Enhanced recovery after surgery (ERAS) constitutes a multimodal approach, based on available scientific evidence, that achieves better patient's functionality, reduces pain, and even lowers financial costs. The present consensus statement proposes the standards for the implementation of ERAS programmes to lumbar fusion surgery, a meant benchmark we call REPOC.
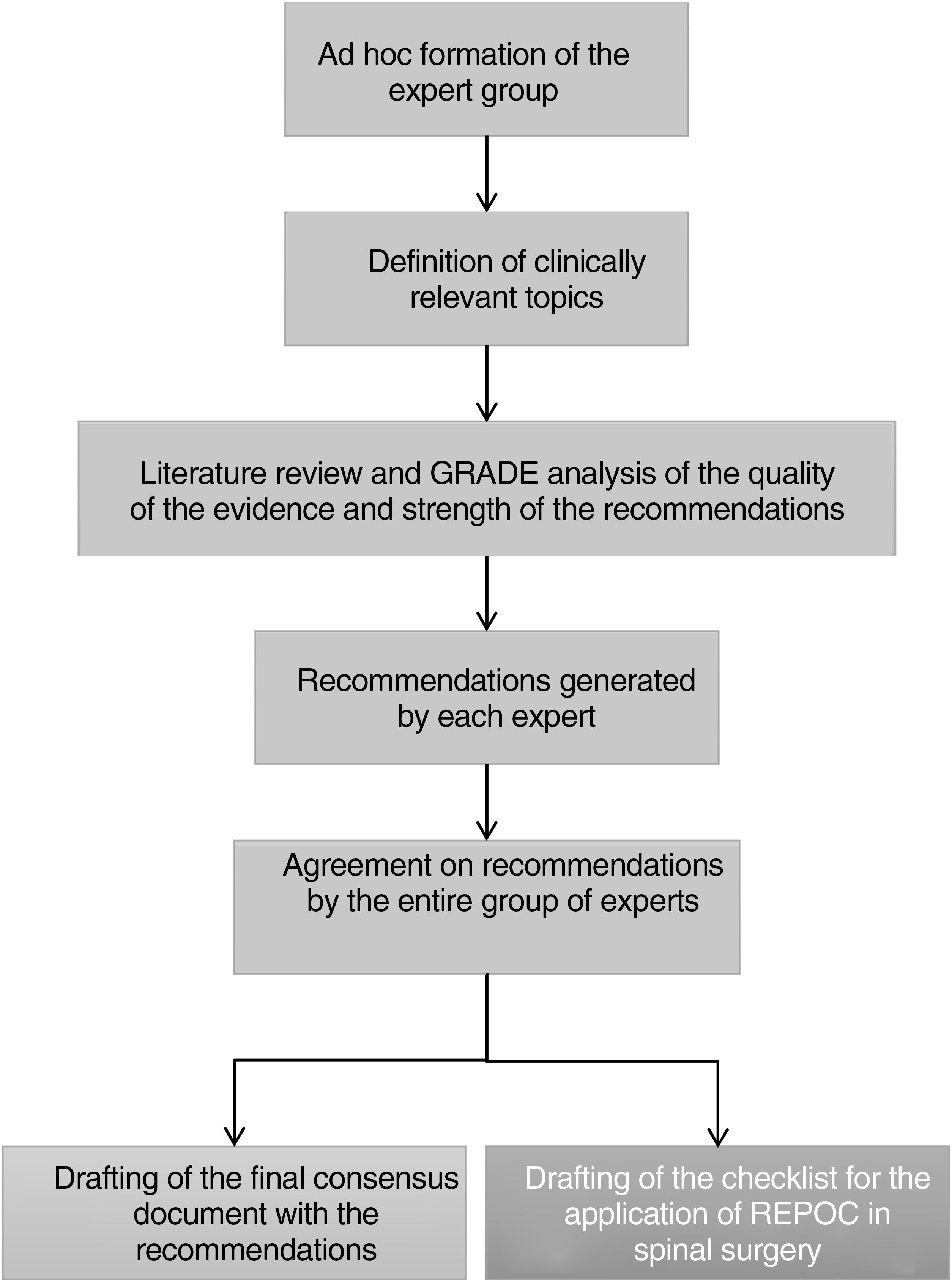
MethodologyA multidisciplinary group of experts was set up ad hoc to review consensus recommendations for lumbar arthrodesis, using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system.
ResultsAs a result, 23 recommendations were selected throughout the preoperative, intraoperative, and postoperative phases of the surgical procedure. A 29-item checklist was also drawn up to implement REPOC protocols in spinal surgeries.
ConclusionsThis list of recommendations will facilitate the implementation of this multimodal approach as a safe and effective tool for reducing adverse events in our environment.
La recuperación posquirúrgica optimizada en columna (REPOC) constituye un enfoque multimodal, basado en la evidencia científica disponible, que consigue una mejora eficaz de la funcionalidad fisiológica del paciente, reduce el dolor e incluso disminuye los costes hospitalarios. El objetivo de este trabajo es proponer unos estándares para la aplicación de la REPOC a la cirugía de fusión lumbar.
