Robinson and Smith published the results of anterior cervical arthrodesis (ACA) in 1958, this has been the standard surgical procedure for the treatment of symptomatic cervical disc degenerative disease (CDDD).1 A recent study pointed out that 84.3% of spinal column surgeons use ACA as their standard surgical technique for CDDD.2 CDDD, which includes cervical discopathy and cervical hernias, is considered to be one of the chief causes of work disability.3,4 At the present time some studies describe an increasing tendency to use cervical surgery in the near future, above all in the population aged from 45 to 54 years old.4,5
Many studies have found ACA to be a successful procedure that offers excellent relief of the symptoms and significantly improves the quality of life.2,6,7 Nevertheless, it is also associated with certain complications, such as pseudoarthrosis, a lack of instrumentation and the adjacent segment syndrome. The latter may be one of the most important complications, as it leads to secondary surgery in the patients.2,8,9 As ACA creates solid bone fusion, it may change the range of movement and the mechanical load on adjacent segments, and this may cause adjacent segment disease or syndrome.8,9 Hilibrand et al. found that symptomatic adjacent segment syndrome affects more than one quarter of all patients within the 10 years after an ACA.10 Lee et al. found that after ACA secondary surgery in the adjacent segments occurred in a relatively constant proportion of 2.4% of patients per year (confidence interval (CI) 95%: 1.9–3.0).11
Cervical arthroplasty (CA) emerged in the 1990s to prevent the risks of a lack of fusion and adjacent syndrome, with the advantage of preserving physiological movement while maintaining the height of the disc and segmentary lordosis.12–15 Due to these advantages, CA has been increasingly used over recent years.5 However, CA also has certain disadvantages, the most common of which are implant failure and heterotopic ossification.16,17
Several previous meta-analyses compared the advantages and drawbacks of CA and ACA, mainly over a short-term follow-up periods (2 years).15,16,18 Few studies have analyzed their efficacy over the mid (5 year follow-up) or long term (more than 7 years of follow-up), and they found no fully conclusive results.19–23 One limitation of these meta-analyses is that they mix studies of patients operated at 1 and 2 cervical levels.15,16,18–22 Furthermore, previously published works3 as well as the latest randomized clinical trials (RCT) published with a 5 year follow-up24,25 found no advantages for CA in reducing the incidence of adjacent segment syndrome. Based on the hypothesis that it will be possible to detect differences between medium and long-term follow-up periods, this systematic review and meta-analysis aims to update and compare clinical, radiological and surgical results, above all in terms of adjacent segment syndrome, adverse events and the re-operation of patients operated using CA or ACA in RCT at a single cervical level.
Material and methodsLiterature search strategySystematic review and meta-analysis. This meta-analysis was undertaken following the stipulations of the declaration Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).26 The systematic review was carried out following the recommendations of the Manual Cochrane para Revisiones Sistemáticas de Intervenciones.27 An electronic search was performed in PubMed, EMBASE and the Cochrane Collaboration Library until 1 January 2023 for RCT that compared CA with ACA. The search strategy used the following key words in English and Spanish: “anterior cervical discectomy and fusion or artrodesis cervical anterior”, “ACDF or ACA”, “cervical disc arthroplasty or artroplastia cervical”, “CDA or CA”, “randomized control trial or ensayos clínicos aleatorizados”, or “RCT or ECA”. The bibliographical search was restricted to the English and Spanish languages. Additional strategies for the identification of studies included consultation with experts and the use of “associated papers” functions.
Inclusion criteriaThe inclusion criteria for study identification were as follows: (1) RCT which compare 2 surgical procedures (ACA and CA); (2) studies that compare surgery at a single cervical level; (3) with a follow-up time of at least 60 months; and (4) studies which report on at least one result associated with the variables studied. The meta-analysis excluded studies which (1) lacked comparative data, (2) had an insufficient follow-up time, (3) were biomechanical or in vitro, and (4) were presentations in conferences, editorials or summaries.
The selection of studiesTwo of the authors evaluated the eligibility of the search results. The complete text was read intensively when the results fulfilled the inclusion criteria. If any conflict arose between the 2 reviewers, a third reviewer was consulted to reach a decision.
Data extractionData were extracted from the main texts and the complementary appendices. Data were grouped in the following way: (1) general characteristics, such as the first author, year of publication, clinical trial number, patients included, age, sex, type of prosthesis, follow-up time and losses during follow-up; (2) the primary variables studied: superior adjacent syndrome, inferior adjacent syndrome and re-operation rate, (3) secondary variables studied: cervical disability index (CDI), cervical AVS, radicular AVS, 36 item short format health survey (SF-36) covering physical and mental aspects, rate of adverse events, rate of high grade heterotopic ossification and the range of movement of the operated cervical segment.
