To analyse the clinical and radiologic results, the survival and complications obtained in 70 year or older patients who underwent cementless total knee arthroplasty (TKA).
Material and methodAn observational study of patients operated between January 2014 and December 2016 was carried out according to the Natural Knee model (Zimmer®, USA). The main variables were the Oxford Knee Score, the visual analogue scale, the presence of radiolucencies, complications, survival and reasons for revision.
ResultsOf 104 TKA, 86 were available for revision. The median age was 76 years. The mean follow-up was 5.4 years (range 3.7–6.9). The Oxford Knee Score punctuation showed a median of 17 presurgical (range 0–40) and 37 post surgical (range 5–48), P<.001. The 87.2% of the patients obtained a clinically significant improvement. The median visual analogue scale punctuation was 8 for presurgical (range 4–10) and 2 for post surgical (range 1–9), P<.001. The 88.3% of the patients obtained a clinically significant decrease. Three months after the surgery, the 55.81% of the TKAs presented radiolucencies around the tibial plateau. At the end of the follow-up, radiolucencies were present in 30.23% of the TKAs. Survival from all causes was 91.86% at 77.2 months and 96.5% due to aseptic loosening.
ConclusionCementless knee prostheses are a valid option in patients aged 70 or older, presenting good clinical, radiological and survival results.
Analizar los resultados clínicos, radiológicos, la supervivencia y las complicaciones obtenidos en pacientes de 70 años o más intervenidos mediante artroplastia total de rodilla (ATR) no cementada.
Material y métodoSe realizó un estudio observacional de pacientes intervenidos entre enero 2014-diciembre 2016 con el modelo Natural Knee (Zimmer®, Estados Unidos). Las variables principales fueron la puntuación de Oxford Knee Score y la de la escala visual analógica, la presencia de radiolucencias, complicaciones, supervivencia y motivo de revisión.
ResultadosDe 104 ATR, 86 estuvieron disponibles para su revisión. La mediana de edad fue de 76 años. El seguimiento medio fue de 5,4 años (rango 3,7–6,9). La puntuación del Oxford Knee Score presentó una mediana de 17 (rango 0–40) prequirúrgica y 37 (rango 5–48) posquirúrgica, p<0,001. El 87,2% de los pacientes obtuvo una mejoría clínicamente significativa. La mediana de la puntuación de la escala visual analógica fue 8 (rango 4–10) prequirúrgica y 2 (rango 1–9) posquirúrgica, p<0,001. El 88,3% de los pacientes obtuvo una disminución clínicamente significativa. Alrededor del platillo tibial, a los 3 meses de la cirugía, el 55,81% de las ATR presentaron radiolucencias, al final del seguimiento las radiolucencias estuvieron presentes en el 30,23% de las ATR. La supervivencia por todas las causas fue del 91,86% a los 77,2 months y del 96,5% por aflojamiento aséptico.
ConclusiónLas prótesis de rodilla no cementadas son una opción válida en pacientes de 70 o más años, presentando buenos resultados clínicos, radiológicos y de supervivencia.
Total knee arthroplasty (TKA) is one of the most common interventions in orthopaedic surgery. The main surgical indication is degenerative osteoarthritis, which accounts for over 95% of diagnosed cases.1 The aim of TKA is to replace a painful joint with a painless one which functions better. Therefore, given the continuous increase in life expectancy2 and progressive ageing of the Western population, the demand for TKA and the mean age of patients undergoing it continues to rise.3
Since the appearance of the first cementless implants in the 1970s, the choice between cementing or cementless as a technique for TKA fixation has been a controversial issue.4 Today, cemented TKAs continue to be the gold standard, given the good results and high survival they have demonstrated.5 However, interest in cementless has resurfaced in recent years due to the increased rate of aseptic loosening in cemented TKA in patients with high functional demand and in obese patients.2
Initially, cementless implants showed unfavourable results, with a high rate of aseptic loosening, and were therefore discontinued for a long time.6,7 However, these problems were solved with the new designs. A decisive change was the coating of the implants. Hydroxyapatite or trabeculated tantalum coatings promote osseointegration between the implant and the bone, promoting a biological fixation that leads to greater implant stability, greater resistance to shear forces and longer survival.4,8 The new generation of cementless TKAs is showing excellent results, with a significant increase in longevity.9 For this reason, some authors are already recommending them for young patients.10
The age up to which non-cementation should be recommended is also a matter of debate. On the one hand, some authors advise against cementing in older patients, citing reduced bone remodelling due to ageing as a possible cause of implant failure.11,12 In contrast, other authors advocate non-cementation to achieve a more stable implant fixation11,13 and thus avoid the need for future prosthetic replacement surgery in older patients.
