To establish the prevalence of lesions of the labrum and articular cartilage of the hip in asymptomatic elite soccer players by performing 3T magnetic resonance imaging.
MethodsEighty-four asymptomatic hips of 42 professional soccer players were evaluated. Male subjects older than 18 years were included. Cam and pincer deformity were defined as an alpha angle greater than 55 degrees and a lateral centre edge angle greater than 39 degrees, respectively. Labral injuries were classified with the Czerny classification and cartilage damage was classified with the Outerbridge classification. Specific statistical tests were used to establish the relationship between anatomical variances of the hip and the presence of chondral and labral injuries.
ResultsFAI morphology prevalence was 25%. Abnormalities such as cam (22.5%) and labral injuries (33.8%) were found. Those cases with reported labral injury were predominantly intrasubstance damage (18.8%). Anatomical features of FAI were found to be related to lesions of the femoral cartilage (p<.001), chondrolabral damage (p=.042), or both injuries (p<.001).
ConclusionAsymptomatic labral or cartilaginous injuries of the hip were reported in 25% of the included professional soccer players. These injuries were associated with anatomical features of FAI.
Establecer la prevalencia de lesiones del labrum y el cartílago articular de la cadera en futbolistas profesionales asintomáticos y explorar la asociación con hallazgos en las pruebas de imagen de choque femoroacetabular (CFA).
MétodosEstudio de corte transversal que evaluó por imagen de resonancia magnética en 3 tesla (IRM 3 T) un total de 84 caderas en jugadores de fútbol profesional, con edades entre los 18 y 31 años. Se identificaron las lesiones del labrum y las del cartílago acetabular y femoral. Pruebas estadísticas específicas fueron utilizadas para establecer la relación entre las alteraciones anatómicas de CFA y la presencia de lesiones condrolabrales.
ResultadosLa prevalencia de CFA fue del 25%, siendo el tipo cam el más predominante con 22,5%. Para las lesiones del labrum existe una prevalencia de 33,8%, de las cuales el 18,8% fueron para degeneración intrasustancial y 2,5% para rotura completa. Las características anatómicas de la cadera según el tipo de CFA están asociadas con lesiones del cartílago femoral p<0,001, lesiones de la unión condrolabral p=0,042 y lesión combinada (presencia de lesión del labrum o cartílago o acetabular o femoral o unión condro-labral) p<0,001.
ConclusiónExiste una alta prevalencia de lesiones asintomáticas del labrum y del cartílago articular de la cadera en futbolistas profesionales, las cuales se asocian a las características anatómicas de CFA de cadera.
Labral or cartilage lesions in the absence of abnormalities typical of femoroacetabular impingement (FAI) rarely occur1; however, not all patients with these typical abnormalities have chondrolabral lesions. This seems to indicate that, in addition to the anatomical variances identified in FAI, there are further predisposing factors that result in the progressive deterioration of the hip joint towards OA.
Some sports activities that involve repeated hip movements with extreme joint arc movements could be a determining factor for lesions of the labrum and cartilage in the presence of anatomical abnormalities of the femur and acetabulum. This could explain, in part, why athletes have 2–4.5 times the risk of the general population of developing arthrosis.2
Because the length of time between diagnosis and appropriate treatment of FAI, or its associated lesions, could impact the outcome and sporting future of professional footballers, it is particularly important that injuries that are susceptible to intervention are detected promptly to prevent progression to irreparable labral damage or early-onset osteoarthritis.
Magnetic resonance imaging (MRI) can assess lesions of the labrum and cartilage as well as anatomical variances of FAI, with better diagnostic accuracy when direct intra-articular contrast is used (direct magnetic resonance arthrography).3–5
Acute detection of labral injuries and chondral defects is possible without using intra-articular gadolinium. Recent advances in MRI resolution, with 3Tesla (T) equipment available in our environment, enable sufficient anatomical detail so that the use of a contrast dye is not essential, with the consequent advantage for patient safety,6 and therefore 3T images are preferred to 1.5T.7
Although there are published articles on the frequency of clinical and imaging findings of FAI in elite athletes,2,8–12 the frequency of associated lesions found by 3T MRI has not been determined.
The objective of this study was to establish the prevalence of lesions of the articular cartilage of the hip in professional footballers using 3T MRI, and to explore the association with findings on imaging tests of FAI in professional footballers.
The hypothesis of this study was that there is a high prevalence of lesions of the labrum and cartilage, which are associated with the anatomical characteristics of FAI of the hip.
Material and methodsOn the approval of the Instituto de Alta Tecnología Médica de Antioquia (IATM) (Institute of Advanced Medical Technology of Antioquia), we undertook a cross-sectional study that included 42 footballers, aged between 18 and 31 years, from 3 first division teams coded as team A, team B and team C. The subjects, who were asymptomatic, underwent a clinical assessment and 3T MRI of both hips.