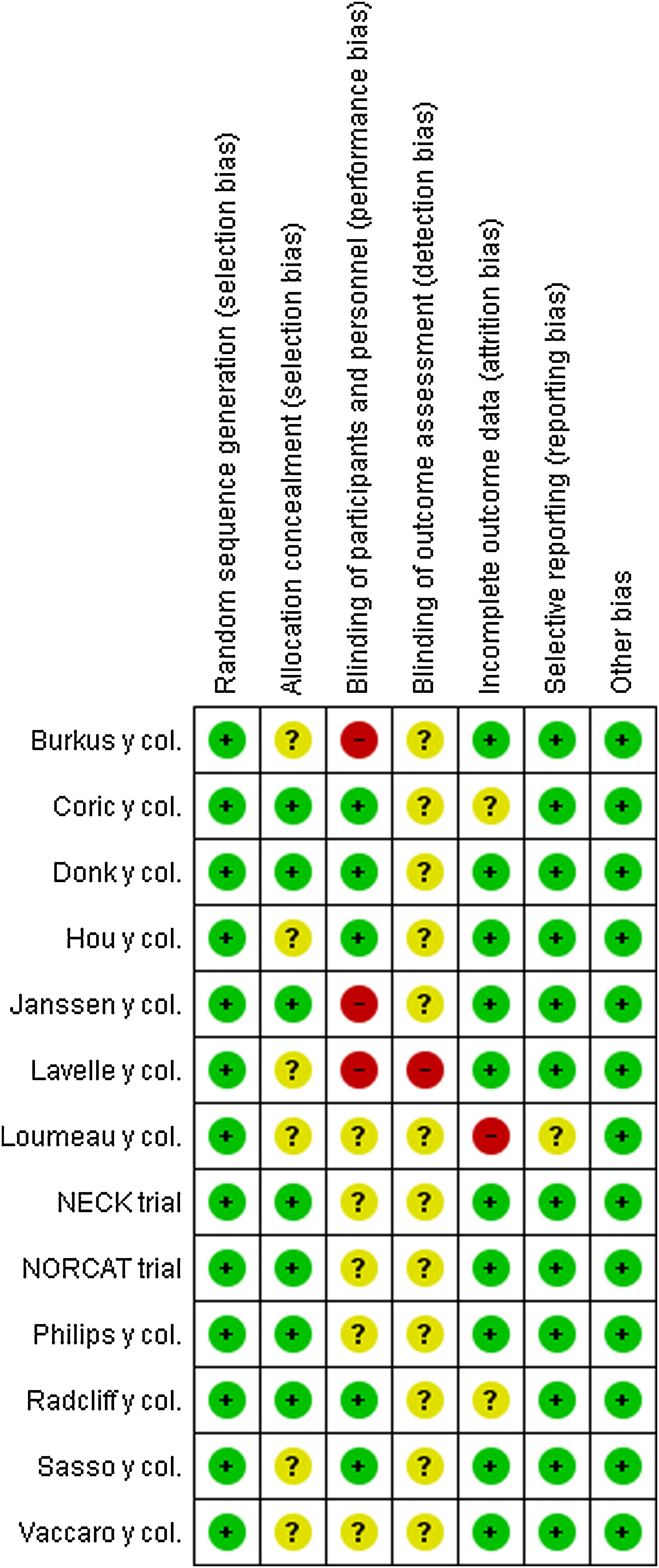
Quality evaluationThe quality of the RCT was assessed using version 5.3 of the Review Manager programme (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, 2014) to evaluate the risk of bias. The assessment methodology consisted of the following steps: generation of random sequences, hiding the assignation, blinding, incomplete result data and the selective reporting of results. Scores were analyzed in an evaluation of the general risk of bias for a RCT: 91) “low risk of bias”; 92) “some concerns”; or (3) “high risk of bias”.
Statistical analysisThe descriptive statistics used were the average and standard deviation (SD) for continuous variables, and distribution and percentage for categorical variables. The meta-analysis was performed using version 5.3 of the Cochrane Community Review Manager. The odds ratio (OR) was used to evaluate binary variables, while the average standard difference (ASD) was used for continuous variables, with a 95% CI. The heterogeneity of the studies was calculated using the I2 test. The random effects inverse variance model was applied. Statistical significance was defined as P<.05.
