Life expectancy has risen, leading to an increase in acetabular fractures in fragile patients. Total hip arthroplasty with a reinforcement cage is a technically complex option, but allows fracture control and early mobilization. Our aim is to assess whether the use of Burch-Schneider cage in fragile patients with acetabular fractures allows immediate load stabilization without threatening the early survival of the arthroplasty.
Material and methodsDescriptive study of a series of 14 patients with acetabular fractures treated by a reinforcement cage associated with autologous bonegraft plus a cemented acetabular cup, and mobilization and bearing. Judet Letournel fracture types, surgical delay, and complications during admission were analyzed. Following hospital discharge we recorded the incorporation of grafts according to Gie’s classification, presence of calcifications according to Brooker, consolidation of the fracture, loosening of implants and functional aspects according to the HHS and Merlé D’Aubigné Postel score.
ResultsThe most common fracture was both columns (6/14), with a surgical delay being of 11 days mean and 21,5 days of length of stay. One patient died after surgery. The mean follow-up was 34.4 months. All fractures healed and the bonegraft was incorporated in all cases. The mean HHS was 82 points and the Merle Score was 15/18. There were no complications related to arthroplasty.
ConclusionsTotal hip arthroplasty with Burch-Schneider cage on bonegraft and no added osteosynthesis is a good option of treatment of all types of displaced acetabular fractures in a fragile patient.
El aumento de esperanza de vida está produciendo un incremento de fracturas de cotilo en el paciente anciano. La artroplastia total con anillo de refuerzo es una opción técnicamente compleja, pero permite el control de la fractura, la movilización y la deambulación precoz. Nuestro objetivo es valorar si el uso del anillo de Burch-Schneider en las fracturas de cotilo del paciente anciano permite la estabilización sin poner en riesgo la supervivencia precoz de la artroplastia.
Material y métodosEstudio descriptivo sobre una serie de 14 pacientes con fracturas de cotilo tratados mediante anillo de refuerzo asociado a autoinjerto más implante acetabular cementado e inicio precoz de movilización y deambulación. Se analizaron los tipos de fractura según la clasificación de Judet Letournel, la demora quirúrgica y las complicaciones durante el ingreso. Al alta se valoró la incorporación de injertos según la clasificación de Gie, la presencia de calcificaciones según Brooker, la consolidación de la fractura, la movilización de implantes y los aspectos funcionales según la escala de HHS y Merlé D’Aubigné Postel.
ResultadosLa fractura más frecuente fue la de ambas columnas (6/14), la demora quirúrgica media de 11 días y la estancia media de 21,5 días. Un paciente falleció en el postoperatorio inmediato. El seguimiento medio fue de 34,4 meses. Todas las fracturas consolidaron e incorporaron el injerto. El HHS medio fue de 82 puntos y el Merle Score de 15/18. No hubo complicaciones relativas a la artroplastia.
ConclusionesLa artroplastia primaria de cadera con anillo de BS sobre injerto sin osteosíntesis añadida es una buena opción en el tratamiento de todo tipo de fracturas de cotilo desplazadas en paciente frágil.
The increase in life expectancy together with the change in habits of the elderly has led to an increase in acetabular fractures at this age, which is currently the group with the highest frequency.1–3 Elderly patients have different characteristics in terms of morbidity and types of fracture,3–6 and therefore require a different therapeutic approach to that used in young patients, the main objectives being to reduce morbidity and mortality and hasten functional recovery. This requires the least aggressive and most functional treatment possible.
There are various therapeutic options for these fractures, but no a defined algorithm.1,6 Conservative treatment is limited to non-displaced fractures and for patients whose general condition contraindicates surgery.5 Osteosynthesis, the standard treatment in the young patient, due to its aggressiveness, the different characteristics of the fracture and lower bone quality entails high morbidity and mortality in the elderly7, and more failures with the need for short-term arthroplasty in more than half of cases.6,8–10
Total hip arthroplasty (THA) in the acute phase of a fracture is an increasingly used therapeutic option. A prosthetic model needs to be chosen to stabilise the fracture and support the acetabular implant, enabling early mobilisation and ambulation.7,11–16
The performance of osteosynthesis and arthroplasty in the same surgical procedure requires atypical osteosynthesis in most cases,5,13 because it is recommended to perform osteosynthesis and arthroplasty using the same surgical approach. Prosthetic acetabular cup models have been used that allow osteosynthesis through the holes in the cup, acting as a circular osteosynthesis plate.13 These are cementless cups whose primary stability is not always achieved, and whose results have been inferior to cemented cups which appear to be the most suitable option.17 Rings and cages are used in hip revision surgery with severe defects, even with pelvic disruption,18,19 which is often the case in acetabular fractures in the elderly. These implants allow stabilisation of the disruption without added osteosynthesis serving as a support for a cemented cup. They seem to be a suitable option, simpler and less aggressive than other options. There are few publications on these techniques, and they have short series, but they have encouraging results that will need to be confirmed in the long term.5,6,12,16,20–22
Our objective was to study whether the Burch-Schneider (BS) cage, without added osteosynthesis, provides immediate stability to all types of acetabular fractures in the elderly, and simultaneously serves as a support for a cemented cup of a hip arthroplasty that enables immediate weight-bearing ambulation.