Athletes with a history of fracture around the hip, with a history of Perthes disease or hip dysplasia, and those for whom MRI was contraindicated were excluded from the study.
Clinical assessmentThe clinical assessment of the hip was carried out by an orthopaedic surgeon specialising in hip surgery. The flexion angles, internal rotation, external rotation, adduction and abduction were measured in the supine position and manually with a goniometer. The tests used to evaluate the anterolateral and posterior impact of the hip were: the FADDIR test,13,14 that assesses pain with the hip flexed to 90 degrees, and adducted and internally rotated; the FABER test,14 that evaluates pain with the hip flexed, and adducted and externally rotated, and measures the distance between the knee of the limb assessed with the examination table and comparing this distance with the other limb in the same position; this test helps to determine whether the pain originates in the hip or the posterior region such as in the sacroiliac joint; the DEXRIT test15 (dynamic external rotatory impingement test), which assesses pain in the hip by taking it to 90 degrees flexion and then making an arc movement of abduction and external rotation, thus assessing impingement or posterior-superior acetabular impingement and sense of anteroinferior instability and log roll sign,13 and with the patient in the supine position and their hip and knee extended, a log roll movement of the limb is made in internal and external rotation on the examination table to check whether or not there is pain on the anterior surface of the examined hip.
In addition to taking the clinical history and the physical examination, a standard anthropometric assessment was made that included weighing the subject using a Tanita® electronic scale (Tanita Corporation of America, Inc., IL, USA), their height was measured using a Seca 206® stadiometer (HRM USA Inc., Hamburg, Germany), their BMI was measured according to the traditional weight/height2 formula, and their body fat (BF) percentage was calculated using the formula validated by Evans from 2005,16 which uses the sum of 3 skin folds: abdomen, thigh and triceps, measured using a Slim Guide® body fat calliper (Creative Health, MI, USA). The hip, muscle and leg circumferences were also measured with a Seca 201® metric tape (HRM USA Inc., Hamburg, Germany).
