Patellar osteochondral fractures with no dislocation are uncommon and usually affect the centromedial facet of the patella. We present the case of a 10-year-old, overweight, female patient. She was seen in the emergency room after suffering an accidental fall, assessed as an osteochondral fracture-dislocation of the right patella with upper-outer displaced free fragments. By patient interview, she referred to no previous episodes of patellar dislocation. To complete the study, we performed an MRI which showed a medial facet patellar fracture, with two osteochondral fragments located in the sub-quadricipital recess, associated with other lesions suggesting patellar subluxation.
We considered that the best treatment was surgery, so the following was performed: an open reduction and internal fixation with absorbable bars, lateral patellar release (Ficat technique), patellar coverage by medial portion of quadriceps (Insall technique) and internal moving of the lateral half of the patellar tendon (Goldwaith technique).
The injury was checked 1year later using arthroscopy. It confirmed a good reconstruction of the articular surface, and right patellar centring.
At follow-up, during the physiotherapy period, the patient began to have repeated episodes of instability in the contralateral patella. The CT scan confirmed the patellar lateralisation (TAGT 17). Centring surgery was indicated due to the occurrence of multiple dislocation episodes.
The patient currently carries out normal physical activity and she has a complete range of movement.
Patellar osteochondral fracture is an injury frequently associated with patellar instability, which may onset in the first episode.
The medial location of the lesions and the involvement of the system of medial knee stability is a fundamental finding. This fact reinforces the diagnosis of pre-fracture patellar dislocation. This is not a fracture-dislocation, but a dislocation-fracture. We may, therefore, treat the injury and its cause.
Las fracturas osteocondrales patelares sin luxación son infrecuentes, y suelen afectar a la faceta centromedial de la rótula. Presentamos el caso de una niña de 10 años con sobrepeso, que acude a urgencias después de sufrir una caída casual, valorándose como una fractura-luxación ostecondral rotuliana derecha con desplazamiento supero-externo. Al historiar la paciente, no refiere episodios previos de luxación rotuliana. Para completar el estudio, realizamos una resonancia magnética que objetiva una fractura osteocondral de faceta medial rotuliana desprendiéndose dos fragmentos que se sitúan en el receso subcuadricipital y lesiones sugestivas de subluxación rotuliana.
Se efectúa la cirugía, realizándose reducción y osteosíntesis con barras reabsorbibles y recentraje rotuliano derecho mediante liberación lateral y traslación interna del hemitendón rotuliano externo según técnica de Goldthwaith.
Una artroscopia de revisión confirma una buena reconstrucción y centraje rotuliano derecho. En el seguimiento, durante el período de rehabilitación, la paciente inicia episodios repetidos de inestabilidad en la rótula contralateral. Se realiza una tomografía computarizada que confirma la lateralización de la misma con una TAGT de 17. Al repetir estos episodios de inestabilidad, se indica un centraje rotuliano mediante las técnicas de Insall (disección del músculo vasto interno, cubriendo la rótula con el colgajo del mismo), Ficat (sección del alerón lateral externo), Goldwaith (traslación hacia metáfisis tibial superointerna del hemitendón rotuliano externo).
La paciente, actualmente, realiza actividad física sin limitación y con un balance articular completo.
La fractura osteocondral patelar es una lesión frecuentemente asociada a inestabilidad rotuliana, pudiendo debutar en el primer episodio.
La localización medial de las lesiones y la afectación del sistema de estabilidad medial de la rodilla es un dato fundamental. Esto refuerza el diagnóstico de luxación patelar previa a la fractura osteondral, no es una fractura-luxación, sino una luxación-fractura. Debemos, por tanto, tratar la lesión y su causa.
Patella fractures are much less frequent in children for several reasons. Firstly, the cartilage of the patellar articular surface protects this bone from direct contusions. Likewise, it is less sensitive to tension forces due to a shorter moment of force on a shorter muscle length. In addition, a child's patella has greater mobility in the coronal plane.1
One of the most conflictive points in kneecap fractures in children is perhaps the diagnosis. As this structure is composed of mostly cartilage, paediatric patellar lesions can be underdiagnosed or the diagnosis can be delayed.
As to the injury mechanics, we know that among children the alteration of the extensor apparatus2 is one of the most frequent causes of patellar avulsion.
It is possible to establish a relationship between the location of the osteochondral knee injury and its cause.
In relation to osteochondral patellar fractures of the lateral articular surface, Kennedy3 describes 2 fracture mechanisms. The first, exogenous, is due to a flexor-rotation mechanism. The second, endogenous and the most customary, stems from patellar dislocation. In the latter case, the lesions are found in the medial side of the patella. For that reason, the literature recommends surgical treatment for an osteochondral fracture associated with repairing the medial retinaculum.