Material and methodsWe conducted an observational, descriptive, and retrospective study, that included patients diagnosed with acetabular fracture treated by THA in the acute phase of the fracture, with the following inclusion and exclusion criteria.
Inclusion criteria:
- -
Over 55 years of age.
- -
Diagnosis of acetabular fracture with displacement greater than 5 mm, due to high or low energy injury.
- -
Surgical treatment in the acute phase of the fracture by THA with Burch-Schneider® cage (Zimmer®, Etupes, Francia) cup cemented over the cage and cemented or cementless stem.
- -
Follow-up of more than 6 months.
- -
Patient walking prior to the fracture.
Exclusion criteria:
- -
Under 55 years of age.
- -
Conservative treatment or treatment by open reduction and osteosynthesis.
- -
Treatment with secondary THA due to sequelae of acetabular fracture.
- -
Patient not walking prior to the fracture.
- -
Loss to follow-up.
Initial diagnosis of the fracture was by plain X-ray in anteroposterior, alar oblique, and obturator view, and CT scan. The clinical and socio-demographic characteristics of the patients were collected: sex, age, anaesthetic risk (ASA), mechanism of production, laterality, blood test data on admission and 24 h after surgery, and type of fracture according to the Judet Letournel classification.23
We identified a total of 14 patients, of whom one died in the immediate postoperative period. Eight were male (57%) and 6 female (43%), with a mean age of 71.6 years (range: 55-88 years). The ASA of the patients was within the range 2-3 in all cases.
The mechanism of injury was high energy in 5 cases (4 traffic accidents, one collision), and low energy in 9 cases (fall to the ground from standing). The injury affected the right side in 6 cases and the left in 8 cases.
On admission, the fracture was reduced under sedation, lateralising the root of the thigh by manipulation in the case of central protrusion of the femoral head and supracondylar femoral skeletal traction between 5 kg and 7 kg was maintained until surgery. Prophylaxis for thromboembolic disease was 40 mg of subcutaneous low molecular weight heparin every 24 h, and 3 doses/1 g of cefazolin/every 8 h were used for infection, as we use for elective hip arthroplasty, starting 30 min before the prosthetic surgery. Three surgeons experienced in both hip revision surgery and pelvic fractures operated on all the patients, under general anaesthesia in each case. The surgical technique was similar in all cases, following the same protocol using a direct lateral Hardinge Bauer approach, osteotomy of the femoral neck without prior dislocation of the femoral head so as not to increase fracture displacement, removal of the femoral head using a corkscrew, reduction of the fracture with direct visualisation of the cup by means of instrumented manipulation of fragments as far as possible without seeking anatomical reduction, careful resection of the acetabular cartilage using an acetabular reamer, filling of the acetabular floor with crushed and compacted autologous graft of the femoral head, implantation of a titanium BS cage screwed on the roof of the acetabulum and iliac bone and ischial anchorage, and cemented "all-poly" cup type Müller® (Zimmer®, Winterthur, Switzerland) on the cage. Cemented Exeter® (Stryker Inc®, Newbury, UK) femoral stem in 8 patients and cementless Sl-Plus® (Smith & Nephew Orthopaedics® AG, Switzerland) in 5 depending on their bone quality. We used a 32 mm head and polyethylene metal torque in all cases.
Sitting was allowed in all cases after 24 h and weight-bearing ambulation with 2 crutches from postoperative day 2.