MétodosSe constituyó ad hoc un grupo multidisciplinario de expertos que revisaron la evidencia disponible y plantearon recomendaciones consensuadas para la artrodesis lumbar, utilizando el sistema Grading of Recommendations, Assessment, Development, and Evaluation (GRADE).
ResultadosSe seleccionaron 23 recomendaciones en las fases preoperatoria, intraoperatoria y postoperatoria de la intervención quirúrgica. También se elaboró una lista de 29 ítems para la aplicación de la REPOC en cirugía de columna.
ConclusionesEste listado de recomendaciones facilitará la implementación del enfoque REPOC como herramienta segura y eficaz para la reducción de los acontecimientos adversos en nuestro entorno.
Lumbar fusion surgery has been described as one of the most painful surgical procedures, with an increased risk of chronic pain and opioid dependence.1–6 Over recent decades, mainly due to the progressive ageing of the world's population, there has been a significant increase in the number of lumbar fusion surgeries, and in the complications, recovery delays, and costs associated with these procedures.2,3,7–9 The clinical practice of these interventions significantly varies between countries, with varying perioperative surgical outcomes, including mean length of hospital stay (LOS), postoperative complication rates and functional recovery rates.1–9 There is, therefore, a need for evidence-based, efficiency-enhancing standardisation in the management of the lumbar spinal fusion patient. We have named this standard REPOC – recuperación posquirúrgica optimizada en columna. This multimodal and multidisciplinary paradigm is based on the Enhanced Recovery After Surgery (ERAS) programmes,10 which have been successfully implemented in different surgical areas.1,2,4,11–14 These programmes have been successful in improving surgical outcomes and patient experience, and in reducing complications, opioid use, mean LOS and hospital costs.2–4,9,11–13,15–19
Despite the efforts made in recent years, high-quality prospective data for spinal surgery is lacking.4 There is a lack of specific guidelines and there are no standardised guidelines aimed at reducing perioperative stress, minimising complications, and accelerating hospital discharge.3,9,16–18 Achieving these goals would increase sustainability and reduce the environmental impact of these surgical interventions. The aim of the present paper is to review the available protocols for lumbar arthrodesis, develop a consensus list of recommendations, and propose an initial checklist for the implementation of REPOC for this type of surgery, focusing on patients undergoing single-level lumbar arthrodesis.
Material and methodsFor the first time in our country, a multidisciplinary group of experts, comprised equally of neurosurgeons and orthopaedic surgeons, was set up ad hoc to review procedures and draft consensus-based, evidence-based recommendations for the perioperative process of lumbar fusion surgery. We have named the resulting procedure REPOC: enhanced postoperative recovery in the spine.
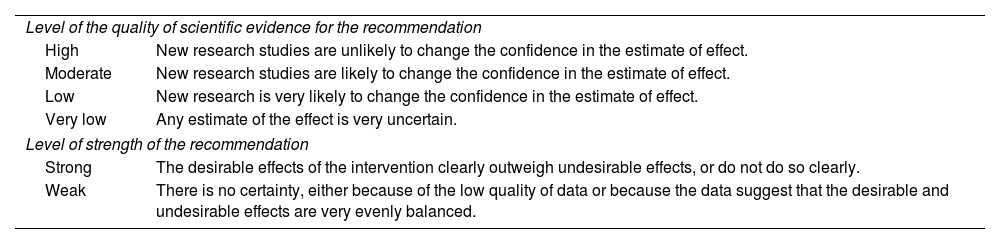
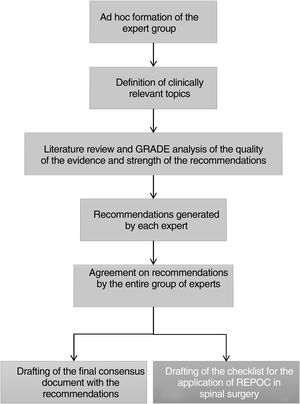
After defining the clinically relevant topics, the expert panel conducted a literature review and analysis of the quality of evidence and strength for each of the recommendations. The Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system20 was used for this analysis. This system classifies the scientific evidence for each recommendation as high, moderate, low, or very low; and the strength of the recommendation as strong or weak (Table 1). A specific REPOC recommendation can have a strong grade of recommendation, even if the quality of scientific evidence is low, if the risk of harm is negligible. The recommendations were selected following the guidelines for the development of clinical guidelines within the framework of the ERAS10 society. Fig. 1 graphically depicts the different stages in the development of this consensus document. Neither informed consent nor Ethics Committee approval was required.
GRADE system for rating the quality of scientific evidence and the strength of recommendations.20
| Level of the quality of scientific evidence for the recommendation | |
| High | New research studies are unlikely to change the confidence in the estimate of effect. |
| Moderate | New research studies are likely to change the confidence in the estimate of effect. |
| Low | New research is very likely to change the confidence in the estimate of effect. |
| Very low | Any estimate of the effect is very uncertain. |
| Level of strength of the recommendation | |
| Strong | The desirable effects of the intervention clearly outweigh undesirable effects, or do not do so clearly. |
| Weak | There is no certainty, either because of the low quality of data or because the data suggest that the desirable and undesirable effects are very evenly balanced. |
GRADE: Grading of Recommendations, Assessment, Development, and Evaluation.