Acquisition and interpretation of 3T magnetic resonance imagesThe imaging was performed by a radiological technician trained in the specifications required for the study; they stored the images in digital format and assigned them the corresponding code. A specialist radiologist in osteomuscular imaging, blinded for the clinical assessment, then analysed each of the magnetic resonance images.
The studies were performed on a Philips Ingenia 3T system, 4.1.3 (High Tech Campus 5, Eindhoven, Holland) with the following sequences: wide FOV images including both hips in coronal STIR (TR 3752, TE 30 and TI 190, with a duration of 2min and 22s), coronal T1 (TR 500 TE 20, with a duration of 1min and 51s), axial fat-suppressed proton density (TR4479, TE 30 duration of 1m and 38s), axial isotropic 3D gradient echo (TR 15, TE 4, and a duration of 1min and 51s) and axial T2 (TR 5309, TE 110, and a duration of 1min and 46s); in addition, small localised FOV sequences were performed on each hip in coronal fat-suppressed proton-density (TR 2234, TE 30, duration of 1min and 51s) and sagittal proton-density (TR 3300, TE 28, duration of 2min and 12s) for a total examination duration of 20min after adding the localiser time. These isotropic volumetric sequences enabled axial oblique reconstruction.
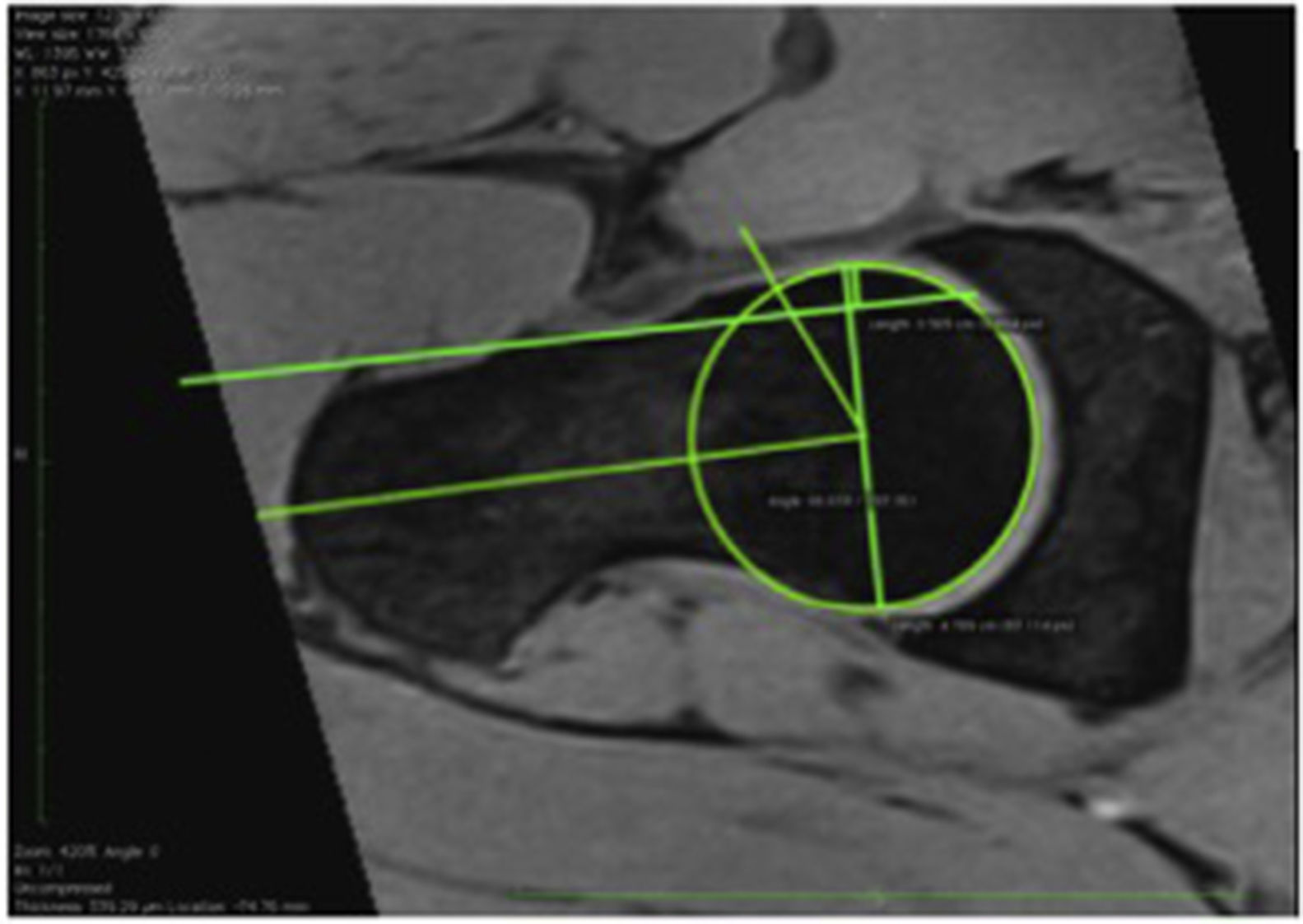
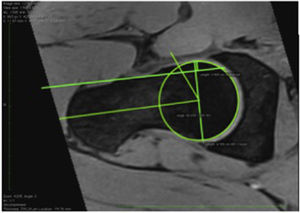
Cam lesions were evaluated by measuring the alpha angle on the axial oblique reconstruction between the axis of the femoral neck and a line connecting the centre of the femoral head to the start point of the sphericity of the head-neck contour. Subjects with an alpha angle >55° were diagnosed with a cam-type impingement.7–20