The aim of this study is to analyse the clinical and radiological results, complications and survival obtained in patients aged 70 years or older with cementless TKAs in our centre.
Material and methodDesignAn observational study was conducted to analyse the clinical and radiological outcomes and survival of consecutive cementless knee replacements implanted in our department. The study was approved by the Ethics Committee of our institution (reference 103/20). Informed consent was not required as it was an evaluation of routine clinical practice. All primary TKAs implanted in our centre with a minimum clinical and radiological follow-up of 2 years in which the Natural Knee prosthetic model (Zimmer®, USA) with porous titanium coating was used were included. Patients with a diagnosis of inflammatory osteoarthritis (rheumatoid arthritis, psoriatic arthritis, etc.) and patients whose questionnaires were not correctly completed were excluded.
SampleA minimum sample size of 58 patients was calculated to demonstrate a clinically meaningful outcome for postoperative change of 5 points or more on the Oxford Knee Score (OKS). This figure was extracted from the literature.14 We performed the calculation with an alpha error of 5% and a power of 80%, assuming losses of 15%.
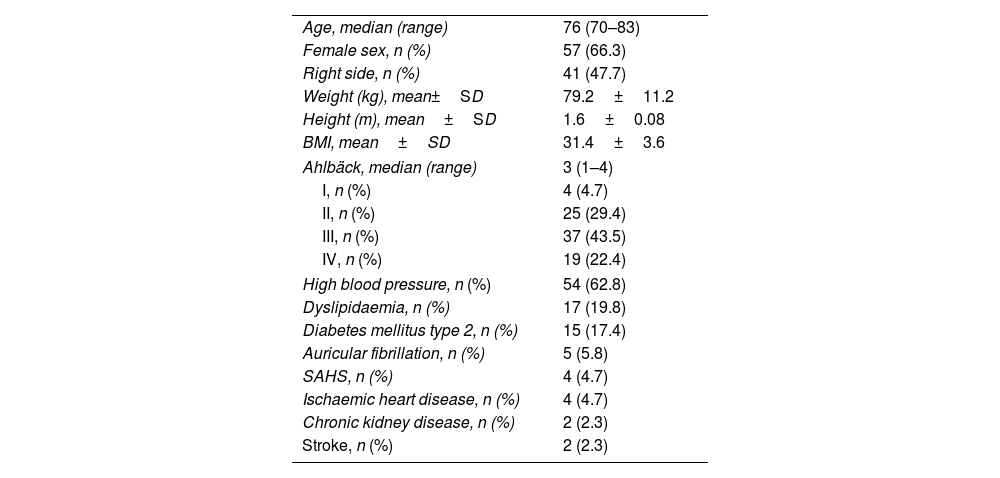
Between January 2014 and December 2016, 104 knees were operated on in 99 patients. Two patients were excluded due to rheumatoid arthritis, one due to psoriatic arthritis, six due to loss to follow-up and nine patients died. None of the patients died of surgery-related causes. Therefore, 86 knees of 81 patients had complete radiographic and clinical evaluations. The average length of follow-up of the included patients was 5.4 years (range: 3.7–6.9). The baseline characteristics of the included patients are summarised in Table 1.
Baseline patient characteristics.
| Age, median (range) | 76 (70–83) |
| Female sex, n (%) | 57 (66.3) |
| Right side, n (%) | 41 (47.7) |
| Weight (kg), mean±SD | 79.2±11.2 |
| Height (m), mean±SD | 1.6±0.08 |
| BMI, mean±SD | 31.4±3.6 |
| Ahlbäck, median (range) | 3 (1–4) |
| I, n (%) | 4 (4.7) |
| II, n (%) | 25 (29.4) |
| III, n (%) | 37 (43.5) |
| IV, n (%) | 19 (22.4) |
| High blood pressure, n (%) | 54 (62.8) |
| Dyslipidaemia, n (%) | 17 (19.8) |
| Diabetes mellitus type 2, n (%) | 15 (17.4) |
| Auricular fibrillation, n (%) | 5 (5.8) |
| SAHS, n (%) | 4 (4.7) |
| Ischaemic heart disease, n (%) | 4 (4.7) |
| Chronic kidney disease, n (%) | 2 (2.3) |
| Stroke, n (%) | 2 (2.3) |
BMI, body mass index; SAHS, sleep apnoea and hypopnoea syndrome; SD, standard deviation.
