Postoperative pain after total hip arthroplasty can affect postoperative rehabilitation and delay hospital discharge. The objective of this study is to compare pericapsular nerves group (PENG) block with pericapsular infiltration (PAI) and plexus nerve block (PNB) for postoperative pain management, response to physical therapy, opioid consumption, and length of hospital stay after a primary total hip arthroplasty.
MethodsRandomised clinical trial of parallel and blinded groups was performed. Sixty patients who underwent elective THA between December 2018 and July 2020 were randomised into the different groups (PENG, PAI and PNB). The visual analogue scale was used to assess pain; and motor function was measured with the Bromage scale. We also record opioid usage, length of hospital stay, and related medical complications.
ResultsPain level at discharge was similar in all groups. Hospital stay was 1 day shorter in the PENG group (p<0.001) and they also had lower opioid consumption (p=0.044). Optimal motor recovery was similar in the groups (p=0.678). Pain control when performing physical therapy was better in the PENG group (p<0.0001).
ConclusionsPENG block is an effective and safe alternative for patients undergoing THA as it reduces opioid consumption and hospital stay compared to other analgesic methods.
El dolor postoperatorio luego de una artroplastia total de cadera puede afectar la rehabilitación postoperatoria y retrasar el alta hospitalaria. El objetivo de este estudio es comparar el bloqueo PENG con PAI, PNB para el manejo del dolor postoperatorio, la respuesta a la fisioterapia, el consumo de opioides y la duración de la estancia hospitalaria.
MétodosEnsayo clínico aleatorizado de grupos paralelos y ciego para la evaluación. Sesenta pacientes sometidos a ATC electiva entre diciembre de 2018 y julio de 2020 fueron asignados al azar en los diferentes grupos. Se utilizó la escala visual analógica para evaluar el dolor, y la función motora se midió con la escala de Bromage. También registramos el consumo de opioides, la duración de la estancia hospitalaria y las complicaciones médicas relacionadas.
ResultadosEl nivel de dolor en el momento del alta fue similar en todos los grupos. La estancia hospitalaria fue un día menor en el grupo PENG (p<0,001), y este grupo también tuvo menor consumo de opioides (p=0,044). La recuperación motora óptima fue similar en los grupos (p=0,678). El control del dolor al realizar fisioterapia fue mejor en el grupo PENG (p<0,0001).
ConclusionesEl bloqueo PENG es una alternativa efectiva y segura para los pacientes sometidos a ATC al disminuir el consumo de opioides y la estancia hospitalaria en comparación con otros métodos analgésicos.
The number of total hip arthroplasty (THA) procedures performed each year is increasing, with a projected annual volume of more than 4 million cases by 2030 in the United States.1 This growing number of THAs is closely related to improvements in the quality of materials, surgical techniques, anaesthesia, and postoperative care.1 THA is one of the most common orthopaedic surgical procedures worldwide and has a major impact on improving the quality of life of people with degenerative hip disease.2
Although this intervention has good outcomes in terms of patient satisfaction, effective postoperative pain management can minimise the need for opioids and their adverse effects.3 Pain after surgery leads to a need for rest, interruptions in physiotherapy, and delays in ambulation. This prolonged rest increases the risk of thromboembolism, muscle atrophy, and functional impairment, resulting in a longer hospital stay.2–4
The term multimodal analgesia describes pain management using both pharmacological and non-pharmacological techniques, which aims to maximise the positive aspects of treatment and limit side effects.5 The American Society of Anaesthesiologists recommends the use of 2 or more analgesic modalities with different mechanisms of action.6
Over time, different routes of analgesia have been incorporated, such as surgeon-provided periarticular infiltration (PAI),7 femoral nerve block,8 and plexus nerve block (PNB).9 A new regional anaesthetic technique has emerged, called pericapsular nerve group block (PENG), which targets the anterior hip capsule by blocking the articular branches of the femoral nerve and obturator accessory nerve.10,11
The aim of this study was to compare PENG blockade in patients undergoing THA with PAI and PNB for postoperative pain relief, and determine whether there are differences in pain level, response to physiotherapy, opioid consumption, and length of hospital stay.