A diagnosis of pincer-type impingement was principally established by a centre edge angle measurement >39° (FAI), which is an indicator of excess acetabular coverage. The FAI was measured on the coronal plane between a vertical line passing through the centre of the femoral head and another line from the centre of the femoral head to the lateral acetabulum.21–23
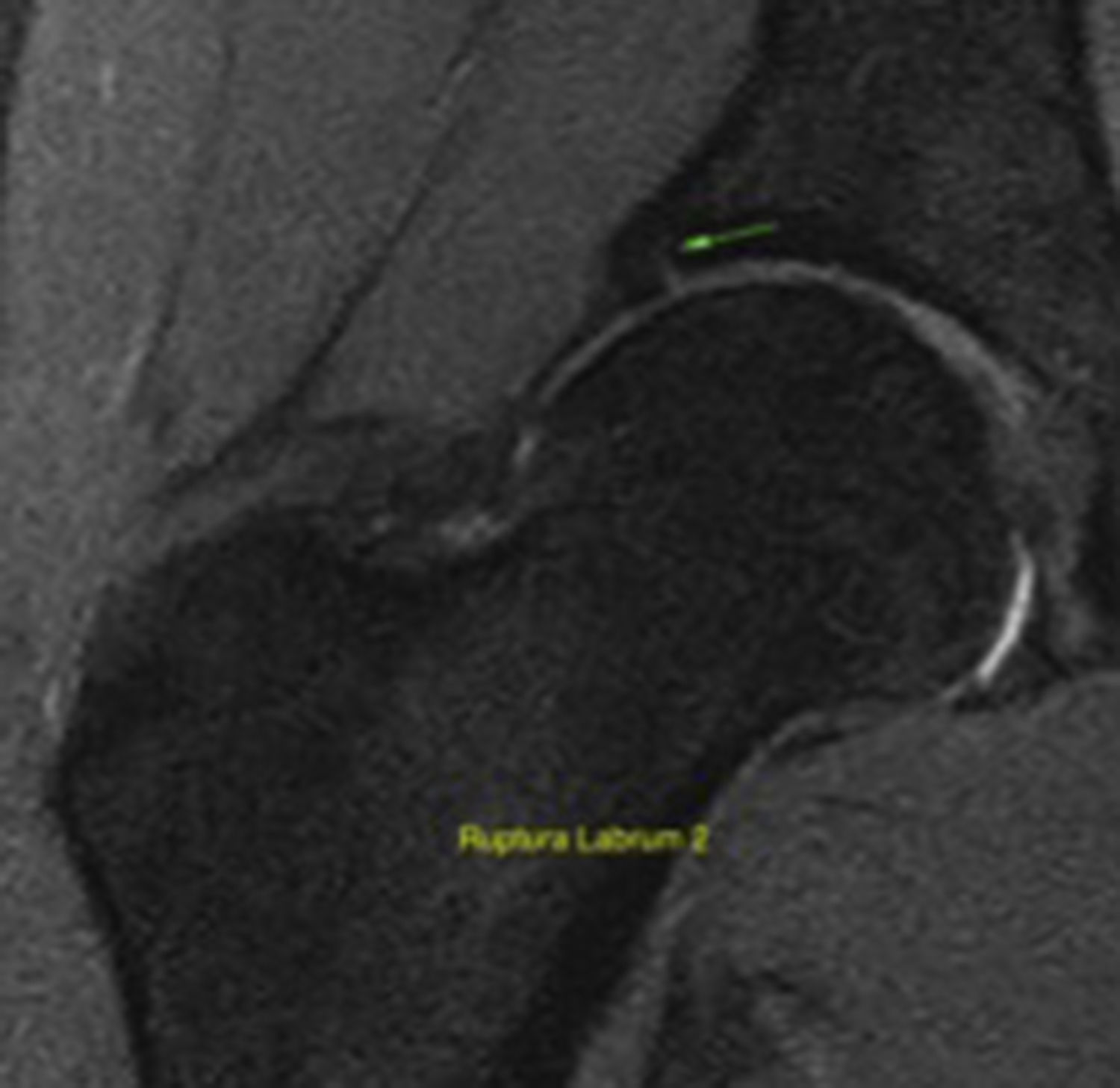
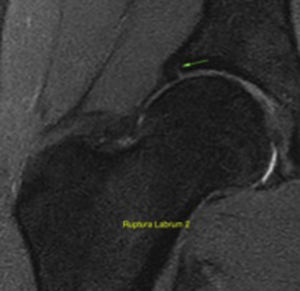
To evaluate the labral lesions by MRI as the method of choice to identify soft tissue lesions around the hip, including the labrum and the cartilage, we used the following simplified classification: stage 0 normal, 1 intrasubstance degeneration, 2 partial tear, and 3 complete tear.
The Outerbridge classification system was used for the cartilage lesions, widely described in the literature, with a scale of 0–4, 0 being normal cartilage and 4 complete wear of the cartilage with exposure of subchondral bone.24,25
Statistical analysisA sample of 42 subjects was calculated (84 hips) for which a 40% frequency of labral lesions was taken into account (stages 2B, 3A and 3B), 7% precision and 95% confidence of a total population of 150 footballers. The Kolmogorov–Smirnov and Shapiro–Wilk tests were used to assess whether the distribution of the quantitative variables, in the entire sample and in the different subgroups, came from a population with normal distribution.
The nominal qualitative variables were described using frequencies and proportions. The quantitative variables with normal distribution were described by means and standard deviation; medians and interquartile range were used for the quantitative variables with non-normal distribution.
The Student's t-test or Mann–Whitney U test were used to determine whether there were differences between the footballers with chondrolabral lesions of the hip and those without. The χ2 test of independence was used to establish the relationship between anatomical variances and the presence of chondrolabral lesions.
A 5% level of statistical significance was implemented for all the analyses, and SPSS version 21.0 was used.