Patients were operated on by a team of surgeons experienced in knee arthroplasty. An ischaemia sleeve was used in all cases. The approach was medial parapatellar. Guidance for tibial cuts was extramedullary in 76.7% of patients. For femoral sections the guidance was intramedullary. In the sagittal axis, the rotation of the femoral component was 3° or 5° to external depending on the anatomy of the case, while the tibial component was aligned with the junction between the medial third and the outer 2 thirds of the patellar tendon. Test blocks were used to verify the balance of the spaces, with appropriate soft tissue releases performed in case of imbalance. Alignment was verified using trial components. The final components were fixed using the pressfit technique. No patella was prosthesised. A vacuum drain was placed after the procedure and removed after 48h. Ischaemia was removed after 48h. Ischaemia was removed after wound closure and placement of a compression dressing. Antibiotic prophylaxis was performed with a single dose of 2g cefazolin and 240mg gentamicin intravenously prior to induction of anaesthesia and then continued with 1g cefazolin every 8h for 24h. In case of beta-lactam allergy, cephalosporin was replaced by clindamycin. Thromboprophylaxis was carried out with low molecular weight heparin for one month. Weight-bearing, if tolerated, was allowed with the aid of a walker the day after surgery. During the admission period patients received assisted rehabilitation which started the day after surgery and continued after discharge in rehabilitation centres.
AssessmentsClinical and radiological assessments were performed by the surgeon preoperatively and postoperatively at 15 days, 1, 3, 6, 12, 24 months and then annually.
Joint range was recorded at each visit. Functional assessment was performed using the OKS, validated in Spanish,15 where 0 points corresponds to the worst result and 48 to the best. Pain was assessed using the visual analogue scale. For each questionnaire, a clinically significant result was considered when the change was 5 or more points on the OKS16 and 3 or more points on the visual analogue scale.17
The radiological evaluation assessed the presence of radiolucencies (RL) at the tibial plateau, as well as the presence of signs of loosening such as implant displacement or subsidence. RLs were defined as radiolucent intervals between the implant and adjacent bone ≥1mm in more than 50% of a zone. The zones were defined using the Knee Society evaluation and scoring system.18 Progression of LR, defined as a progressive increase in radiolucent areas, was also observed.
For the analysis of the results, only the pre-surgical results and the last follow-up were considered. Implant survival at the end of follow-up was also recorded.
Statistical analysisStatistical analysis was performed using SPSS version 25.0.0. In the descriptive analysis of the results, the mean (standard deviation) was used for normal quantitative variables, the median (range) for non-normal variables, and absolute and relative frequencies were used for nominal variables. To analyse the significance of clinical outcomes before and after surgery, the normality of the variables was studied using the Kolmogorov–Smirnov test and the Student's t-test or Wilcoxon sign test was used. For analysis of the clinical significance of the results, the included patients were divided into those whose result was clinically significant and those whose result was not, differences between groups were compared using the Mann–Whitney U or the χ2 test. Results with a P-value <.05 were considered statistically significant. Hedges’ g-test for related samples was used to calculate effect size.