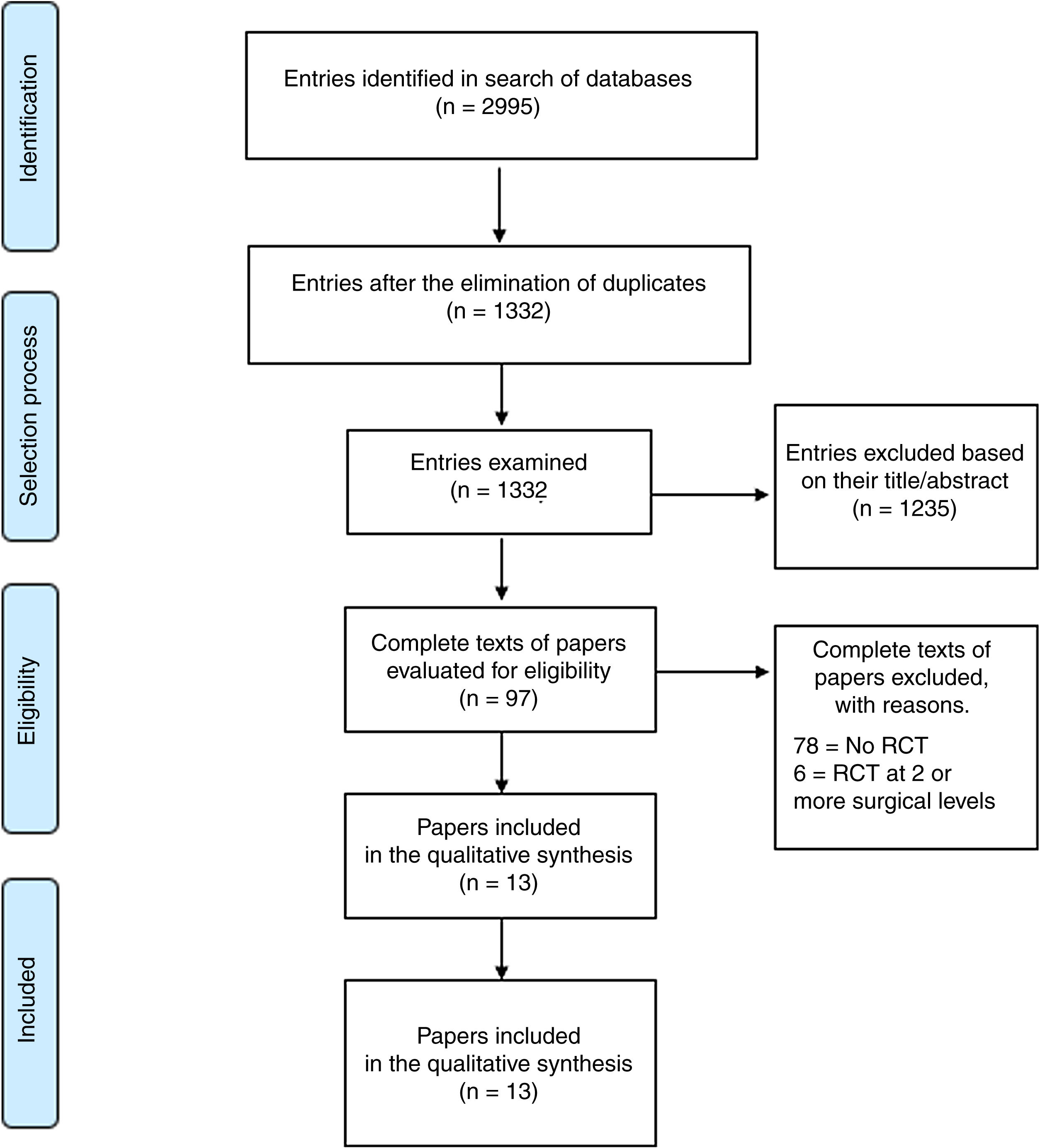
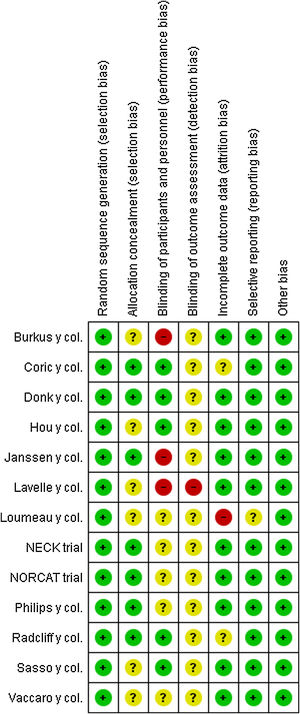
ResultsBibliographical reviewThe first search of the database identified 2995 papers (PubMed: 1508, Embase: 1031, and the Cochrane Collaboration Library: 384). The detailed selection of the bibliography is described in the flowchart of Fig. 1. A total of 1663 studies were eliminated because they were duplicated, 1235 studies were excluded due to their titles and abstracts, and 97 studies were eliminated because of other reasons. The final result was the identification of 13 studies.24,25,28–38Fig. 2 shows a summary of the risk of bias.
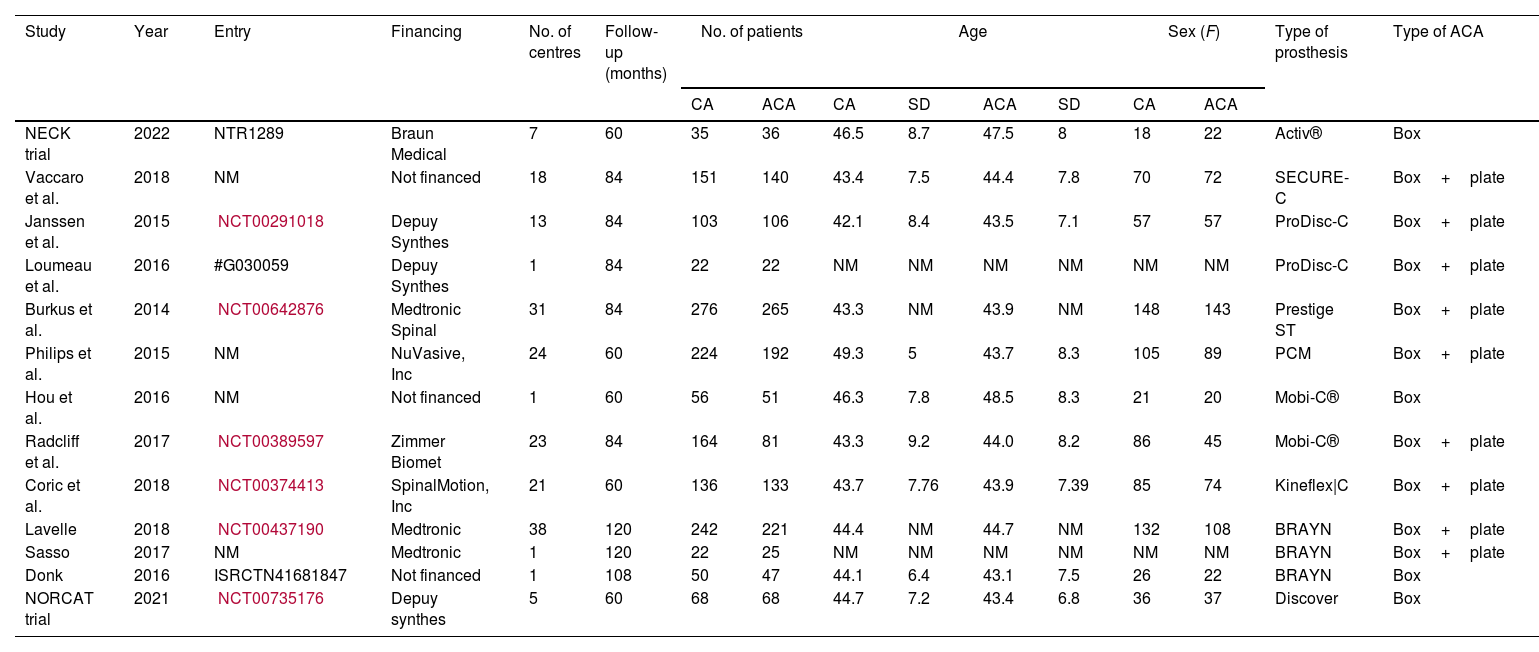
Table 1 shows the general characteristics of each study.24,25,28–38 The meta-analysis included a total of 2936 patients, with 1549 CA patients and 1387 ACA patients.24,25,28–38 Their average age was 44.2 years (SD 2.2) in the CA group and 44.7 years (SD 1.9) in the ACA group.24,25,28,29,32–34,37,38 52.1% of the CA group were women, as were 51.4% of the ACA group.24,25,28–30,32–34,36–38
Basal characteristics of the studies included in the meta-analysis.