Injuries to the medial femoral condyle are related to a direct contusion (a fall) or to a compression-rotation (tibiofemoral) mechanism. For the lateral femoral condyle, the mechanisms can be a direct contusion (blow), compression-rotation (tibiofemoral) or acute patellar dislocation.
We present the case of a 10-year-old patient, having no known history of kneecap dislocation, with a post-traumatic osteochondral fracture. Under these circumstances, the therapeutic approach to the injury and/or to its possible causes poses a challenge.
Clinical caseWe present the case of an overweight 10-year-old girl who came to our emergency service for post-traumatic pain in the knee after a simple fall. No episodes of patellar dislocation were reported when taking the case history.
Examination revealed articular leakage and pain on palpating the upper pole of the kneecap. Extension of the active knee was present and there were no other significant examination results.
A simple X-ray showed a kneecap fragment displaced in a superoexternal direction. To get a better idea of the injury, magnetic resonance imaging (MRI) was performed, revealing an osteochondral fracture of the medial patellar facet with 2 free fragments in the subquadricipital recess. It also showed an area of osseous contusion with an impact fracture in the border of the external femoral condyle, associated with an injury to the internal and patellofemoral ligaments, giving an aspect of external patellar subluxation4 (Fig. 1).
Magnetic resonance image of the knee, transversal cut. Osteochondral fracture of the medial patellar facet with 2 free fragments, focal osseous contusion; impacted fracture from impaction on the border of the external femoral condyle and a lesion in the internal and patellofemoral ligaments.
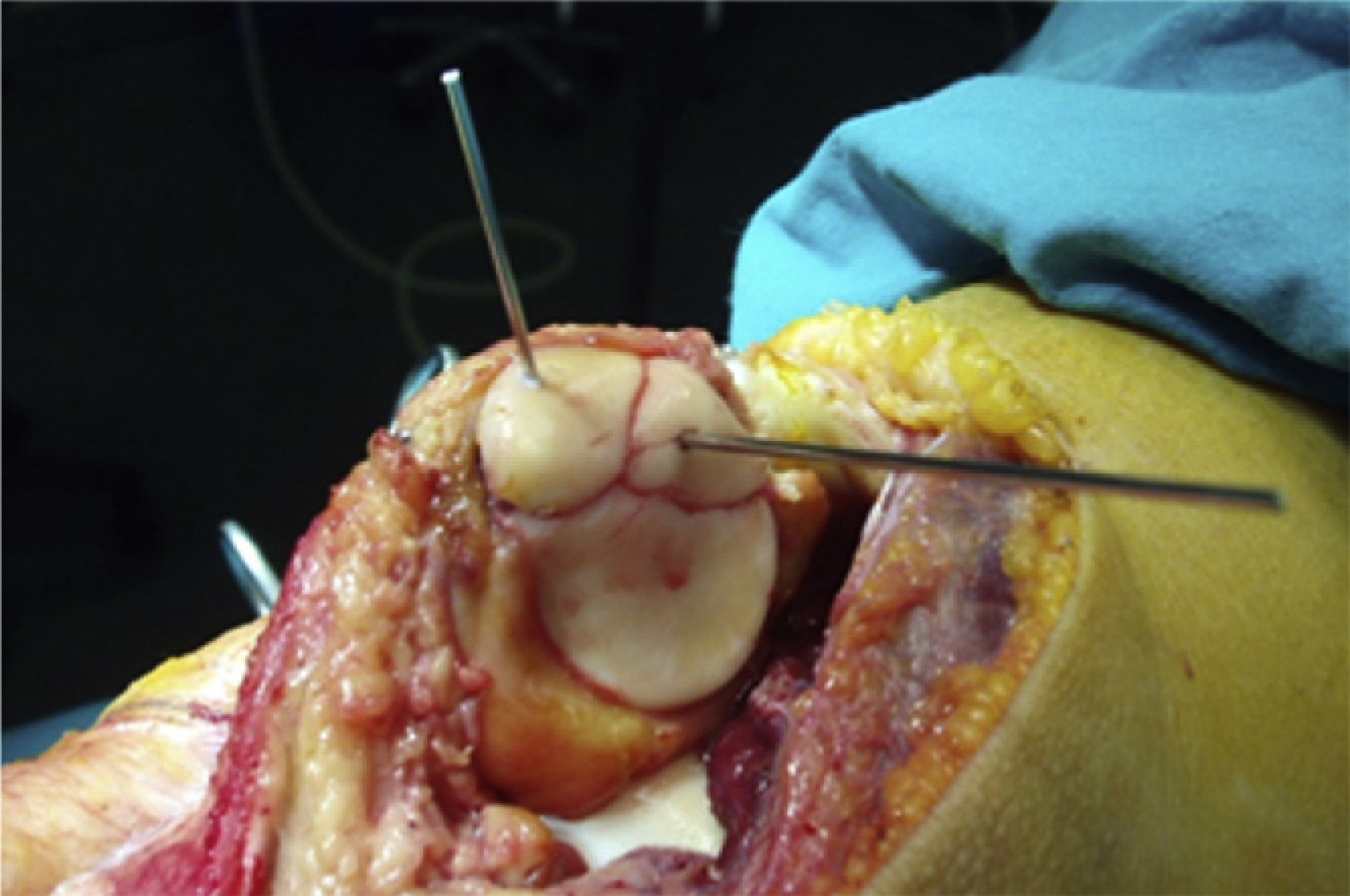
Surgery was indicated based on the study on the injury. After open reduction by an internal parapatellar approach, synthesis was achieved through resorbable rods5 and coverage with the internal vastus. The right patella was recentred by freeing the external ligament laterally (Ficat procedure), the patella was covered with an internal vastus flap (Insall procedure) and the external patellar hemi-tendon was moved internally (Goldthwait procedure) (Fig. 2).