The duration of the operation, blood loss by haematocrit and haemoglobin (Hb), the need for transfusion, the start of weight-bearing ambulation and the complications that arose were studied during the patients’ admission. Their clinical and radiological examination was performed on an outpatient basis one month after surgery, at 3 and 6 months, which was the minimum follow-up. The final functional results were assessed with the Harris Hip Score (HHS) 24 and the Merle d'Aubigné & Postel Score25; and on plain radiology, the incorporation of grafts using Gie’s scale (a scale that includes 3 grades from no changes compared to the first X-ray "grade 1" to complete trabecular remodelling "grade 3"),26 and periprosthetic ossifications according to the Brooker scale.27
We performed a hypothesis test on the influence of fracture type on functional outcomes using the Kruskal-Wallis test for quantitative variables. We used SPSS® version 17.0 software (Chicago, USA) for the statistical analysis.
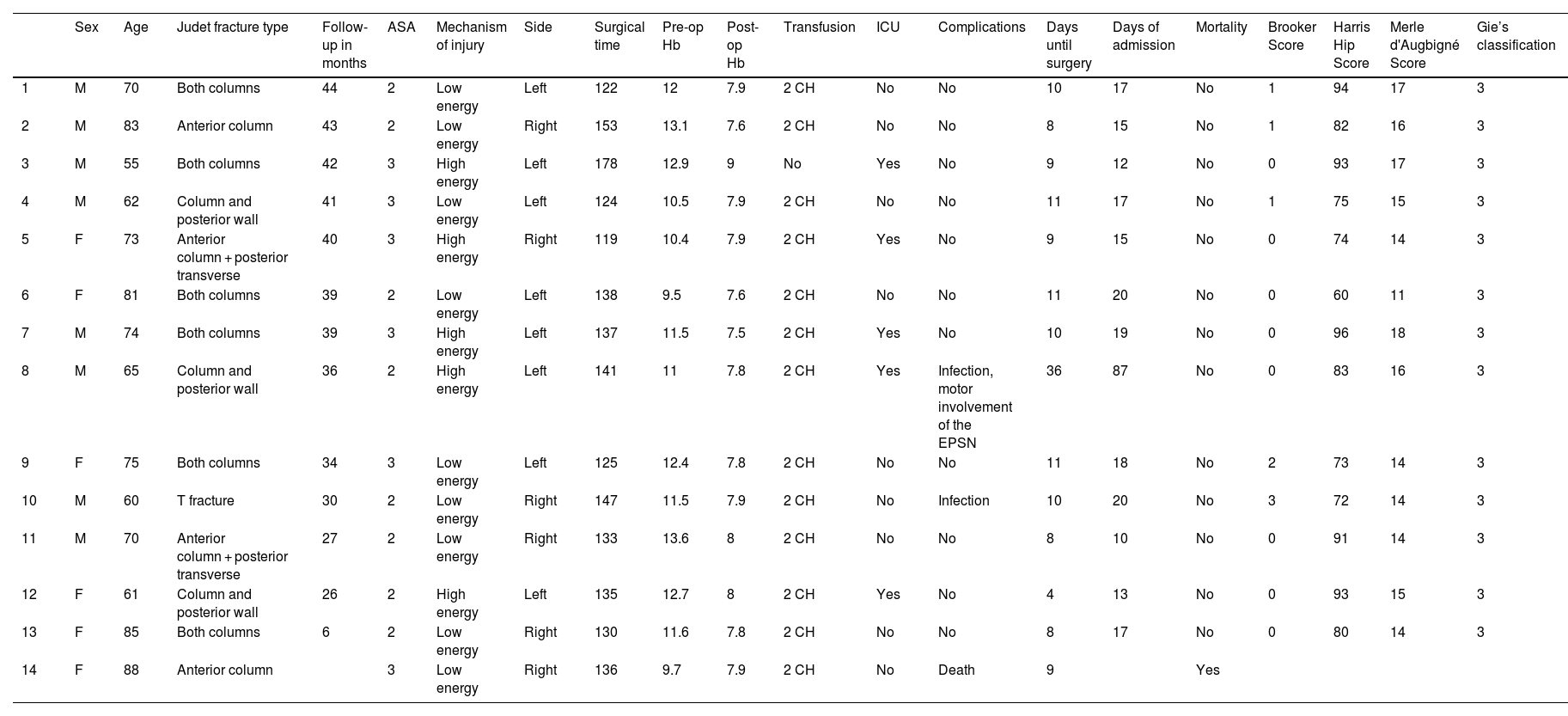
ResultsTable 1 summarises the patients’ most relevant demographic and clinical data. The fractures were classified according to the Judet Letournel classification. The most frequent fracture type was both columns in 6 cases, followed by column and posterior wall in 3 cases, and anterior + posterior transverse column in 2 cases.