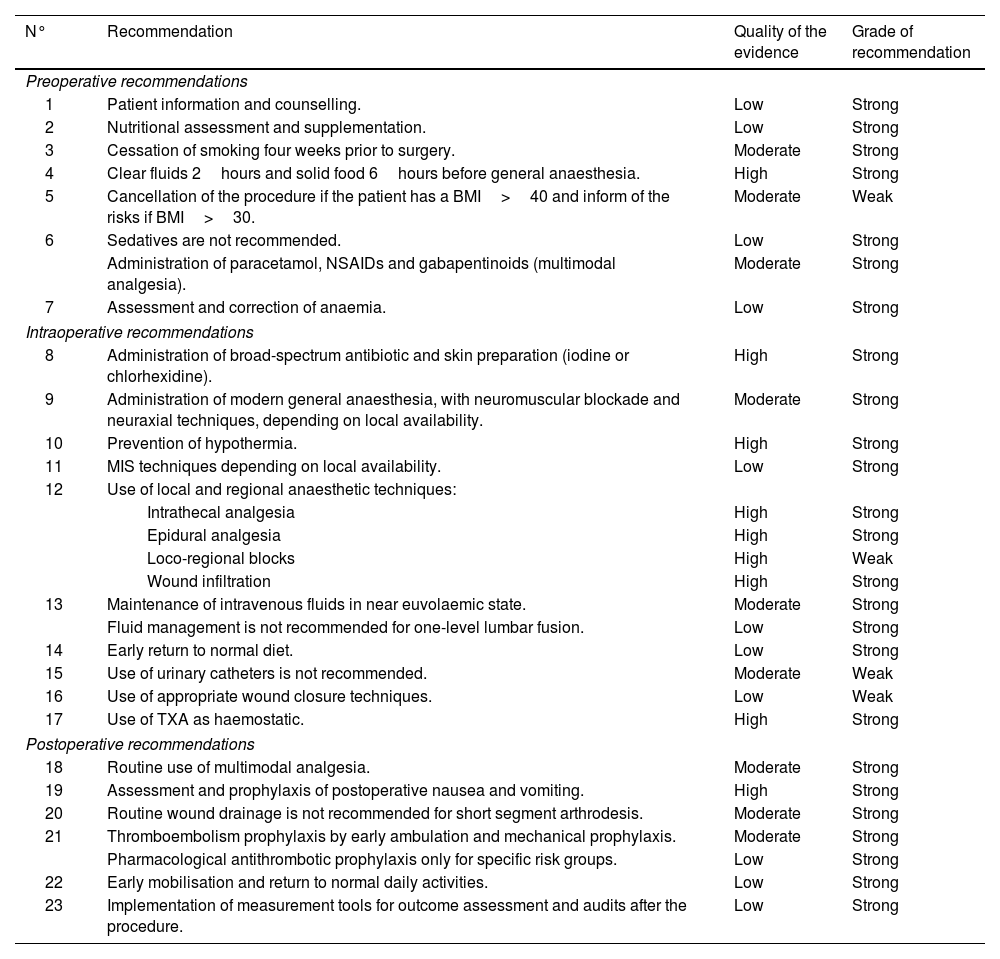
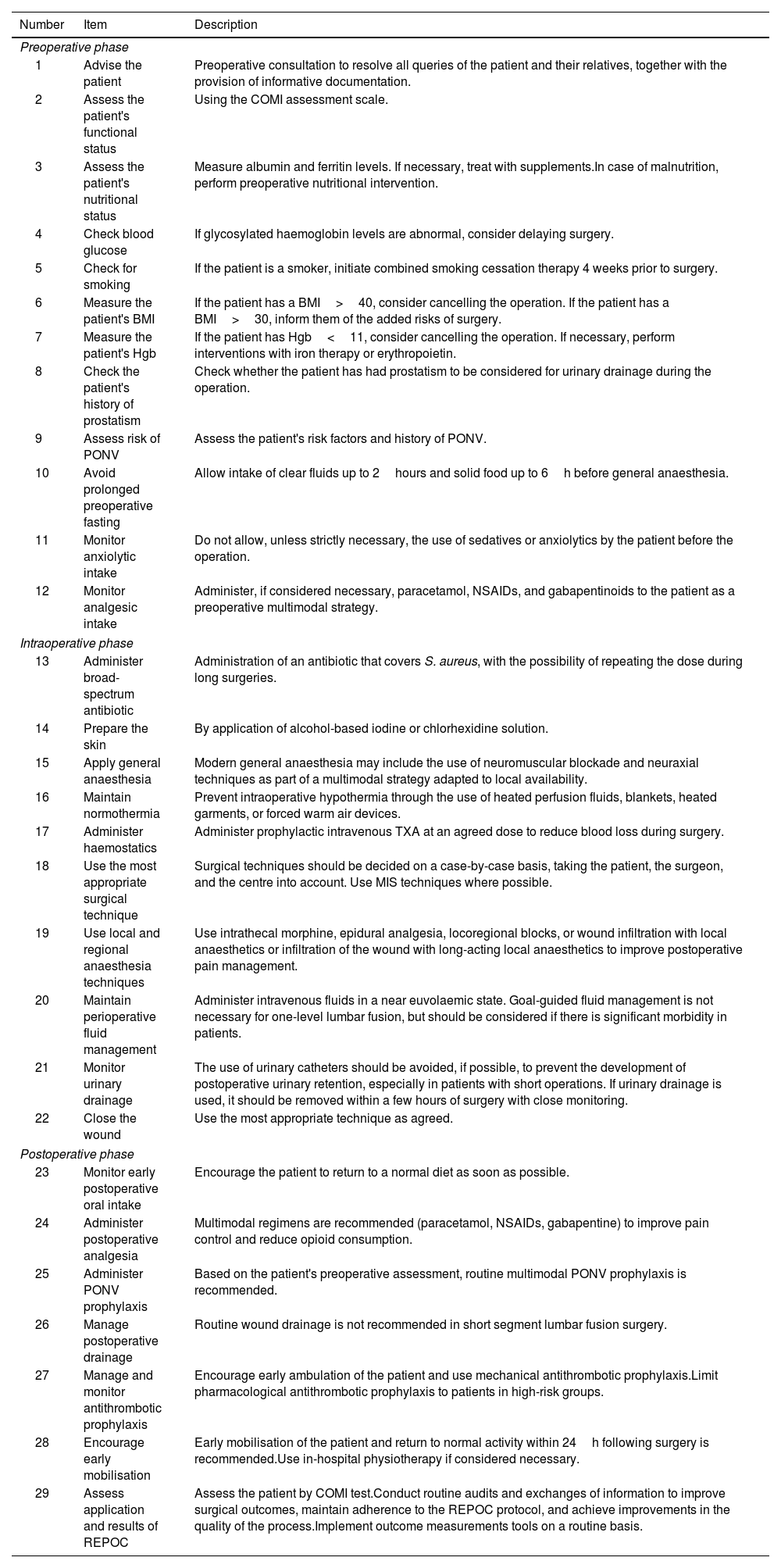
Concurrent with other studies,2,7,9,11,12,17,19 three phases (preoperative, intraoperative, and postoperative) were identified in which REPOC seeks to improve the care of the spinal surgery patient. With no major disagreements among the members of the expert group, this consensus document was drafted, and a checklist created that can be used by healthcare professionals involved in lumbar arthrodesis surgery. The 23 recommendations are summarised in Table 2. The 29 items of the checklist are listed in Table 3.
Summary of recommendations for perioperative care of spinal surgery according to the REPOC paradigm.
| N° | Recommendation | Quality of the evidence | Grade of recommendation |
|---|---|---|---|
| Preoperative recommendations | |||
| 1 | Patient information and counselling. | Low | Strong |
| 2 | Nutritional assessment and supplementation. | Low | Strong |
| 3 | Cessation of smoking four weeks prior to surgery. | Moderate | Strong |
| 4 | Clear fluids 2hours and solid food 6hours before general anaesthesia. | High | Strong |
| 5 | Cancellation of the procedure if the patient has a BMI>40 and inform of the risks if BMI>30. | Moderate | Weak |
| 6 | Sedatives are not recommended. | Low | Strong |
| Administration of paracetamol, NSAIDs and gabapentinoids (multimodal analgesia). | Moderate | Strong | |
| 7 | Assessment and correction of anaemia. | Low | Strong |
| Intraoperative recommendations | |||
| 8 | Administration of broad-spectrum antibiotic and skin preparation (iodine or chlorhexidine). | High | Strong |
| 9 | Administration of modern general anaesthesia, with neuromuscular blockade and neuraxial techniques, depending on local availability. | Moderate | Strong |