| Study | Year | Entry | Financing | No. of centres | Follow-up (months) | No. of patients | Age | Sex (F) | Type of prosthesis | Type of ACA | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CA | ACA | CA | SD | ACA | SD | CA | ACA | ||||||||
| NECK trial | 2022 | NTR1289 | Braun Medical | 7 | 60 | 35 | 36 | 46.5 | 8.7 | 47.5 | 8 | 18 | 22 | Activ® | Box |
| Vaccaro et al. | 2018 | NM | Not financed | 18 | 84 | 151 | 140 | 43.4 | 7.5 | 44.4 | 7.8 | 70 | 72 | SECURE-C | Box+plate |
| Janssen et al. | 2015 | NCT00291018 | Depuy Synthes | 13 | 84 | 103 | 106 | 42.1 | 8.4 | 43.5 | 7.1 | 57 | 57 | ProDisc-C | Box+plate |
| Loumeau et al. | 2016 | #G030059 | Depuy Synthes | 1 | 84 | 22 | 22 | NM | NM | NM | NM | NM | NM | ProDisc-C | Box+plate |
| Burkus et al. | 2014 | NCT00642876 | Medtronic Spinal | 31 | 84 | 276 | 265 | 43.3 | NM | 43.9 | NM | 148 | 143 | Prestige ST | Box+plate |
| Philips et al. | 2015 | NM | NuVasive, Inc | 24 | 60 | 224 | 192 | 49.3 | 5 | 43.7 | 8.3 | 105 | 89 | PCM | Box+plate |
| Hou et al. | 2016 | NM | Not financed | 1 | 60 | 56 | 51 | 46.3 | 7.8 | 48.5 | 8.3 | 21 | 20 | Mobi-C® | Box |
| Radcliff et al. | 2017 | NCT00389597 | Zimmer Biomet | 23 | 84 | 164 | 81 | 43.3 | 9.2 | 44.0 | 8.2 | 86 | 45 | Mobi-C® | Box+plate |
| Coric et al. | 2018 | NCT00374413 | SpinalMotion, Inc | 21 | 60 | 136 | 133 | 43.7 | 7.76 | 43.9 | 7.39 | 85 | 74 | Kineflex|C | Box+plate |
| Lavelle | 2018 | NCT00437190 | Medtronic | 38 | 120 | 242 | 221 | 44.4 | NM | 44.7 | NM | 132 | 108 | BRAYN | Box+plate |
| Sasso | 2017 | NM | Medtronic | 1 | 120 | 22 | 25 | NM | NM | NM | NM | NM | NM | BRAYN | Box+plate |
| Donk | 2016 | ISRCTN41681847 | Not financed | 1 | 108 | 50 | 47 | 44.1 | 6.4 | 43.1 | 7.5 | 26 | 22 | BRAYN | Box |
| NORCAT trial | 2021 | NCT00735176 | Depuy synthes | 5 | 60 | 68 | 68 | 44.7 | 7.2 | 43.4 | 6.8 | 36 | 37 | Discover | Box |
CA: cervical arthroplasty; ACA: anterior cervical arthrodesis; SD: standard deviation; No.: number; NM: not mentioned.
Three studies used the BRYAN® cervical disc (Medtronic, Minneapolis, MN, U.S.A.),30–32 2 studies used the ProDisc-C® cervical disc (Depuy-Synthes Spine, Raynham, MA, U.S.A.),34,35 2 studies used the Mobi-C® cervical disc (Zimmer Biomet, Varsovia, IN, U.S.A.)28,38 and each one of the other 6 studies used a different model of CA.24,25,29,33,36,37 There were also differences in the type of ACA used; 4 studies used boxes without plates,24,25,32,38 while the remaining 9 studies used boxes with plates.28–31,33–37
Evaluation of biasFig. 2 shows the results of bias assessment. All 13 studies describe suitable methods of randomization24,25,28–38; 5 studies blinded the patients as well as the researchers.28–32,38 The demographic data on age and sex at the start of the study were similar in both treatment groups studied in all of the studies. All 13 studies contained descriptions of patient abandonment and withdrawal. Ten of the 13 studies were financed by the industry32,33,38 (Table 1).