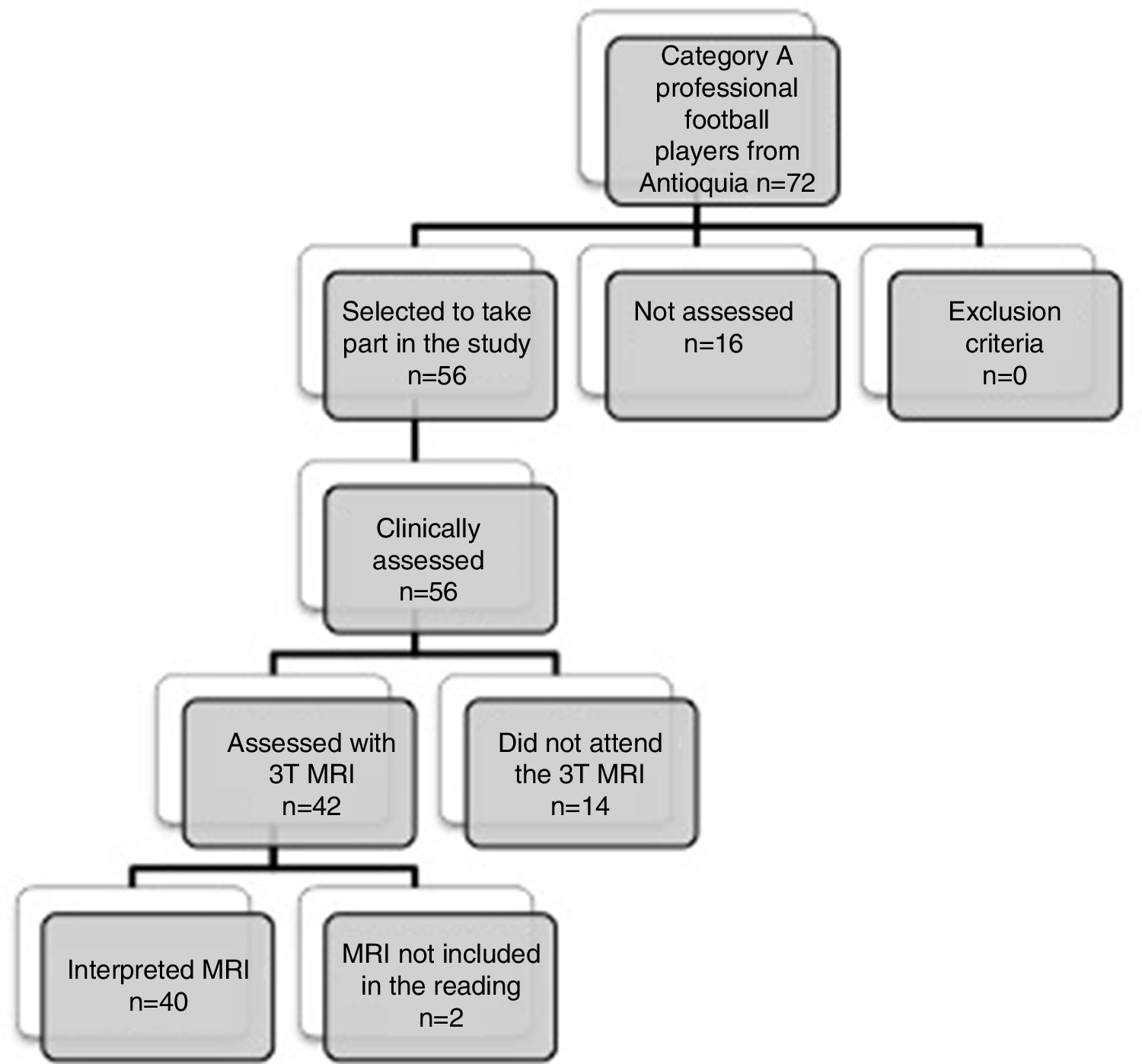
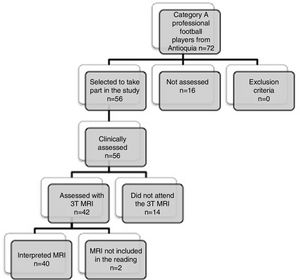
ResultsCharacteristics of the sample studiedOf a total of 72 players from 3 professional football teams in Antioquia of category A (coded as A, B and C), 56 footballers were contacted, who agreed to participate in the study and were clinically assessed by the orthopaedic specialist in charge. Forty-two footballers underwent MRI assessment of both hips (Fig. 1).
Team B had the highest number of footballers in the sample, at 22 (50%). The mean overall age was 23.4±4.1 years, BMI was 23.9±1.3kg/m2 and body fat percentage (% BF) was 9±2.7%. Forty-five percent of the sample were mixed race (n=18), and 70% had completed high school (n=28). The right leg was dominant in the majority of the footballers (72.5%). The average age of starting the sport was 7.8±3 years, and of starting to play it professionally was 17.4±1.7 years. Depending on the position, the majority of the sample were midfielders, at 47.5% (n=19), and there were fewer strikers in the sample at 7.5% (n=3).