MethodsDesignRandomised, participant-blinded, observer-blinded clinical trial. The present study was approved by our institution's health sciences ethics committee. All patients received oral and written information about the trial and signed an informed consent form prior to inclusion. The trial was reported in accordance with the CONSORT statement.12
Participants and settingThe study was conducted in a private clinic in the city of Cordoba, Argentina. We included adult patients (18 years or older) who underwent elective primary THA secondary to degenerative osteoarthritis, with an American Society of Anaesthesiologists (ASA) classification I, II, or III. We excluded all patients with chronic opioid use, body mass index>45, allergies to study drugs, impaired cognitive function, contraindication for regional anaesthesia, major systemic diseases such as chronic kidney disease, cardiac (New York Heart Association class III or IV congestive heart failure), or liver disease.
Randomisation and maskingPatients were randomly assigned to one of the interventions PNB, PAI, or PENG. The randomisation sequence was generated using an electronic randomisation generator (/www.sealedenvelope.com). The allocation ratio was 1:1 in fixed blocks of 3. The nurse anaesthetist opened an opaque sealed envelope in the operating theatre and allocated the patient according to the sequence. Due to the nature of the procedure it was not possible to mask the anaesthetist or nurse anaesthetist. However, the surgeon (attending physician), the research physicians attending the patient and the kinesiologists involved in the rehabilitation were unaware of the allocation. The study staff who assessed the event (kinesiologists) were unaware of the allocation of the intervention. Patients who received regional anaesthesia without sedation were not blinded to the treatment assigned, while those who underwent general anaesthesia were blinded to the treatment assigned.
InterventionAfter the intervention the participants received the block according to the randomisation as follows:
PNB: after wound closure, and using Capdevilla and Stimuplex® Ultra Braun landmarks with a 22G .7mm×100mm needle, ultrasound guided, the lumbar plexus was infiltrated by a senior anaesthesiologist with a 20ml solution of .25% bupivacaine with epinephrine.
PAI: before wound closure the surgeon infiltrated the anterior, posterior, and inferior hip capsule with 80ml of a mixture of morphine 10mg, ketorolac 60mg, and bupivacaine .25% with epinephrine.
PENG: after wound closure, the patient was placed in a dorsal recumbent position and the articular branches of the femoral nerve and obturator accessory nerve were infiltrated by the senior anaesthesiologist using ultrasound guidance. A 20ml solution of .25% bupivacaine with epinephrine was used.
All surgical procedures were performed under spinal anaesthesia using a posterolateral approach.
At the preoperative visit all participants were instructed to take preventive oral analgesia from 24h before the surgical procedure with 500mg paracetamol twice daily orally (PO) and 300mg gabapentin PO on the day, according to our standard protocol for THA. After the surgery, paracetamol 500mg 3 times daily (PV), etoricoxib 60mg 2 times daily (PV), and gabapentin 300mg at night (PV) were indicated. Patients were monitored to assess their degree of pain and a rescue dose of tramadol 50mg (PO) was given to those who reported visual analogue scale (VAS) pain greater than or equal to 5.
Definition of outcome variablesPainPain was assessed by the kinesiologists initially at rest (baseline and at 6h) and, once kinesiotherapy was initiated, after each session and until discharge. Data were collected using a VAS pain form on a scale from 1 to 10, which was given to the patient to complete.
Hospital stayHospital stay was measured from the date of admission to the date of discharge, where the patient had to meet the criteria of being able to stand, walk a distance of 30m, and score less than 3 points on the VAS.
Use of opioids and derivativesWe recorded whether the patients required tramadol rescue in the first 48h as a dichotomous variable.
Motor functionMotor function was measured using the Bromage scale13 to assess motor block of the lower extremities. There is a score of 1 if there is no motor block and up to 4 if the block is complete. Measurements were taken at the end of surgery, one hour after surgery, and the total time to complete motor recovery was recorded.
ComplicationsPostoperative complication was defined as any eventuality occurring in the anticipated course of the surgical procedure with local or systemic response that could delay recovery, compromise function, or be life threatening.