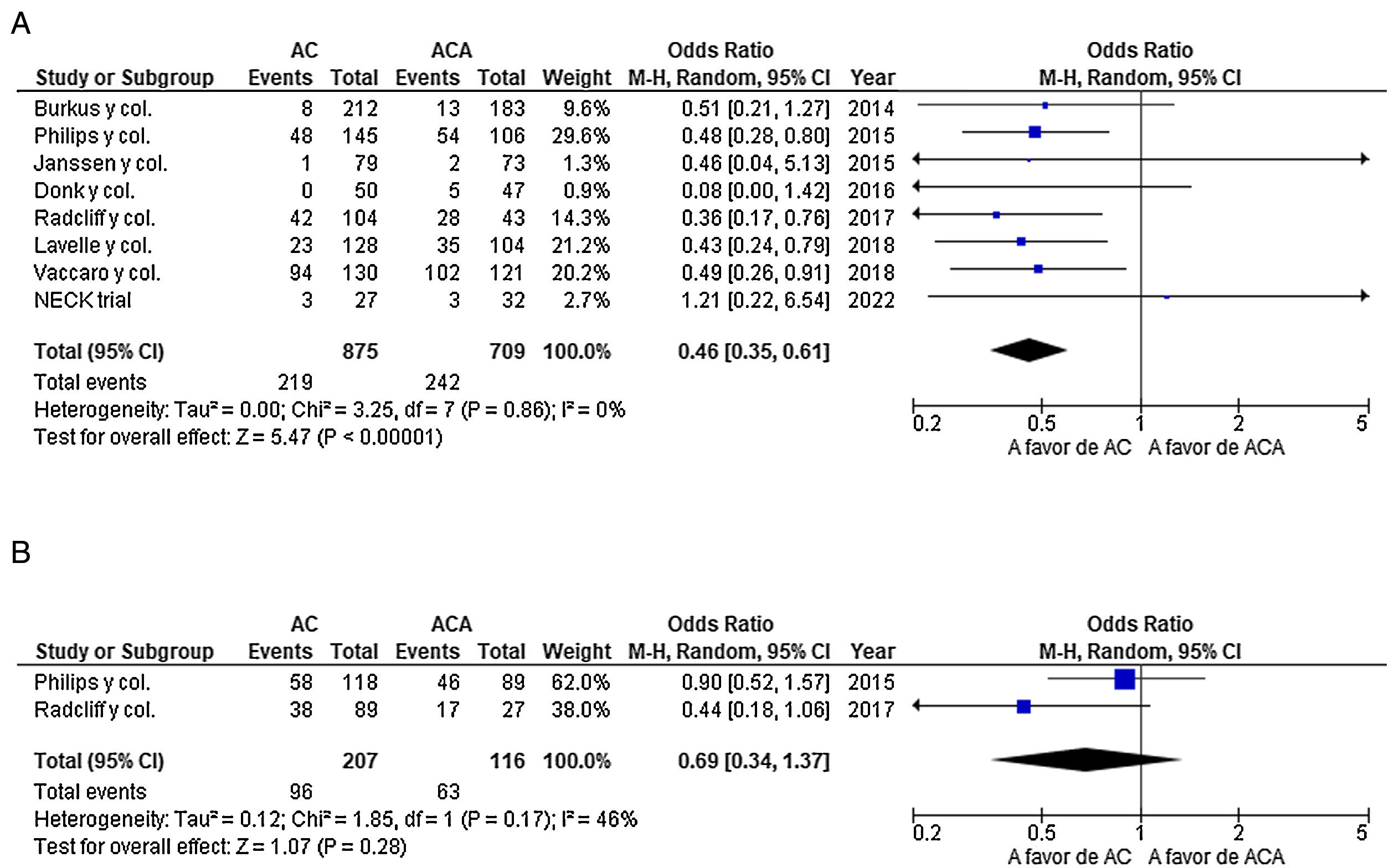
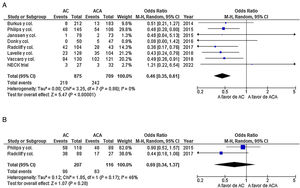
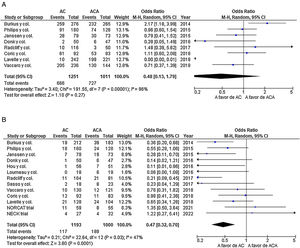
Primary objective results: superior adjacent syndrome, inferior adjacent syndrome, the adverse events rate and the re-operation rateEight studies reported on the incidence of superior adjacent syndrome.24,28,30,32–34,36,37 The overall results showed an incidence of superior adjacent syndrome that was significantly lower in the CA group (OR=0.49; 95% CI: 0.37–0.65; P<.001), with zero heterogeneity (I2=0%; P=.78) (Fig. 3a). Only two studies reported the incidence of inferior adjacent syndrome.28,37 No statistically significant differences were found in the results as a whole between both groups in terms of the incidence of inferior adjacent syndrome (OR=0.70; 95% CI: 0.34–1.44; P=.33), with a moderate level of heterogeneity (I2=53%; P=.14) (Fig. 3b).