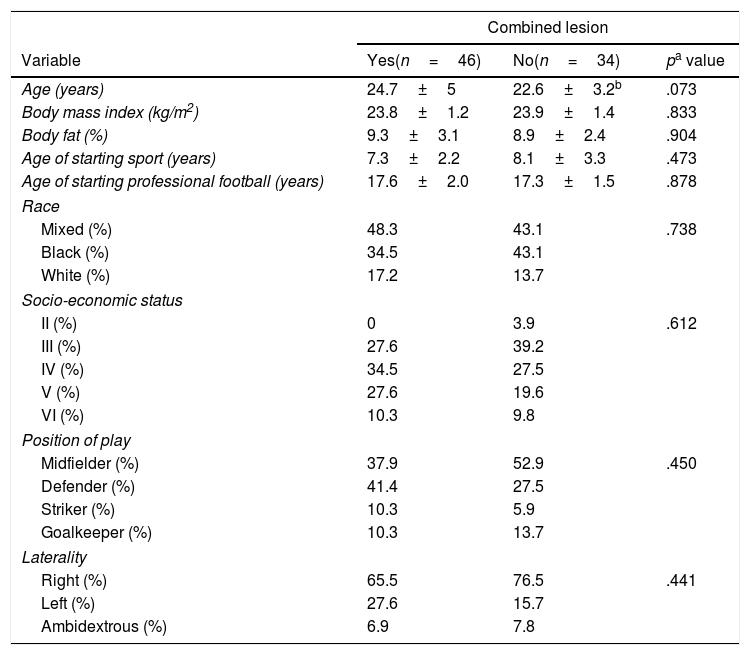
No differences were found in terms of team, race, level of education, socio-economic level, position of play or laterality with regard to the presence of chondrolabral lesions (Table 1).
Comparison of socio-demographic variables and the presence of a combined lesion (labral or acetabular or femoral cartilage or chondrolabral lesion).
| Combined lesion | |||
|---|---|---|---|
| Variable | Yes(n=46) | No(n=34) | pa value |
| Age (years) | 24.7±5 | 22.6±3.2b | .073 |
| Body mass index (kg/m2) | 23.8±1.2 | 23.9±1.4 | .833 |
| Body fat (%) | 9.3±3.1 | 8.9±2.4 | .904 |
| Age of starting sport (years) | 7.3±2.2 | 8.1±3.3 | .473 |
| Age of starting professional football (years) | 17.6±2.0 | 17.3±1.5 | .878 |
| Race | |||
| Mixed (%) | 48.3 | 43.1 | .738 |
| Black (%) | 34.5 | 43.1 | |
| White (%) | 17.2 | 13.7 | |
| Socio-economic status | |||
| II (%) | 0 | 3.9 | .612 |
| III (%) | 27.6 | 39.2 | |
| IV (%) | 34.5 | 27.5 | |
| V (%) | 27.6 | 19.6 | |
| VI (%) | 10.3 | 9.8 | |
| Position of play | |||
| Midfielder (%) | 37.9 | 52.9 | .450 |
| Defender (%) | 41.4 | 27.5 | |
| Striker (%) | 10.3 | 5.9 | |
| Goalkeeper (%) | 10.3 | 13.7 | |
| Laterality | |||
| Right (%) | 65.5 | 76.5 | .441 |
| Left (%) | 27.6 | 15.7 | |
| Ambidextrous (%) | 6.9 | 7.8 | |
The data are presented as mean±standard deviation as appropriate.
Thirty-five percent (n=14) of the players reported a history of hamstring injury, 10% (n=4) quadriceps injury, 10% (n=4) adductor injury, 12.5% (n=5) had suffered pubalgia and 17.5% (n=7) backache. Only one of the participants reported inguinal pain and none of them reported coxalgia during activities of daily living.
With regard to the physical examination, the FABER test was positive for 40% of the players, and present in the right side in 17.5% (n=7), bilateral in 2.5% (n=1) and present in the left side in 20% (n=8). The FADDIR test was positive for 20% of the subjects, 12.5% (n=5) on the left side and bilateral in 7.5% (n=3). Both external and internal coxa saltans was present in 5% (n=2) of those assessed. None of the footballers had a positive log-roll sign. With regard to the arcs of movement, the mean for internal rotation and abduction of the right hip was 24.5±11 degrees and 81.5±8.4 degrees, respectively. The mean internal rotation of the left hip was 30.8±9.8 degrees and abduction was 80.9±8.9 degrees.
3T magnetic resonance assessmentBoth hips of the 40 participating players were assessed by 3T MRI; therefore we report the principal results for 80 hips.
With regard to the type of FAI, there was a prevalence of 22.5% (n=18) of cam-type lesions, and of 1.3% of both pincer and mixed lesions (n=1) (Fig. 2). We found 33.8% labral lesions, and 18–8% (n=15) intrasubstance degeneration, 12.5% partial labral tear (n=10), and 2.5% complete labral tear (n=2) (Fig. 3). The prevalence of femoroacetabular cartilage lesions was 13.8% of the hips assessed, and we found acetabular cartilage lesions in 6.3% (n=5), this percentage was in turn distributed into 5% (n=4) with cartilage softening and oedema, and into 1.3% (n=1) with subchondral bone fissures >1.5 in diameter; 75% (n=6) had femoral cartilage lesions. An acetabular cyst was present in 5% (n=4) of the population. Chondrolabral damage was seen in 10% (n=8) and synovitis in 1.3% (n=1). Other findings were femoral head oedema in 5% (n=4), capsular or ligament thickening in 2.5% (n=2), coxa profunda in 17.5% (n=14) and labral or paralabral cyst in 1.3% (n=1). None of the players had cysts in the femoral head-neck union, round ligament impairment, retroversion or Os acetabuli.