Demographic and clinical data of the patients.
| Sex | Age | Judet fracture type | Follow-up in months | ASA | Mechanism of injury | Side | Surgical time | Pre-op Hb | Post-op Hb | Transfusion | ICU | Complications | Days until surgery | Days of admission | Mortality | Brooker Score | Harris Hip Score | Merle d'Augbigné Score | Gie’s classification | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 70 | Both columns | 44 | 2 | Low energy | Left | 122 | 12 | 7.9 | 2 CH | No | No | 10 | 17 | No | 1 | 94 | 17 | 3 |
| 2 | M | 83 | Anterior column | 43 | 2 | Low energy | Right | 153 | 13.1 | 7.6 | 2 CH | No | No | 8 | 15 | No | 1 | 82 | 16 | 3 |
| 3 | M | 55 | Both columns | 42 | 3 | High energy | Left | 178 | 12.9 | 9 | No | Yes | No | 9 | 12 | No | 0 | 93 | 17 | 3 |
| 4 | M | 62 | Column and posterior wall | 41 | 3 | Low energy | Left | 124 | 10.5 | 7.9 | 2 CH | No | No | 11 | 17 | No | 1 | 75 | 15 | 3 |
| 5 | F | 73 | Anterior column + posterior transverse | 40 | 3 | High energy | Right | 119 | 10.4 | 7.9 | 2 CH | Yes | No | 9 | 15 | No | 0 | 74 | 14 | 3 |
| 6 | F | 81 | Both columns | 39 | 2 | Low energy | Left | 138 | 9.5 | 7.6 | 2 CH | No | No | 11 | 20 | No | 0 | 60 | 11 | 3 |
| 7 | M | 74 | Both columns | 39 | 3 | High energy | Left | 137 | 11.5 | 7.5 | 2 CH | Yes | No | 10 | 19 | No | 0 | 96 | 18 | 3 |
| 8 | M | 65 | Column and posterior wall | 36 | 2 | High energy | Left | 141 | 11 | 7.8 | 2 CH | Yes | Infection, motor involvement of the EPSN | 36 | 87 | No | 0 | 83 | 16 | 3 |
| 9 | F | 75 | Both columns | 34 | 3 | Low energy | Left | 125 | 12.4 | 7.8 | 2 CH | No | No | 11 | 18 | No | 2 | 73 | 14 | 3 |
| 10 | M | 60 | T fracture | 30 | 2 | Low energy | Right | 147 | 11.5 | 7.9 | 2 CH | No | Infection | 10 | 20 | No | 3 | 72 | 14 | 3 |
| 11 | M | 70 | Anterior column + posterior transverse | 27 | 2 | Low energy | Right | 133 | 13.6 | 8 | 2 CH | No | No | 8 | 10 | No | 0 | 91 | 14 | 3 |
| 12 | F | 61 | Column and posterior wall | 26 | 2 | High energy | Left | 135 | 12.7 | 8 | 2 CH | Yes | No | 4 | 13 | No | 0 | 93 | 15 | 3 |
| 13 | F | 85 | Both columns | 6 | 2 | Low energy | Right | 130 | 11.6 | 7.8 | 2 CH | No | No | 8 | 17 | No | 0 | 80 | 14 | 3 |
| 14 | F | 88 | Anterior column | 3 | Low energy | Right | 136 | 9.7 | 7.9 | 2 CH | No | Death | 9 | Yes |
ASA: Anaesthetic risk; EPSN: External popliteal sciatic nerve; F: Female; Hb: Haemoglobin; ICU: Intensive Care Unit; M: Male; RBC: Red blood cell count.