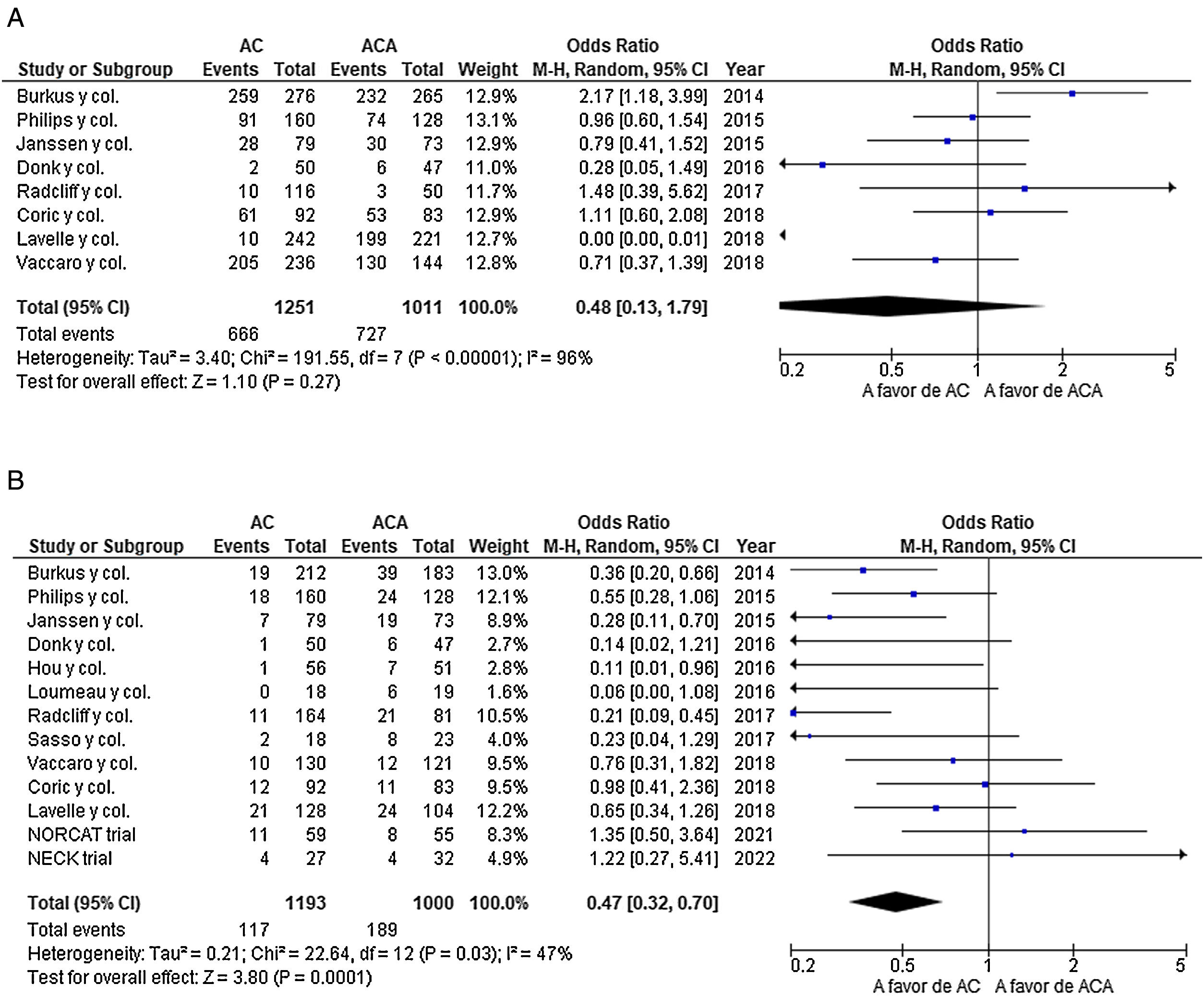
No differences were found in the incidence of adverse events (OR=0.70; 95% CI: 0.34–1.44; P=.33), with a moderate level of heterogeneity (I2=53%; P=.14) (Fig. 4a). Nevertheless, a significantly higher incidence of re-operation was found in the ACA group (OR=0.47; 95% CI: 0.32–0.70; P<.001), with a moderate level of heterogeneity (I2=47%; P=.03) (Fig. 4b).
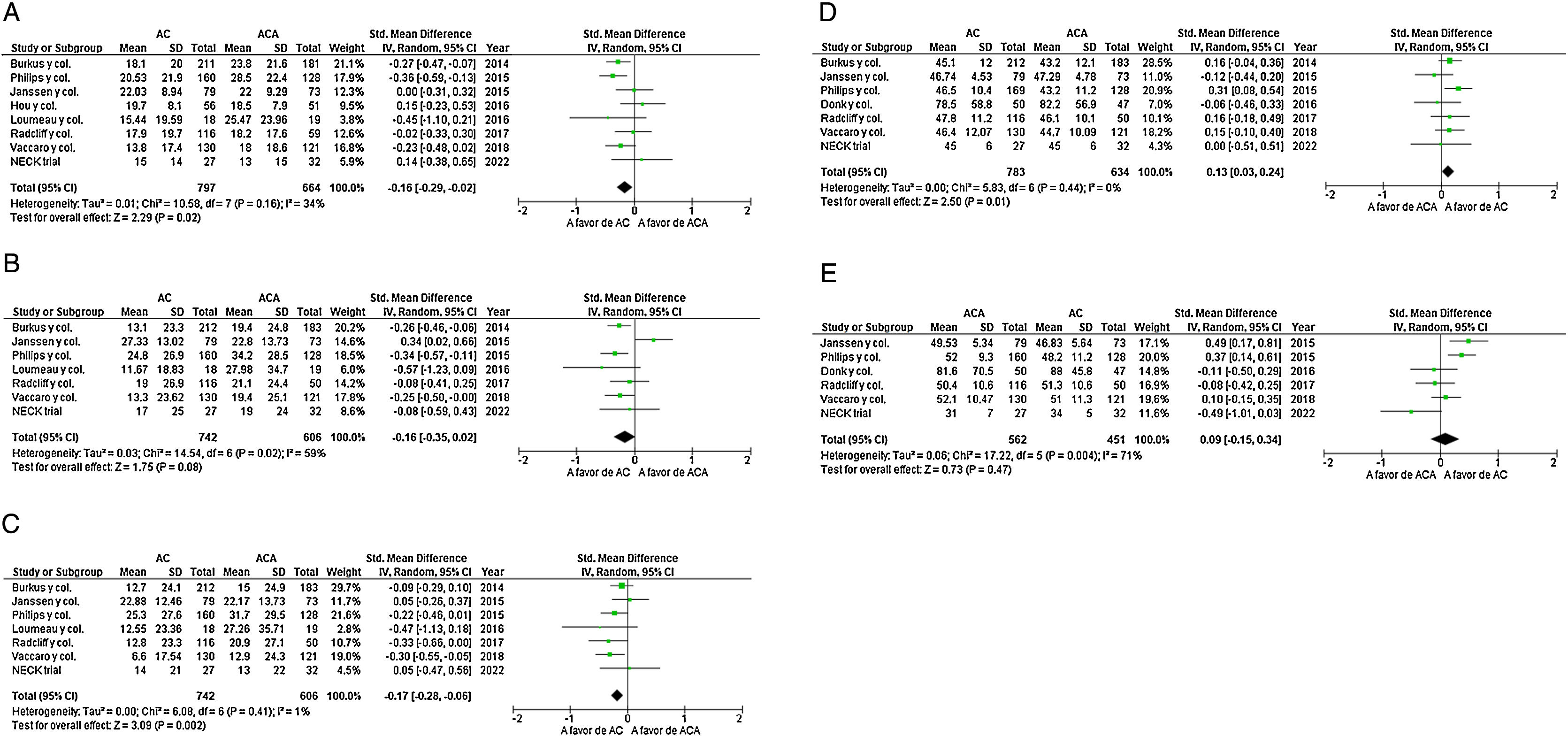
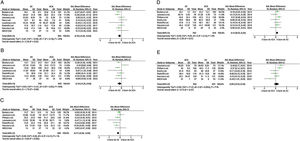
Secondary objective results: cervical disability index, cervical AVS, radicular AVS, mental and physical components of the SF-36, heterotopic ossification rate and range of movementEight studies identified CDI data. They included 797 patients in the CA group and 664 patients in the ACA group.24,28,33–38 Significant differences in favour of CA were found in the CDI (ASD=−0.16; 95% CI: −0.29 to −0.02; P=.02), with a moderate level of heterogeneity (I2=34%; P=0.16) (Fig. 5a). Cervical and radicular AVS was analyzed in 7 studies, with 742 patients in the CA group and 606 patients in the ACA group.24,28,33–37 The overall results showed no significant differences in terms of cervical AVS between both groups (ASD=−0.16; 95% CI: −0.35–0.02; P=.08) with a moderate level of heterogeneity (I2=59%; P=.02) (Fig. 5b). However, significant differences were found in favour of the CA group in radicular AVS (ASD=−0.17; 95% CI: −0.28 to −0.06; P=.002), with a slight degree of heterogeneity (I2=1%; P=.41) (Fig. 5c).
(a) Forest plot of the cervical disability index (CDI). (b) Forest plot of cervical AVS. (c) Forest plot of radicular AVS. (d) Forest plot of the SF-36 physical component. (e) Forest plot of the SF-36 mental component. ACA: anterior cervical arthrodesis; ASD: average standard deviation; AVS: analogue visual scale; CA: cervical arthroplasty; CDI: cervical disability index; 95% CI: 95% confidence interval.