| 10 | Prevention of hypothermia. | High | Strong |
| 11 | MIS techniques depending on local availability. | Low | Strong |
| 12 | Use of local and regional anaesthetic techniques: | ||
| Intrathecal analgesia | High | Strong | |
| Epidural analgesia | High | Strong | |
| Loco-regional blocks | High | Weak | |
| Wound infiltration | High | Strong | |
| 13 | Maintenance of intravenous fluids in near euvolaemic state. | Moderate | Strong |
| Fluid management is not recommended for one-level lumbar fusion. | Low | Strong | |
| 14 | Early return to normal diet. | Low | Strong |
| 15 | Use of urinary catheters is not recommended. | Moderate | Weak |
| 16 | Use of appropriate wound closure techniques. | Low | Weak |
| 17 | Use of TXA as haemostatic. | High | Strong |
| Postoperative recommendations | |||
| 18 | Routine use of multimodal analgesia. | Moderate | Strong |
| 19 | Assessment and prophylaxis of postoperative nausea and vomiting. | High | Strong |
| 20 | Routine wound drainage is not recommended for short segment arthrodesis. | Moderate | Strong |
| 21 | Thromboembolism prophylaxis by early ambulation and mechanical prophylaxis. | Moderate | Strong |
| Pharmacological antithrombotic prophylaxis only for specific risk groups. | Low | Strong | |
| 22 | Early mobilisation and return to normal daily activities. | Low | Strong |
| 23 | Implementation of measurement tools for outcome assessment and audits after the procedure. | Low | Strong |
BMI: body mass index; MIS: minimally invasive surgery; NSAIDs: nonsteroidal anti-inflammatory drugs; REPOC: enhanced recovery after surgery; TXA: tranexamic acid.