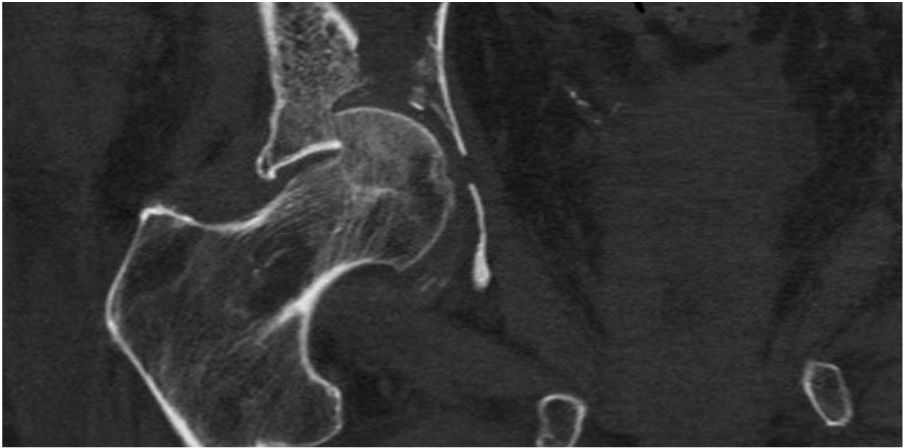
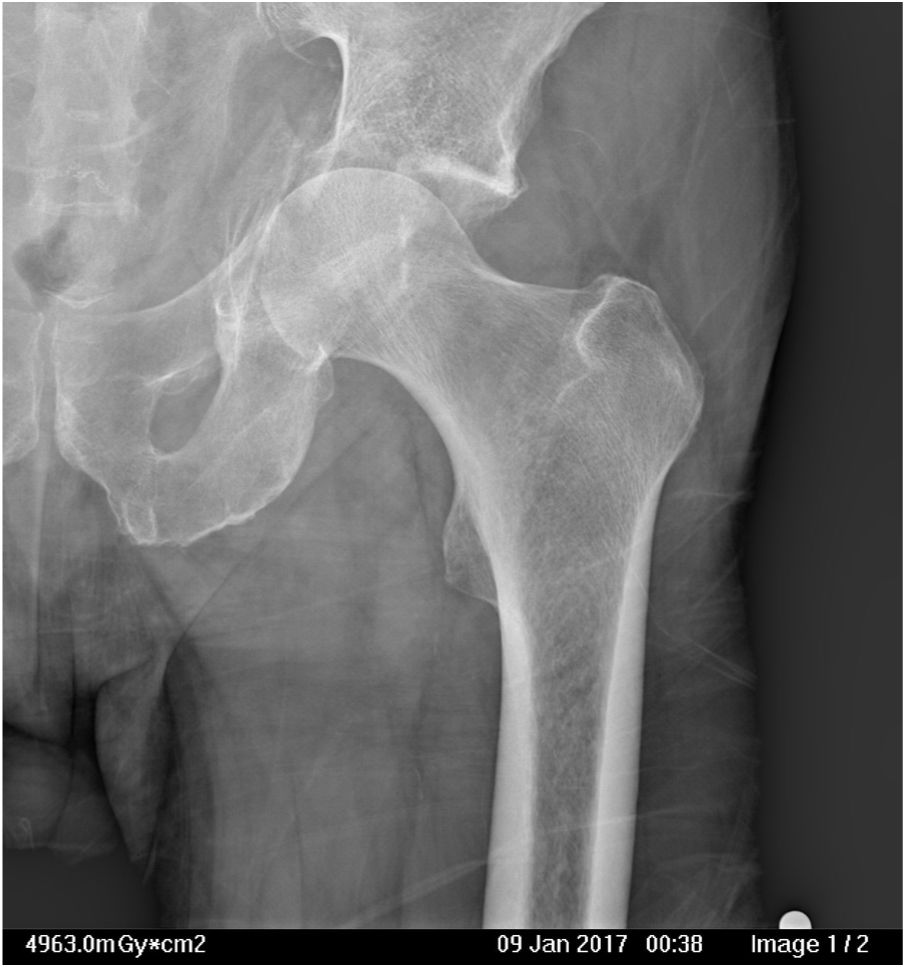
The most frequent injuries encountered were acetabular roof collapse (Fig. 1), fracture of the quadrilateral lamina with central protrusion of the femoral head (Fig. 2), and fracture of the femoral head (Fig. 1).
The mean operative delay was 11 days, ranging from 4 to 36 days, and the patients’ mean length of hospital stay from admission to discharge was 21.5 days (10-87).
The mean duration of surgery was 137 min (120-180). In terms of blood loss, with a mean Hb of 11.6 mg/dl on admission, postoperative Hb levels were a mean of 7.9 mg/dl, requiring postoperative blood transfusion in all but one patient.