Statistical analysisContinuous variables were described as mean and standard deviation (SD) or median and interquartile range 25–75 (IQR) according to the distribution of the data. The Shapiro Wilks test was used for this purpose. To compare variables between groups, the ANOVA or Kruskal–Wallis test was used for continuous variables, and the χ2 test for categorical variables.
Linear regression models were performed to compare pain at each time interval. The PNB group was used as a reference category.
As a secondary analysis we fitted generalised estimating equations, to make use of the repeated measures of pain. Specifically, we used an identity link, normal distribution, individual-level clustering, and the sandwich estimator to construct 95% confidence intervals. The models included indicators of time, group assignment and their interaction. The baseline measure was retained for this analysis as part of the response vector.
A significance level equal to .05 was used in all cases.
Sample sizeTaking a type I error of 5% and a type II error of 20% to detect a pain scale difference between groups of 2/10 points on the VAS, with an SD of 3 points, 18 patients per treatment arm were required to be included. The number was increased by 10% for potential loss to follow-up or withdrawal of consent, and therefore 20 participants per arm were finally included.
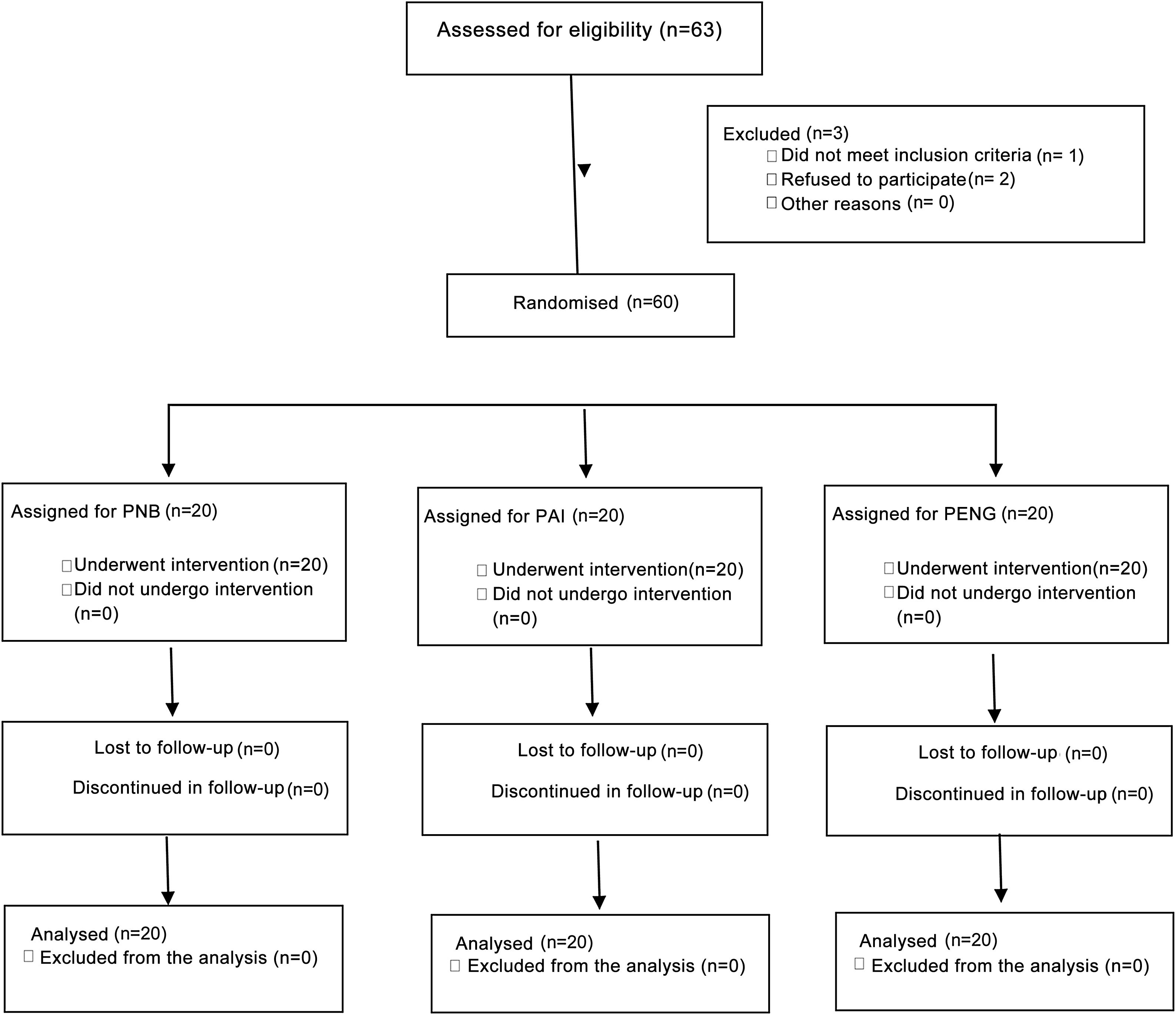