To check the final state of the knee and the result of the surgical reconstruction, an arthroscopy was performed 1year after the injury.6 This showed complete reduction of the patellar articular face, with satisfactory reconstruction of the external facet and crest, the global aspect thus being good. The patella showed correct translation in the femoral trochlea.
In the follow-up of the knee operated on (right), we found full joint balance, with patella stability. Unexpectedly, the patient then began to present episodes of patella instability in the contralateral (left) knee. A computed tomography study evidenced a lateralisation of the contralateral (left) patella, with TAGT 13.2 Faced with a clinical picture that suggested patella instability, along with a few corroborating complementary tests,7 we opted for surgical treatment. The operation was the same as that performed on the other knee, using the Insall, Ficat and Goldthwait procedures.
At present, the patient has been discharged. She can perform physical activities without any limitations and has full joint balance.
DiscussionIn children or adolescents, patellar osteochondral injuries without patella dislocation are infrequent.2,4 In cases of lateral patella dislocation, there are associated patellar joint injuries in up to 95% of the cases, according to Nomura et al.,6 against only 39% for Nietosvaara et al.8
In the series published by Elías,5 up to 90% of young patients who suffered a lateral patella dislocation had not presented symptoms of instability before the episode. Consequently, we can link the osteochondral fractures of the patella with patellar instability. We recommend searching for possible patella instability, differentiating between post-traumatic osteochondral injuries and those related to patella dislocation. To do so, the case history and the examination are important, along with the MRI findings.
Cases caused by patella dislocation involve a medial osteochondral injury, not a centromedial one; the injury is associated with ligament injury to the medial patellofemoral ligament or the medial retinaculum.1 In 31% of the cases, there are injuries to the lateral femoral condyle. This was confirmed in our patient, who presented injuries to the lateromedial stability complex of the knee and a medially located osteochondral fracture. We could then confirm that the cause of the injury was patellar lateral dislocation. What initially seemed to be a fracture-dislocation was really a dislocation-fracture. This case reinforces the importance of eliminating an underlying lateral patella instability in every patient with a medial patellar osteochondral fracture, as is also indicated in the literature.4,6
Injuries associated with dislocation can be osteochondral lesions (19%), isolated patella fractures (24%) or both of these together (57%).6 In our case, there was an isolated osteochondral fracture with no disruption of the remaining cartilage. According to Nomura et al.,6 this group is the least frequent among the injuries associated with patella dislocation.
If a case history and/or MRI findings confirm this, it will be an osteochondral injury and, likewise, the most probable cause will be patellar instability.
Paganopoulos9 points out the importance of the medial patellofemoral ligament as the main ligamentous stabiliser of the patella.10 Evaluating the integrity of this structure by MRI is essential in patellar instability treatment. If there is an injury, its reconstruction is the first priority, normally through autologous tendon plasty of the semitendinosus muscle.9
In the treatment of any patella fracture, the objective must be anatomical reduction and stable synthesis, so as to permit prompt knee rehabilitation.2 As Qi5 published, we feel that bioabsorbable materials yield good consolidation results, without the risks involved in metallic implants, such as migration or local irritation from rubbing.
In agreement with Nomura et al.,6 we support the usefulness of arthroscopic follow-up of knees subjected to this type of injuries, to evaluate the state of the articular facet or to remove any possible free bodies.
Level of evidenceLevel of evidence V.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Please cite this article as: Cepero-Campà S, et al. Lesión osteocondral patelar como debut de una inestabilidad rotuliana. Rev esp cir ortop traumatol. 2012;56(1):63-66.