Checklist for the implementation of REPOC in a lumbar arthrodesis surgical procedure.
| Number | Item | Description |
|---|---|---|
| Preoperative phase | ||
| 1 | Advise the patient | Preoperative consultation to resolve all queries of the patient and their relatives, together with the provision of informative documentation. |
| 2 | Assess the patient's functional status | Using the COMI assessment scale. |
| 3 | Assess the patient's nutritional status | Measure albumin and ferritin levels. If necessary, treat with supplements.In case of malnutrition, perform preoperative nutritional intervention. |
| 4 | Check blood glucose | If glycosylated haemoglobin levels are abnormal, consider delaying surgery. |
| 5 | Check for smoking | If the patient is a smoker, initiate combined smoking cessation therapy 4 weeks prior to surgery. |
| 6 | Measure the patient's BMI | If the patient has a BMI>40, consider cancelling the operation. If the patient has a BMI>30, inform them of the added risks of surgery. |
| 7 | Measure the patient's Hgb | If the patient has Hgb<11, consider cancelling the operation. If necessary, perform interventions with iron therapy or erythropoietin. |
| 8 | Check the patient's history of prostatism | Check whether the patient has had prostatism to be considered for urinary drainage during the operation. |
| 9 | Assess risk of PONV | Assess the patient's risk factors and history of PONV. |
| 10 | Avoid prolonged preoperative fasting | Allow intake of clear fluids up to 2hours and solid food up to 6h before general anaesthesia. |
| 11 | Monitor anxiolytic intake | Do not allow, unless strictly necessary, the use of sedatives or anxiolytics by the patient before the operation. |
| 12 | Monitor analgesic intake | Administer, if considered necessary, paracetamol, NSAIDs, and gabapentinoids to the patient as a preoperative multimodal strategy. |
| Intraoperative phase | ||
| 13 | Administer broad-spectrum antibiotic | Administration of an antibiotic that covers S. aureus, with the possibility of repeating the dose during long surgeries. |
| 14 | Prepare the skin | By application of alcohol-based iodine or chlorhexidine solution. |
| 15 | Apply general anaesthesia | Modern general anaesthesia may include the use of neuromuscular blockade and neuraxial techniques as part of a multimodal strategy adapted to local availability. |
| 16 | Maintain normothermia | Prevent intraoperative hypothermia through the use of heated perfusion fluids, blankets, heated garments, or forced warm air devices. |
| 17 | Administer haemostatics | Administer prophylactic intravenous TXA at an agreed dose to reduce blood loss during surgery. |
| 18 | Use the most appropriate surgical technique | Surgical techniques should be decided on a case-by-case basis, taking the patient, the surgeon, and the centre into account. Use MIS techniques where possible. |
| 19 | Use local and regional anaesthesia techniques | Use intrathecal morphine, epidural analgesia, locoregional blocks, or wound infiltration with local anaesthetics or infiltration of the wound with long-acting local anaesthetics to improve postoperative pain management. |
| 20 | Maintain perioperative fluid management | Administer intravenous fluids in a near euvolaemic state. Goal-guided fluid management is not necessary for one-level lumbar fusion, but should be considered if there is significant morbidity in patients. |
| 21 | Monitor urinary drainage | The use of urinary catheters should be avoided, if possible, to prevent the development of postoperative urinary retention, especially in patients with short operations. If urinary drainage is used, it should be removed within a few hours of surgery with close monitoring. |
| 22 | Close the wound | Use the most appropriate technique as agreed. |
| Postoperative phase | ||
| 23 | Monitor early postoperative oral intake | Encourage the patient to return to a normal diet as soon as possible. |
| 24 | Administer postoperative analgesia | Multimodal regimens are recommended (paracetamol, NSAIDs, gabapentine) to improve pain control and reduce opioid consumption. |
| 25 | Administer PONV prophylaxis | Based on the patient's preoperative assessment, routine multimodal PONV prophylaxis is recommended. |
| 26 | Manage postoperative drainage | Routine wound drainage is not recommended in short segment lumbar fusion surgery. |
| 27 | Manage and monitor antithrombotic prophylaxis | Encourage early ambulation of the patient and use mechanical antithrombotic prophylaxis.Limit pharmacological antithrombotic prophylaxis to patients in high-risk groups. |
| 28 | Encourage early mobilisation | Early mobilisation of the patient and return to normal activity within 24h following surgery is recommended.Use in-hospital physiotherapy if considered necessary. |
| 29 | Assess application and results of REPOC | Assess the patient by COMI test.Conduct routine audits and exchanges of information to improve surgical outcomes, maintain adherence to the REPOC protocol, and achieve improvements in the quality of the process.Implement outcome measurements tools on a routine basis. |
BMI: body mass index; COMI: care outcome measures index; Hgb: haemoglobin; MIS: minimally invasive surgery; NSAIDs: nonsteroidal anti-inflammatory drugs; PONV: postoperative nausea and vomiting; REPOC: enhanced recovery after surgery; TXA: tranexamic acid.