Respecting the 36 item short form health questionnaire (SF-36) (which covers physical and mental aspects), 7 studies included analysis of the physical aspects24,28,32–34,36,37 and 6 studies included analysis of the mental aspects.24,28,32–34,37 The overall results showed that the physical component of the SF-36 significantly favoured the CA group (ASD=0.13; 95% CI: 0.03–0.24; P=.01) with zero heterogeneity (I2=0%; P=.44) (Fig. 5d). No significant differences were found between both groups in terms of the SF-36 mental component (ASD=0.09; 95% CI: −0.15 to 0.34; P=.47), with a moderate degree of heterogeneity (I2=71%; P=.004) (Fig. 5e).
A 9.67% rate of high-grade heterotopic ossification was found in the group of CA patients.28,29,33–38 (Appendix A, Annex 1a). The total results indicate that there is a significantly higher rate of movement in the CA group in the operated segment (ASD=2.97; 95% CI: 1.77–4.17; P<.001), with a severe level of heterogeneity (I2=97%; P<.001) (Appendix A, Annex 1b).28,34,37,38 Follow-up of the degree of movement at the level with CA showed 7.91 (SD 1.9)28–30,33–38 (Appendix A, Annex 1a).
DiscussionNumerous meta-analyses in recent years have compared the clinical and radiological results of ACA and CA with the aim of finding the advantages and drawbacks of each one. The majority of the results of these studies are not conclusive,15,16,18 and they mix patients with different numbers of operated cervical levels.19–22 Our aim in this systematic review and meta-analysis was to compare clinical, radiological and surgical results over the medium and long term. Especial emphasis was placed on the adjacent syndrome, adverse events and the re-operation of patients operated at a cervical level using CA or ACA in published RCT. Our main findings were that with a follow-up of at least 5 years, CA had a lower rate of superior adjacent syndrome, a lower re-operation rate, a higher CDI score, less radicular AVS and a higher score for the SF-36 physical component. No significant different were found in the rate of inferior adjacent syndrome, the adverse events rate, the cervical pain scale or the mental component of SF-36. Other findings in the CA group were a range of mobility of 7.91° at the end of follow-up and a heterotopic ossification rate of 9.67%.