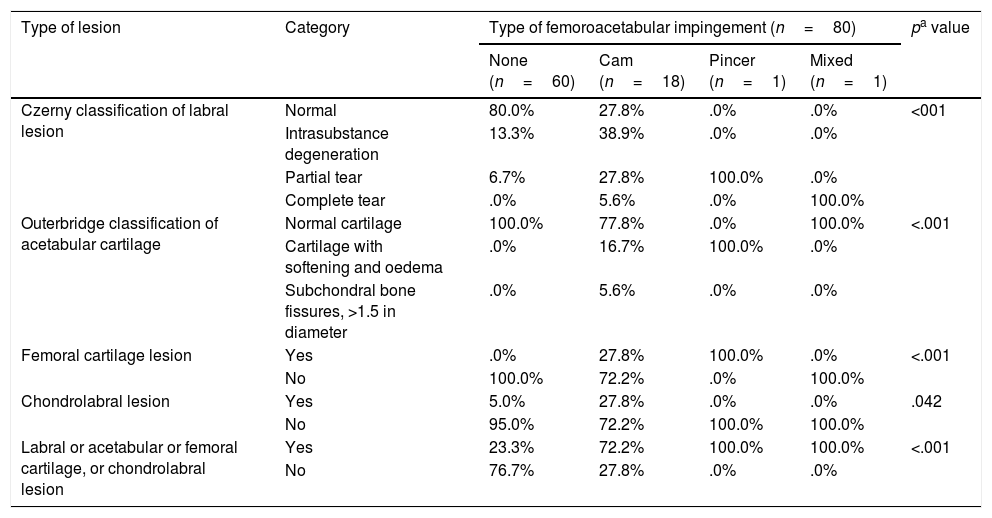
When the type of impairment was compared with the presence of impairments of the labrum and cartilage (alone or combined), a clear and significant association was found between cam-type FAI and the different lesions; therefore, of the hips studied that had cam configuration, 72% had lesions of the labrum (p<.001), 22.3% acetabular cartilage lesions (p<.001), 27.8% had femoral cartilage and chondrolabral lesions (p=.042), and 72.2% combined lesions (presence of labral, cartilage, acetabular, femoral, or chondrolabral lesion) with a p<.001 (Table 2).
Associations between the type of FAI and lesions of the labrum, acetabular cartilage, femoral cartilage, chondrolabral and combined lesion (labral or acetabular cartilage or femoral cartilage or chondrolabral lesion).
| Type of lesion | Category | Type of femoroacetabular impingement (n=80) | pa value | |||
|---|---|---|---|---|---|---|
| None (n=60) | Cam (n=18) | Pincer (n=1) | Mixed (n=1) | |||
| Czerny classification of labral lesion | Normal | 80.0% | 27.8% | .0% | .0% | <001 |
| Intrasubstance degeneration | 13.3% | 38.9% | .0% | .0% | ||
| Partial tear | 6.7% | 27.8% | 100.0% | .0% | ||
| Complete tear | .0% | 5.6% | .0% | 100.0% | ||
| Outerbridge classification of acetabular cartilage | Normal cartilage | 100.0% | 77.8% | .0% | 100.0% | <.001 |
| Cartilage with softening and oedema | .0% | 16.7% | 100.0% | .0% | ||
| Subchondral bone fissures, >1.5 in diameter | .0% | 5.6% | .0% | .0% | ||
| Femoral cartilage lesion | Yes | .0% | 27.8% | 100.0% | .0% | <.001 |
| No | 100.0% | 72.2% | .0% | 100.0% | ||
| Chondrolabral lesion | Yes | 5.0% | 27.8% | .0% | .0% | .042 |
| No | 95.0% | 72.2% | 100.0% | 100.0% | ||
| Labral or acetabular or femoral cartilage, or chondrolabral lesion | Yes | 23.3% | 72.2% | 100.0% | 100.0% | <.001 |
| No | 76.7% | 27.8% | .0% | .0% | ||
The χ2 test of Independence was used to establish the relationship between anatomical variances and the presence of chondrolabral lesions.
Level of statistical significance: p<.05.
Of the 60 hips that showed no type of impingement, it was found that 20% had labral lesions, none had acetabular or femoral cartilage lesions, 5% had chondrolabral lesions and 23.3% had combined lesions (presence of labral or acetabular cartilage or femoral cartilage or chondrolabral lesions) with a p<.001.