The aim of this phase is to assess and mitigate the potential risks of the intervention, and to maximise the physical and functional status of the patient.
Preoperative patient information and counsellingOur experience and studies show that counselling and informing the patient on surgical expectations increases their confidence and improves their mood. This reduces anxiety, fear and the stress response to lumbar surgery, which is often perceived as having an uncertain outcome, negative side effects, and a long recovery time.1–3,21 This phase can include functional assessment of the patient using the Core Outcome Measures Index (COMI) scale, which has proven useful in daily clinical practice for patients with degenerative lumber spine disease.22 Ideally, a national consensus information document should be available, although it should be adapted to local clinical characteristics in each centre. We believe the quality of evidence for this recommendation is low, but the grade of recommendation is strong (Table 2).
Preoperative nutritional supplementationAlthough malnutrition is considered a risk factor in many surgeries, there are no studies confirming its effect on the outcome of spinal surgery. A randomised clinical trial (RCT) associated nutritional supplementation before and after lumbar fusion surgery with shorter mean LOS, lower incidence of electrolyte imbalances, and higher postoperative albumin levels.23 This phase should include measurement of albumin and ferritin levels, and glycaemic control in diabetic patients. If there are imbalances, treatment with supplements and delaying surgery is recommended if glycosylated haemoglobin values are abnormal. At the local level, consensus should be reached with the nutrition and endocrinology department. The quality of scientific evidence for this recommendation is low, but the grade of recommendation is strong (Table 2).
Preoperative smoking cessationSmoking cessation before (four weeks) and after spinal surgery is associated with a reduction in postoperative complications.12,19,24 The patient's smoking status needs to be included in the initial assessment, advice on smoking cessation, and information on the risks. This recommendation is based on a moderate quality of scientific evidence, but we consider it to have a strong grade of recommendation (Table 2).
Preoperative fasting and carbohydrate treatmentThe European Society of Anaesthesiology and the American Society of Anaesthesiologists recommend that clear liquids be taken up to two hours before general anaesthesia and a light solid meal up to six hours before.25 We include this recommendation in our REPOC (Table 2). Oral carbohydrate loading (POC) has been proposed as a method for glycaemic control in patients undergoing spinal surgery. However, studies have failed to demonstrate any advantage.26 The currently available evidence is insufficient to make any recommendations for lumbar spinal fusion.
Control of obesityExcess adipose tissue is associated with a chronic low-grade inflammatory state, which favours disc damage and the development of chronic lumbar spinal pain.27 Scientific evidence has shown an increase in complications in obese patients, such as infections and thrombosis, after spinal surgery.28 Patients with a BMI>30 should, as with smoking, be explained the added risks of the intervention. However, the evidence is currently insufficient to make a strong recommendation on the need for weight loss before lumbar fusion surgery, except for cases with a body mass index (BMI)>40 (Tables 2 and 3).
Pre-anaesthetic medicationAs part of the multimodal opioid-sparing analgesia strategy, paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), and gabapentinoids can be used preoperatively.15 Dosage should ideally be adjusted according to the patient's age, kidney function, and comorbidities, and the characteristics of the centre (Table 2).
Anaemia managementIn centres with REPOC protocols performing spinal surgery procedures, preoperative detection of anaemia has been associated with a decrease in transfusions, readmissions, critical care admissions, mean LOS, and costs.29 We believe that patients with pre-operative haemoglobin levels below 11g/dL should not undergo surgery, although the specific value should be agreed for each centre. Although the quality of the scientific evidence is low,2,19 we strongly recommend the assessment and correction of possible preoperative anaemia prior to lumbar fusion surgery.
Intraoperative recommendationsThe main objective of this phase is to reduce the surgical stress response and to provide more tailored and personalised patient care.
Antimicrobial prophylaxis and skin preparationAlthough different clinical trials have shown that the use of prophylactic antibiotics decreases the rate of postoperative infection in spinal surgery,1,2,12,19 there is no universally accepted guideline. Using an iodine or chlorhexidine preparation provides adequate intraoperative skin preparation and reduces the risk of surgical site infection (SSI).30 The high quality of the scientific evidence allows a strong recommendation for the administration of a broad-spectrum antibiotic covering Staphylococcus aureus, with the possibility of repeat doses during longer surgeries, and intraoperative skin preparation using alcohol-based iodine or chlorhexidine solution (Table 2). Each centre will follow the recommendations of its infectious and preventive medicine unit.