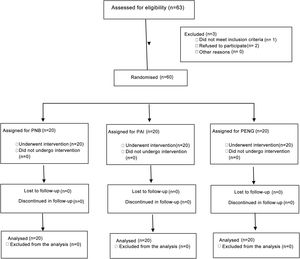
ResultsBaseline characteristicsBetween December 2018 and July 2020, 63 potential participants were screened, of which 60 were included in the study. There were no losses to follow-up. Fig. 1 shows the flow of participants. The median age was 61.5 years (IQR 57–68) and 31 participants (51.7%) were male.
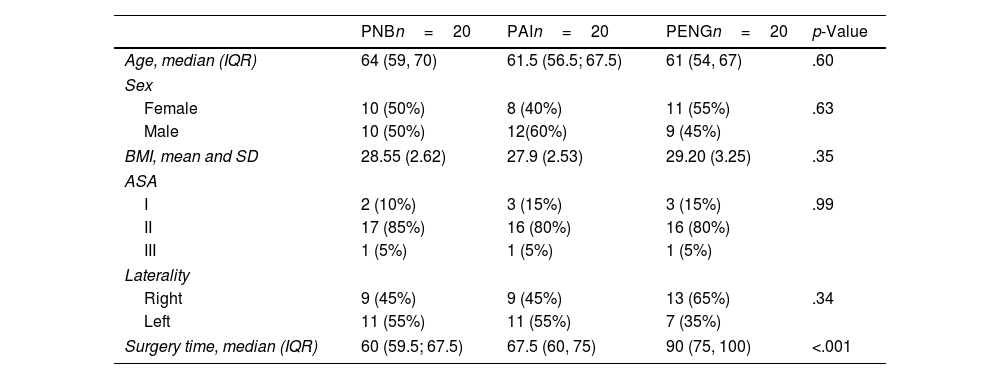
No significant differences in baseline characteristics were found between the different study arms (Table 1). The duration of the surgical procedure was longer in the PNB group because this technique requires more time to perform the block.
Baseline characteristics of the 60 participants.
| PNBn=20 | PAIn=20 | PENGn=20 | p-Value | |
|---|---|---|---|---|
| Age, median (IQR) | 64 (59, 70) | 61.5 (56.5; 67.5) | 61 (54, 67) | .60 |
| Sex | ||||
| Female | 10 (50%) | 8 (40%) | 11 (55%) | .63 |
| Male | 10 (50%) | 12(60%) | 9 (45%) | |
| BMI, mean and SD | 28.55 (2.62) | 27.9 (2.53) | 29.20 (3.25) | .35 |
| ASA | ||||
| I | 2 (10%) | 3 (15%) | 3 (15%) | .99 |
| II | 17 (85%) | 16 (80%) | 16 (80%) | |
| III | 1 (5%) | 1 (5%) | 1 (5%) | |
| Laterality | ||||
| Right | 9 (45%) | 9 (45%) | 13 (65%) | .34 |
| Left | 11 (55%) | 11 (55%) | 7 (35%) | |
| Surgery time, median (IQR) | 60 (59.5; 67.5) | 67.5 (60, 75) | 90 (75, 100) | <.001 |
BMI: body mass index; PAI: periarticular infiltration, PENG: pericapsular nerve group block; PNB: plexus nerve block.