DiscussionThe presence of anatomical abnormalities indicative of FAI that predispose to labral and articular cartilage injuries of the hip is much more common in athletes than in the general population, with a reported prevalence ranging between 10% and 15%.2,12,26
In our study, the frequency of FAI found by 3T magnetic resonance was 25.1%, the cam type being the most prevalent, at 22.5%, followed by pincer and mixed impingement at 1.3% respectively. This is in line with other authors, who report the presence of cam-type deformities in footballers in between 26% and 68% of cases.27,28
The high prevalence of FAI, and more specifically cam-type deformities, found in adult elite athletes, could support the hypothesis proposed by various investigators who suggest that high training loads are associated with a higher frequency of anatomical variances and chondrolabral lesions, and that this dose-response ratio could be explained by the effect of not only the mechanical component of exercise, but also by genetic and nutritional factors, and hormonal regulation (principally growth hormone and insulin-like growth factor-1) that occur during the skeletal development phase, making the hip bones more sensitive to work load between the ages of 12 and 14.29–33
Early chondral and labral damage leads to progressive degeneration if the fundamental cause of the impingement is not corrected,34 with the obvious negative impact on athletes’ sporting performance. Therefore it is essential to detect and recognise radiological abnormalities in the configuration of the acetabulum and femoral head, and perform MRI imaging to assess lesions of the labrum and articular cartilage of the hip in susceptible patients, since these impairments are associated with an increased incidence of osteoarthritis.35
The literature reports labral impairments close to 70% and chondral defects of 24% for the general asymptomatic population,1 which increase with age and if they are located in the anterior area of the labrum. In symptomatic patients with a clinical diagnosis of FAI or labral defects, the prevalence of cartilage lesions is 76–88%.36,37
Attempts have been made to explain the high prevalence of labral tears in asymptomatic athletes8 as the consequence of isolated or repeated traumatic events.38 However, it is still not clear why some athletes with these injuries display no symptoms. Although this phenomenon has also been reported in non-athletes, it is assumed to be more likely that a chondrolabral hip lesion would cause symptoms in an elite athlete. A reasonable hypothesis might be that in some cases the symptoms might be mild or only occur with certain movements, which could result in athletes reporting them less for fear of being ruled out of competition. This observation is only theoretical and difficult to prove.
We found in our study that the anatomy of the hip is associated with lesions of the labrum and cartilage (isolated or combined) in asymptomatic professional footballers, and this association is irrespective of demographic variables such as race, socio-economic level, position of play or laterality because we found no differences between these variables and the presence or otherwise of chondrolabral lesions.
To our knowledge, this study is the first to evaluate with 3T MRI the prevalence of asymptomatic lesions of the labrum and articular cartilage of the hip in professional footballers and their association with the anatomical characteristics of FAI.
The results of this study enable us to establish that being a professional footballer constitutes an additional risk for the development of lesions of the labrum or articular cartilage in the context of femoracetabular anatomical malformations. If the various professionals who work with athletes take this into account it will enable preventive strategies to be established based on biomechanical, anatomical or clinical associations that might be identified.
Because cam and pincer-type deformities are predisposing factors for the mechanism of impingement that leads to progressive damage of the joint, encouraged by certain activities of impact and overuse, all strategies that seek to establish special risk groups are justified given the assumed greater prevalence of OA, with its implications for continuing sports activity, the individual's quality of life regardless of their sport, and the costs to the health system.
Limitations of the studyThis study has limitations in relation to its cross-sectional design, which does not enable a causal relationship to be established between the anatomical characteristics of the hip and the presence of chondrolabral lesions. Neither did we obtain previous radiological images or clinical history data that might have explained the results obtained, and the athletes were not followed up.
ConclusionThe prevalence of chondrolabral lesions was significant (57.6%) and distributed as 33.8% for labral lesions, 13.8% for femoroacetabular cartilage and 10% for chondrolabral lesions. Cam-type impingement was the most common FAI (22.5%). The anatomical characteristics of FAI of the hip are associated with lesions of the labrum and cartilage (isolated or combined) in asymptomatic professional football players.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interest to declare.
We would like to thank the Instituto de Alta Tecnología Médica (IATM) (Medellín, Colombia); doctors Édgar Alberto Méndez, Carlos Mario Muñoz and David Londoño, for their valuable collaboration, and the football clubs who participated, whose identity we will not disclose due to medical confidentiality.
Please cite this article as: Márquez WH, Gómez-Hoyos J, Gallo JA, Espinosa B, Rivas N, Llano JF, et al. Prevalencia de lesiones del labrum y del cartílago articular de la cadera en imagen por resonancia magnética simple 3 T de futbolistas profesionales asintomáticos. Rev Esp Cir Ortop Traumatol. 2019;63:77–85.