There were no operative complications. One patient died during the immediate postoperative period, 2 patients had an acute infection that required lavage and debridement with antibiotic treatment and the infection resolved and one also suffered motor involvement of the EPSN that resolved over a period of 9 months. Weight-bearing ambulation with crutches took place on average after 3.4 days.
The mean follow-up of the patients was 34.4 months (6-44). The mean final HHS was 82 points, and the Merle D’Aubigné Score was 15/18. Five patients had excellent results (90-100 points), 3 good results (80-89 points), 4 patients had acceptable results (70-79 points), and one had a poor result (less than 70 points). Twelve patients recovered their pre-fracture life activities. No episodes of dislocation occurred, and no patient required reoperation during follow-up.
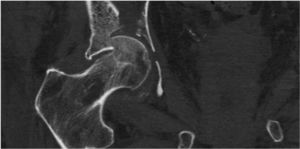
Radiological evaluation showed fracture healing in all patients, and we observed no complications such as screw breakage, implant displacement or mispositioning of the acetabular component. All patients had Gie’s grade 3 osseointegration (Fig. 3), 3 patients had grade I heterotopic calcifications according to Brooker’s classification, one grade II and one grade III, which did not result in functional limitation in any of the cases.
We analysed the influence of the type of fracture on results and complications using the Kruskal-Wallis test for small samples. We concluded that, according to the results of the sample, the use of the cage homogenises functional results and we found no significant differences in the scores of the functional tests, regardless of the type of fracture for which it was used (HHS p = .743; Merle p = .603), with the limitations of these low-power tests.
DiscussionIn recent decades, due to increased life expectancy, there has been a change in the habits of the ageing population towards greater physical activity. Acetabular fractures, classically typical in young patients, are now more frequent in the elderly,1,5 although their frequency is lower than hip fractures, and therefore experience in treating them is much more limited2 and published series are much shorter, both in the number of patients and follow-up times, and, as in our series, do not usually exceed 10-15 patients and 3-4 years of follow-up.5,6,12,16,20–22 Their characteristics are different both in terms of the type of patient and the type of fracture.3–6 Older patients usually have a history of multiple morbidity and high risk to life, with poor bone quality. Fractures usually occur over time by a low energy mechanism with trauma to the greater trochanter, which due to femoral anteversion, produces a fracture by collapse of the acetabular roof, fracture of the quadrilateral lamina and of the anterior wall and column with central dislocation of the femoral head.2,6,28 In other words, different characteristics to those of the young patient in whom fractures of the column and posterior wall are more frequent.14 This means that, if the elderly patient is different and the fractures are also different, the therapeutic tactic must also be different.5 The objective of treatment must be the survival of the patient and their return to pre-fracture functionality as early as possible. We must therefore opt for a treatment that minimises morbidity and mortality and allows immediate weight-bearing ambulation.14
Conservative treatment has a high mortality rate1,9,28 and more than half the patients treated with osteosynthesis require an arthroplasty in under 1.5 years,6,9,10 since correct reduction is not achieved in half these cases,5,8,29 and if it is also verified by CT, it is practically never achieved.30 When arthroplasty is performed in the sequelae phase on a fracture of the acetabulum that had been treated by osteosynthesis, the results are much poorer,5,31,32 and there are even reoperation figures of around 30% at 10 years, in most cases due to loosening.17 Given the absence of a longer follow-up period in our series, we have seen no evidence of loosening in any patient so far. Therefore, conservative treatment and osteosynthesis do not seem to be therapeutic options for acetabular fractures in the elderly,5 especially in those fractures that have a worse prognosis because they are difficult to reduce, such as fractures with anterosuperior collapse of the acetabular roof,3,6,8,10,28 and fractures associated with fractures of the column and anterior wall, both of which are extremely common in the elderly and present in practically all the patients in our series.
Manson et al.33 found that functional results in the elderly are poor and the same in patients treated conservatively or by osteosynthesis, and therefore above the age of 60 years they indicate treatment by hip arthroplasty, even extending this indication to younger patients in whom anatomical reduction is not possible due to the characteristics of the fracture. In other words, primary arthroplasty is increasingly indicated in the treatment of acetabular fractures, not only because of the characteristics of the patient and their age, but also due to the characteristics of the fracture and the possibility of reducing it.