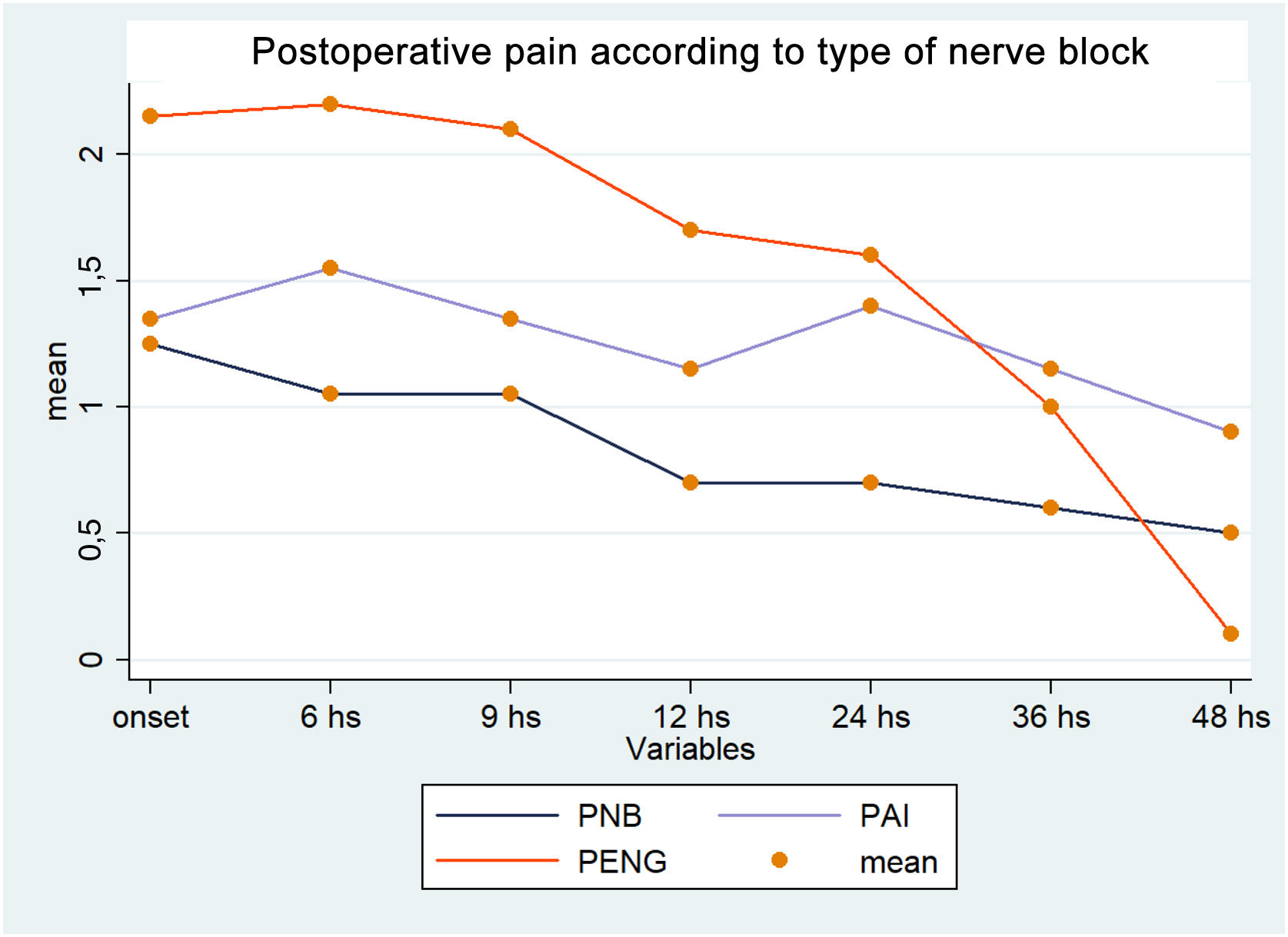
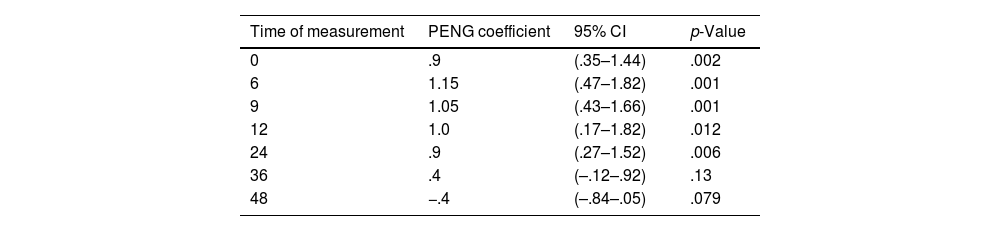
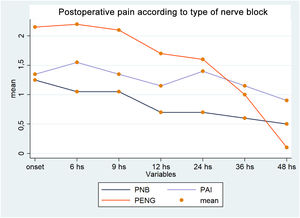
With all the interventions the mean pain was between 1 and 3, and therefore they can be grouped within a range of mild pain. There was no difference in pain level between PNB and PAI in successive measurements in the linear regression analysis (Table 2). During the first 24h the pain level with the PENG technique was about one unit higher than with the other 2 interventions. After that time no differences were found between intervention groups in pain control (Fig. 2).