Standard anaesthetic protocolThere are a wide variety of anaesthetic protocols in lumbar fusion surgery due to the wide range of available drugs and modes of administration. A large observational study found no difference between general and non-general anaesthetics in terms of readmission rates, complications, and mean LOS.31 With moderate evidence we strongly recommend the use of modern multimodal anaesthesia, including the use of neuromuscular blocking agents and neuraxial techniques (Table 2).
Prevention of intraoperative hypothermiaIntraoperative hypothermia has been associated with increased blood loss, cardiac complications, shivering, SSI, and prolonged mean LOS.2,32 The high quality of scientific evidence leads us to strongly recommend the maintenance of normothermia during and after surgery.
Surgical techniquesNo single technique alone has been shown to have superior beneficial effects over another. The use of minimally invasive approaches is increasingly common in spinal surgery,33 and some authors claim that without minimally invasive surgery the REPOC paradigm loses its relevance.17 Due to the lack of unequivocal data, the surgical techniques to be used must be decided on a case-by-case basis.
Local and regional anaesthetic techniquesLocal and regional anaesthetics are an attractive multimodal approach that may reduce opioid consumption and improve analgesia efficacy. With a high quality of scientific evidence, the use of intrathecal morphine, epidural analgesia, or wound infiltration with long-acting local anaesthetics is recommended to improve postoperative pain management (Table 2).
Perioperative fluid managementSeveral meta-analyses and quantitative reviews have reported improved perioperative outcomes when fluids were managed,9,13,19 which is a common element in REPOC protocols. Although the quality of scientific evidence is moderate, we recommend that intravenous fluids be maintained at near euvolaemic status (Tables 2 and 3).
Early postoperative oral nutritionReturning to normal food intake as soon as possible is considered an essential component of REPOC.1,2,4,11–14 Nevertheless, the direct association of early postoperative feeding with recovery after spinal surgery has not been investigated. Therefore, although the scientific evidence is low, encouragement of an early return to a normal diet is recommended with a strong grade of recommendation.
Urinary drainageProlonged urinary drainage after surgery is associated with urinary tract infections, SSI, and urinary retention. These complications can be reduced with limited catheterisation.2,6,7,12 With moderate quality of evidence, the routine use of urinary catheters for short segment lumbar spine fusions is not recommended, however, if used, they should be removed within hours following surgery with close monitoring (Table 2).
Wound closureThe incidence of SSI is higher in spinal surgery, particularly spinal fusion, than in other types of orthopaedic surgery.19,34,35 Successful wound closure plays an important role in the outcome of the intervention.35,36 Although there are several methods of wound closure, there is no scientific evidence to decide the optimal technique for wound closure in spinal surgery.37 Due to the low quality of the evidence, we cannot make any recommendations (Tables 2 and 3).
Use of haemostaticsSignificant blood loss in spinal surgery has been associated with increased complications and costs.38 The current literature, in line with the REPOC philosophy, supports the combination of techniques and the multimodal approach to minimise blood loss during surgery.38 However, there is strong evidence for the use of tranexamic acid (TXA) as an effective and commonly used haemostatic agent to reduce blood loss, operating theatre time and mean LOS in lumbar spine surgery, although without significant differences in terms of transfusion rate, hepatorenal function, thrombotic risk, stenosis, or patient instability.38–42 With a high quality of scientific evidence, we recommend (strong grade of recommendation) the use of TXA in lumbar fusion surgery.
Postoperative recommendationsThe main objective of this phase is to incorporate goal-directed care and follow-up after surgery to optimise outcomes.
Postoperative analgesiaMultiple studies have demonstrated the efficacy of multimodal perioperative analgesia in relieving postoperative pain and improving final outcomes.7,13,43 Paracetamol and NSAIDs, including selective COX-2 inhibitors, have been shown to be effective in reducing pain and should be part of this analgesia strategy unless there are patient-specific contraindications.7,13 Although the evidence is moderate, the routine use of multimodal analgesic regimens to improve pain control and reduce opioid consumption is recommended with a strong grade of recommendation. The specifics will depend on each centre's availability.
Postoperative nausea and vomiting (PONV)PONV causes dehydration, delayed return to normal intake, increased intravenous fluid administration, prolonged mean LOS, and increased hospital costs.2,7,9 Preoperative assessment of risk factors for PONV is important in the implementation of REPOC protocols. PONV risk assessment and routine use of multimodal prophylaxis are recommended (Tables 2 and 3).
Postoperative drain managementPostoperative drainage is common in lumbar surgery, although data on its usefulness are of low quality.44 In the case of short segment arthrodesis, the use of drains was associated with several complications, such as delayed ambulation and increased pain.45 Routine wound drainage is not recommended for short-segment lumbar fusion surgery (Table 2).