Arthroplasty has difficulties, as fracture stabilisation and arthroplasty implantation need to be performed simultaneously so that in all cases the patient can be mobilised and ambulate in the immediate postoperative period.14 Using 2 different approaches to performing the arthroplasty and osteosynthesis appears to be an aggressive option, although good results have been published with few complications.15 Like most authors, we prefer a single approach to perform osteosynthesis and arthroplasty.5,12,14,16,21,22 The most commonly used are the posterolateral approach of Kocher Langenbeck34 and the lateral approach of Hardinge Bauer,35 osteosynthesis of the fracture being possible with both approaches, sometimes atypically, depending on the type of fracture.5 The choice of approach depends on the characteristics of the fracture and, above all, on the surgeon’s preference 10, thus Jordá et al.13 use the anterior approach, stabilising the fracture and the arthroplasty using the same route without complications derived from the approach. Perfect reduction of the fracture is not necessary to stabilise the fracture,20,28 but the best possible reduction is recommended, which is simpler than in the classic techniques, as we have a visible cup, having already resected the femoral head.28 Once the fracture has been reduced as far as possible, the acetabular base should be carefully filled with crushed and compacted grafts from the femoral head, to promote consolidation of the fracture and increase the bone volume should the arthroplasty fail and revision surgery be required. Two options are possible to stabilise the fracture, either performing an osteosynthesis using plates and screws or using the prosthetic material itself to stabilise the fracture, which simplifies the surgery by achieving both the stability of the fracture and that of the prosthetic acetabular implant. In our case, we achieved fracture healing and radiological integration of the grafts in all cases, using the lateral approach and the BS cage for fracture stabilisation with no failures.
The cemented cup is currently the standard, as it adapts easily to all characteristics and is widely used with better results than uncemented cups.17 Simko et al.21 conducted a comparative study of primary arthroplasty associated with different types of fracture stabilisation, finding that the best technique is the cemented cup into an acetabulum-stabilizing cage with autografts; this technique is indicated due to its results in younger patients, excellent results have also been achieved by other authors,20 and we use this technique even in non-elderly patients whose fractures we have considered irreducible.
We have found important advantages using a BS cage, since once the fracture has been reduced and the grafts implanted in the acetabular bed, as well as protecting the grafts, the fracture is stabilised by means of the cage’s screws and its own structure, giving support to a cemented cup. In other words, it achieves all the surgical objectives with a single approach, minimising aggressive surgery in frail elderly patients.14,18 The role of the cage in these cases would be to distribute the forces to the periphery, bridging the fracture, and secondly to release compression of the graft that could compromise its incorporation.36 Biomechanical studies consider that the cage reduces the forces behind the cup by 47%, the screw holes being the areas of greatest risk of fatigue.37
Like other authors,12,16 we obtained good functional and radiological results at 3 years without complications or displacement of implants, practically all the patients treated were able to return to their pre-fracture activity. BS cages can also be implanted using any type of approach, which is an additional advantage. We used the lateral approach because it is more common and offers less possibility of dislocation. We delayed surgery by one to three weeks, like other authors,14 to reduce operative bleeding and reduce the symptoms from the trauma, so that mobilisation and ambulation can begin immediately after surgery; however, this delay can probably be reduced. All the patients treated required blood transfusion, more due to the characteristics of the fracture than due to the surgery, as all the surgery was performed using a single approach like that of a primary hip arthroplasty with little increase in surgical time.
Our study has limitations: 1) Firstly, it is a retrospective study and without a control group in which other techniques were used; 2) Due to the low frequency of this type of fracture, the number of patients is small and the follow-up is short; 3) The radiological assessment of graft incorporation could be subject to inter-observer bias and 4) Studies will be needed to extend the series and follow-up time, to confirm our results and the survival of the implants in the medium and long term.
In conclusion, according to the results of our study, the treatment of acetabular fractures by primary THA with a reinforcement cage and bone autograft provides stability for all types of cup fractures, allowing immediate weight-bearing ambulation, and has good results in terms of healing, graft incorporation and functionality.
Level of evidenceLevel of evidence III.
FundingThe authors declare that they received no external funding for this study.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sarasa-Roca M, Angulo-Castaño MC, Gómez-Vallejo J, Torres-Campos A, Lasierra-SanRomán JM, Albareda-Albareda J. Artroplastia total de cadera primaria en fractura de acetábulo en el paciente anciano. Rev Esp Cirug Ortop Traumatol. 2022;66:51–58.