Pain level of the PENG technique compared to the reference technique PNB.
| Time of measurement | PENG coefficient | 95% CI | p-Value |
|---|---|---|---|
| 0 | .9 | (.35–1.44) | .002 |
| 6 | 1.15 | (.47–1.82) | .001 |
| 9 | 1.05 | (.43–1.66) | .001 |
| 12 | 1.0 | (.17–1.82) | .012 |
| 24 | .9 | (.27–1.52) | .006 |
| 36 | .4 | (–.12–.92) | .13 |
| 48 | −.4 | (–.84–.05) | .079 |
This table shows the regression coefficients of the pericapsular nerve group block (PENG) group versus the reference (lumbar plexus block) in each of the 7 linear regression models performed at each time cut-off.
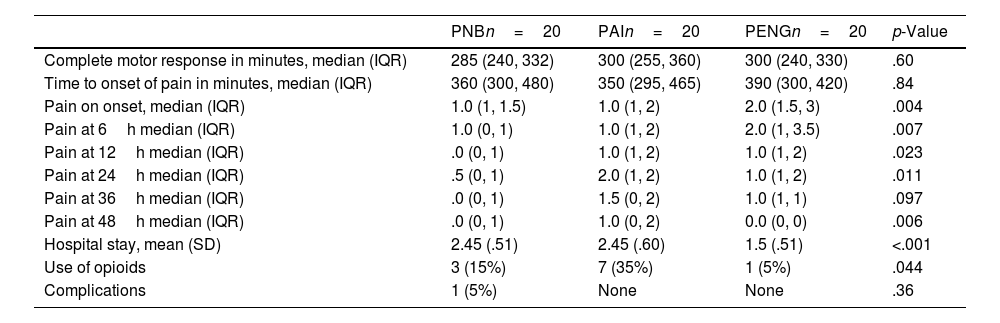
Hospital stay was shorter in the PENG group (1.5 days vs. 2.45 days in the PAI group vs. 2.45 days in the PNB group) (p<.001) (Table 3).
Main results.
| PNBn=20 | PAIn=20 | PENGn=20 | p-Value | |
|---|---|---|---|---|
| Complete motor response in minutes, median (IQR) | 285 (240, 332) | 300 (255, 360) | 300 (240, 330) | .60 |
| Time to onset of pain in minutes, median (IQR) | 360 (300, 480) | 350 (295, 465) | 390 (300, 420) | .84 |
| Pain on onset, median (IQR) | 1.0 (1, 1.5) | 1.0 (1, 2) | 2.0 (1.5, 3) | .004 |
| Pain at 6h median (IQR) | 1.0 (0, 1) | 1.0 (1, 2) | 2.0 (1, 3.5) | .007 |
| Pain at 12h median (IQR) | .0 (0, 1) | 1.0 (1, 2) | 1.0 (1, 2) | .023 |
| Pain at 24h median (IQR) | .5 (0, 1) | 2.0 (1, 2) | 1.0 (1, 2) | .011 |
| Pain at 36h median (IQR) | .0 (0, 1) | 1.5 (0, 2) | 1.0 (1, 1) | .097 |
| Pain at 48h median (IQR) | .0 (0, 1) | 1.0 (0, 2) | 0.0 (0, 0) | .006 |
| Hospital stay, mean (SD) | 2.45 (.51) | 2.45 (.60) | 1.5 (.51) | <.001 |
| Use of opioids | 3 (15%) | 7 (35%) | 1 (5%) | .044 |
| Complications | 1 (5%) | None | None | .36 |
IQR: interquartile range; PAI: periarticular infiltration, PENG: pericapsular nerve group block; PNB: plexus nerve block; SD: standard deviation.