Thromboembolism prophylaxisGiven the relatively low cost, low complication rates and documented efficacy, mechanical prophylaxis should be considered for patients undergoing spinal surgery, although the use of chemoprophylaxis is more controversial. The latter would be more appropriate for high-risk patients, such as those of advanced age, with neurological deficits, and a history of venous thromboembolism.2,19 With a moderate quality of scientific evidence, early ambulation and the use of mechanical prophylaxis is recommended in all patients after spinal surgery (strong grade of recommendation).
Early mobilisation and in-hospital physiotherapyMany cohort studies relate early mobilisation with reduced morbidity and mean LOS.19,46 Early physiotherapy intervention can increase postoperative mobilisation and prevent the negative effects of prolonged rest; however, the need for physiotherapy has not yet been conclusively demonstrated. Early mobilisation of the patient is recommended (with a strong grade of recommendation) and return to normal activity (Table 2).
Continuous improvement and auditsDespite its proven advantages, there are still shortcomings in the implementation of the REPOC paradigm. For example, audits of the implementation of these protocols are rare and prospective studies have yet to be developed. Nevertheless, evidence-based medicine, such as REPOC, improves personal performance and raises the overall standard of medical care.47 Many healthcare professionals are positive about the implementation of REPOC, but find the process difficult.48 To ensure successful implementation of the REPOC guidelines, monitoring, process feedback, and the implementation of outcome measurement tools are essential in an ongoing process of improvement.2–4,6,13,18 Our concept of REPOC therefore is that it is a living tool of continuous evaluation and a commitment to periodic review. This period could be annual or biannual, depending on the characteristics of each centre.
The future of REPOC in spinal surgeryThe focus of the REPOC philosophy is the patient's experience, based on scientific evidence, teamwork, data collection and analysis, and ongoing review of the process to improve the protocol at all stages.1,3,9,12 For REPOC programmes to be effective, compliance and follow-up by all parties involved, including patient, surgeon, and other care providers to that patient, is required.12,17 Therefore, the presence of a dedicated team and a learning curve are essential.4,12
The most common barriers to the implementation of REPOC are resistance to change, lack of time and staff, deficiencies in communication and training of the professionals involved in the process, lack of accurate follow-ups, and initial physician apprehension to discharge patients earlier, as well as lack of leadership, coordination, and collaboration.4,10–14,17,19,21 Moreover, not all patients and procedures are suitable for a REPOC programme, and not all hospitals are able to offer it.17,21 However, given that degenerative lumbar spine conditions are predicted to be a growing healthcare burden in Western countries,17,29 optimising costs and outcomes through paradigms such as REPOC is almost a matter of necessity.
There are still shortcomings to be addressed. The paucity of literature regarding the evidence for REPOC methodology related to lumbar fusion surgery is a limiting factor to its development and validation. Current evidence is restricted to retrospective studies, non-randomised data, and cohort studies that lack formal control groups.16 In the near future, more rigorous RCTs with longer follow-up periods will provide additional robust evidence and improve recovery programmes for specific patient populations.3,16 As the experience and body of data grows, it will streamline interventions and provide spinal surgeons with standardised systems of clinical practice that will reduce all-cause morbidity and mortality, and reduce medical costs.3,17,19 Current trends herald the development of smarter, more personalised and patient-centred medicine, referred to as “healthcare 4.0”.49 The REPOC approach described here is in line with this new way of working in healthcare, and will mean greater patient empowerment and involvement.
Another advantage of the REPOC protocols is that they are modular. Even if a given centre does not manage to implement all the recommendations listed in this consensus document (Table 2), nor complete all the items in the checklist (Table 3), the different items can be implemented independently. Future studies can analyse and verify the efficiency, efficacy, and cost-effectiveness of each recommendation according to patient type, type of surgery, and particular pathology. Thus, further optimisation and better adjustment of the REPOC protocols to the specific circumstances of each centre, each type of intervention, and each patient can be achieved.
ConclusionsSpinal surgery is known for its difficult and uncomfortable recovery process. Most of the reviewed studies reported that the implementation of REPOC protocols in spinal surgery was feasible and associated with shorter mean LOS, accelerated functional recovery, decreased costs, and lower opioid consumption, without increasing complication or readmission rates.4–6,9,11,12,14,16,18 Therefore, using the REPOC approach in patients undergoing spinal surgery, including lumbar arthrodesis, is safe and effective. However, successful implementation of these programmes depends on the integration of several key elements, such as clear communication between all parties, education of patients and caregivers, and a well-structured and organised clinical care sequence. Results have been promising to date, but further studies are needed to justify the expansion of REPOC in the field of spinal surgery.
Level of evidenceLevel of evidence v.
FundingThis article was drafted with the help of Johnson & Johnson Spain.
Conflict of interestsLAG has worked as a consultant for DePuy Synthes, Zimmer Biomet, NuVasive and Spineart. The other authors have no conflict of interests to declare.
We would like to thank Johnson & Johnson for acting as facilitator of the working team (Javier Quintana, Pablo Torres, and Jorge Navarrete) and a Novaquality Consulting S.L. for their help in drafting the document (José Luis Ramírez).