Our study found higher superior adjacent syndrome and re-operation rates in the ACA group. The lower adjacent syndrome and re-operation rates is a constant finding in the meta-analyses39–41 and RCT published beforehand28–38; nevertheless, the last two RCT published with a follow-up longer than 5 years find differently, above all in the adjacent syndrome rate.24,25 In their meta-analysis Luo et al. found that CA had a significantly lower incidence of superior adjacent syndrome (OR=0.57; 95% CI: 0.44–0.73; P<.00001) together with a significantly lower incidence of re-operation (OR=0.50; 95% CI: 0.37–0.68; P<.00001).39 Dong et al. also found a significantly lower rate of adjacent syndrome in the CA group in comparison with the ACA group (P<.01) and that the advantage of CA in reducing re-operation of the adjacent syndrome increased over the follow-up time (P<.01).40 Wang et al. also found a lower rate of adjacent syndrome (OR=0.46; 95% CI: 0.34–0.64; P<.00001) and re-operation (OR=0.50; 95% CI: 0.29–0.87; P=.01) in the AC group.41 Nevertheless, the RCT NECKtrial reported a higher re-operation rate in the ACA group (P=.32), although it also reported the same rate of adjacent syndrome (P=.32)24 while the NORCAT RCT found no differences in the re-operation rate (P=.61) or the rate of adjacent syndrome (P=.32).25 The fact that their small sample size was a limitation in both of these studies should be taken into account,24,25 with fewer than 60 patients per CA or ACA group, and they even had a statistical power of only 80%.25 However, their differentiating strength in comparison with other RCT studied28,33–37 is that an intersomatic box was used in the ACA group without adding a fixing plate.24,25 A recent systematic review discussed whether the prevalence of adjacent syndrome degeneration in ACA is described as more common in U.S.A. papers, these being the majority of the studies analyzed in this meta-analysis.28–31,33–37 This is because in the U.S.A. cervical plates are frequently used, while in Europe plate-free ACA is more common. The latter was used in the NECKtrial24 and NORCAT25 studies, and the conclusion was that there is no answer to this question at the present time.42
There is currently debate about whether superior adjacent syndrome arises in ACA as a consequence of the restriction of movement.23–25. The greater range of movement in CA which remains during follow-up over the medium to long term is a constant finding in the RCT and other meta-analyses, showing that CA movement persists over time.22,28–30,33–38,41 Our study found a range of movement in the CA group of 7.91° at the end of the follow-up, and a heterotopic ossification rate of 9.67%. The percentage of heterotopic ossification is important, as it has been reported that the incidence of cervical adjacent syndrome is significantly higher in patients with high grade heterotopic ossification than it is in those where this is not present (22.73% vs 11.14%; P=.048).43 The inferior adjacent syndrome was harder to evaluate, given that few studies assess it separately; in our study only 2 RCT evaluate it, and they found no statistically significant differences.28,37
In the CA group, our study found a lower rate of adverse events, together with a higher CDI score, less radicular AVS and a higher physical component SF-36 score. No significant differences were found between both groups in the rate of adverse events, the cervical pain score or the mental component of the SF-36 score. The results in terms of adverse events are consistent with those of previous studies.21,22,44 The results of the secondary variables studied are similar to some other meta-analyses14,15,45; nevertheless, they differ from those of other meta-analyses, such as the ones by Luo et al.46 and Gao et al.,7 who found less cervical and radicular AVS in the CA group (P<.05) and a similar CDI in both groups (P>.05). In their meta-analysis Gendreu et al. found no statistically significant difference between the CDI (P=.37), cervical AVS (P=.79) or radicular AVS (P=.66) between both groups.20 Zhang et al. found that in the short and medium term follow-up patients treated using CA had a better CDI score and lower scores for cervical and radicular AVS.15 This discrepancy between results may be due to the heterogeneous nature of the groups.7,14–16,20,45,46 This result may indicate, as Zhang et al. pointed out, that different types of cervical arthroplasty differ in their efficacy.15 However, due to the limited number of RCT it is impossible to carry out an analysis of sub-groups stratified according to prosthesis type to evaluate the results separately. Most of the published RCT currently correspond to the BRYAN® (Medtronic, Minneapolis, MN, U.S.A.) cervical arthroplasty: 3 RCT.30–32
Certain limitations of this study should be taken into account. Firstly, it covers a small number of studies, which may lead an insufficient amount of data. Moreover, the studies included have methodological deficiencies, most commonly the lack of references about the blinding technique used. Furthermore, 10 of the studies were sponsored by the industry, and this financing may be a potential source of bias. Secondly, as in all RCT, inclusion and exclusion are applied to determine which patients analyzed were suitable for CA or ACA. That is, patients who were suitable for an ACA who were not suitable for a CA were excluded, and this restricts these conclusions to a certain patient type. Thirdly, some results show a moderate level of heterogeneity (I2>40%), such as those for the inferior adjacent syndrome, the re-operation rate, cervical AVS and the mental component of the SF-36. Adverse events have a high level of heterogeneity (I2>75%), and this may lead to distortion. Fourthly, although the patients operated using CA or ACA had a CDDD, the intervention in both groups was not the same. Different types of CA were used in the studies analyzed and different implants with or without a cervical fixation plate were used in the ACA patients, as were different types of graft (autograft or allograft). All of these differences hinder the analysis of sub-groups stratified according to type of fusion so that results can be evaluated separately. We therefore believe that further high-quality studies are still required to verify our results. Lastly, this systematic review was not included in the PROSPERO register, as it took place prior to inclusion and PROSPERO does not permit the inclusion of systematic reviews carried out beforehand.
To conclude, for the treatment of CDDD in patients who are suitable for CA or ACA, CA was found over the medium to long term to be superior to ACA in terms of a lower rate of superior adjacent syndrome, a lower re-operation rate, a better CDI score, less radicular AVS and a better score for the SF-36 physical component. No significant differences were found in the rate of inferior adjacent syndrome, the adverse events rate, the cervical pain scale or the mental component of the SF-36.
Level of evidenceLevel of evidence i.
FinancingNo grant (economic support) was received from any institution for the preparation of this paper.
Conflict of interestsThe authors have no conflict of interests to declare.