Only one patient (5%) in the PENG group required rescue, while 3 patients (15%) in the PNB group and 7 (35%) in the PAI group required rescue, with a significant difference p=.044.
Motor assessmentRegarding the initial motor assessment (immediately after surgery) 80% of the patients in the PNB group, 90% in the PAI group, and 95% in the PENG group reported inability to move their legs. There was no significant difference between the groups (p=.322). One hour after surgery motor assessment improved in all groups with no significant differences (p=.754).
Median optimal motor recovery was similar in the groups (PNB 285 minutes (IQR: 240–332), PAI 300 minutes (RIC: 255–360), PENG 300 minutes (IQR: 240–330). There was no statistical difference between groups (p=.60) (Table 3).
ComplicationsWe recorded only one medical complication in the PNB group. One patient suffered an episode of hypotension 5 minutes after the procedure. The patient recovered the same morning without sequelae. There were no medical complications in the other groups.
Secondary analysisOur calculations using generalised estimating equations (GEE) show similar results to our linear regression assessing the change in pain from baseline to 48h. We observe that there is a significant effect of time alone on pain improvement, which is independent of the intervention, and significant effect of the intervention over time. Throughout the whole study the pain level in the PENG group was 1.07 (95% CI: .49–1.65), higher than PNB p<.001, while in the PAI group it was .65 (95% CI: .20–1.10) p=.005.
DiscussionIn our study we found that postoperative pain was mild after all the interventions, particularly in the PENG group we observed that in the first 24h pain was one point above the other interventions, while at 48h it was below the average pain. In terms of length of hospital stay, one day less was recorded for the PENG group than the other groups and lower opioid consumption. There were no significant complications in any of the groups.
We also observed that using any of the 3 analgesic modalities, patients experienced similar motor recovery and there was no advantage of one technique over another in terms of initiation of physiotherapy.
We believe that the delayed effect of the PENG group in reaching the same level of pain as the other groups may be due to the technique being more operator dependent than the other modalities. A similar effect was observed in the study by Bober et al. where patients received an iliac fascia block vs. placebo. The pain level was between 3 and 4 for the first 24h, and in patients who received the block it dropped markedly after that period.12 In the study by Lin et al. comparing PENG with femoral block, patients in the PENG group experienced less pain during the first postoperative day.13
Several previous publications have examined functional recovery, and these studies demonstrate improved rehabilitation after THA when comparing different blocks with lumbar epidural anaesthesia.14–17 This demonstrates that the new analgesia techniques improved patient tolerance to physiotherapy.
Regarding medical complications, for all the blocks the incidence of infections is reported as very low, ranging from .07% to 3%, typically occurring in patients with multiple risk factors.18–20 In our cohort we found no wound complications, only one patient suffered an episode of hypotension which recovered the same morning.
LimitationsThis study has some limitations; firstly, the sample size is small and certain characteristics of the participants may not have been balanced in the randomisation. Follow-up of participants is short, and therefore we have no information on pain, motor function or complications beyond discharge.
While this is one of the first randomised studies comparing the most common analgesic block techniques, more studies are needed to further corroborate our findings.
ConclusionPENG blockade is an alternative in patients undergoing THA by reducing opioid consumption and hospital stay compared to other analgesic methods. The level of pain at discharge was similar in all groups. It is a safe and useful technique, however, it requires anaesthesiologists familiar with the technique.
Level of evidenceLevel of evidence ii.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.