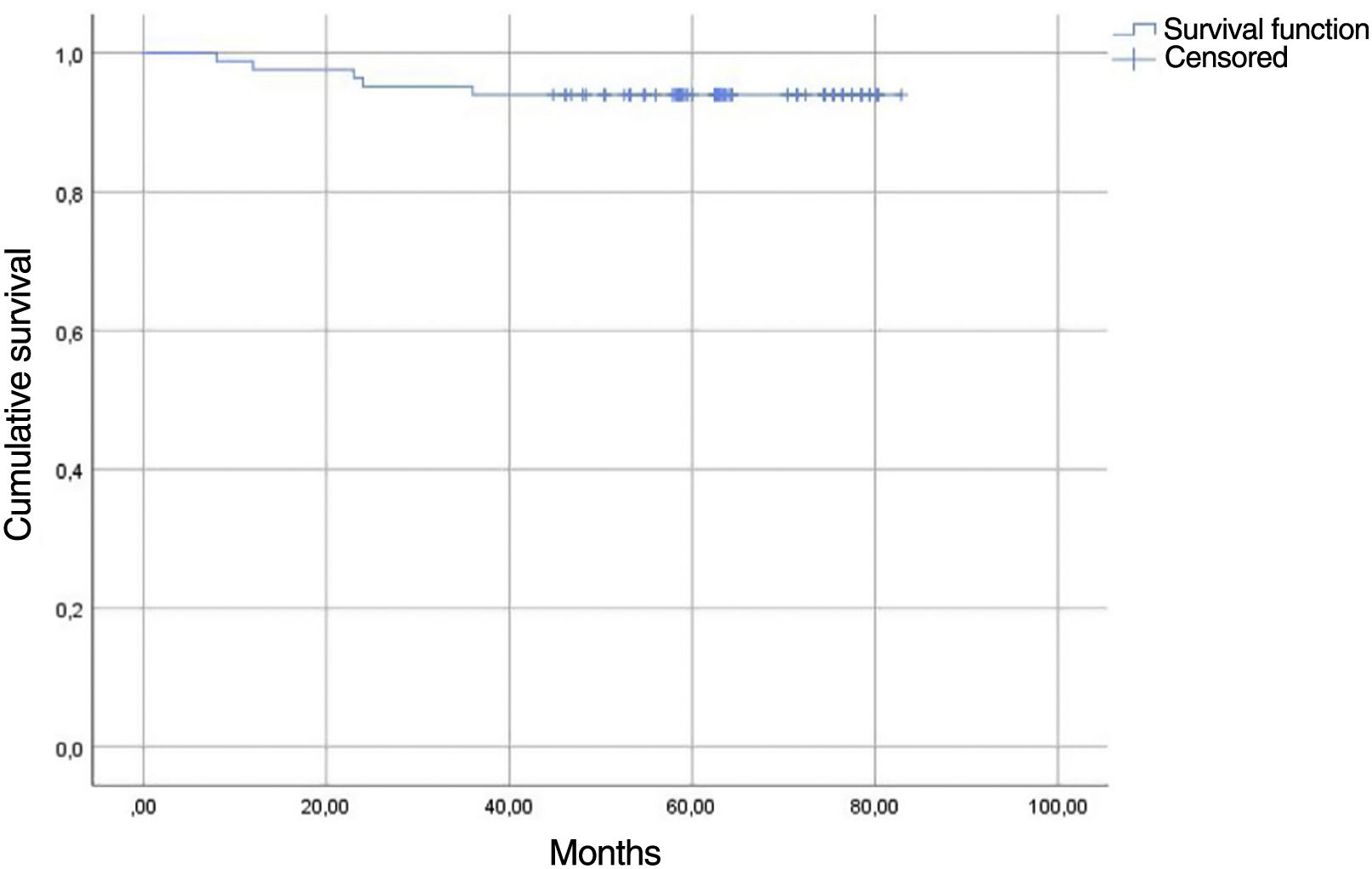
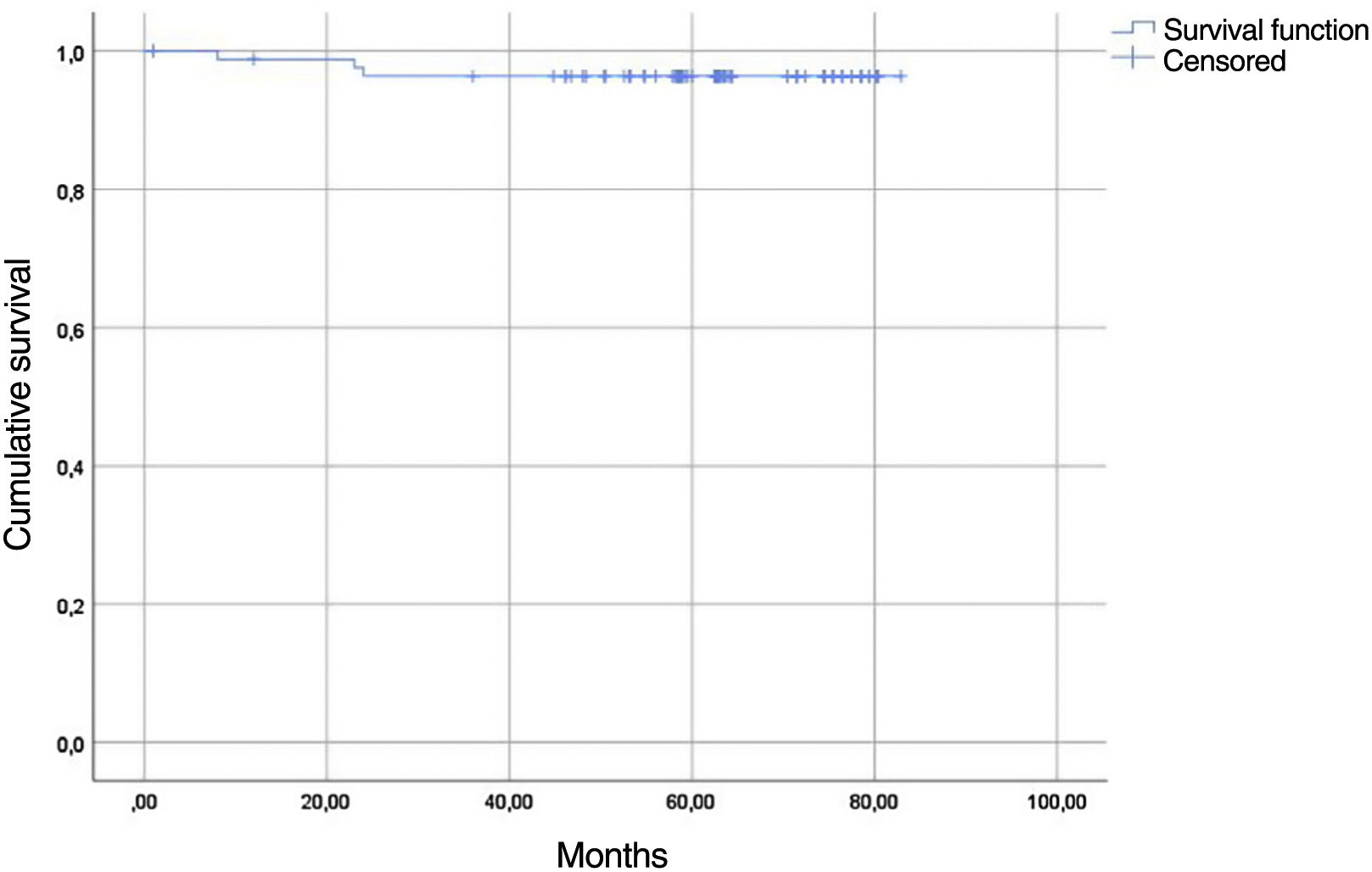
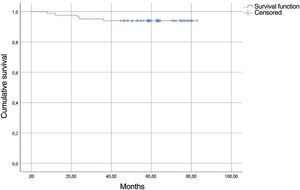
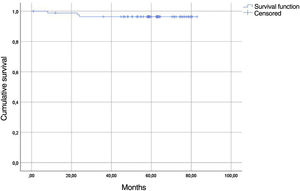
Implant survival was plotted using the Kaplan–Meier curve with endpoint at implant survival for revision for aseptic loosening and for revision for any cause.
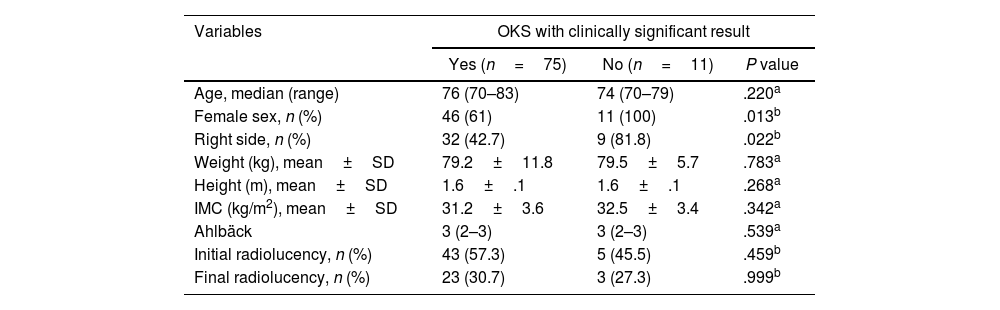
ResultsClinical outcomesThe OKS score had a median of 17 (range: 0–40) preoperatively and 37 (range: 5–48) postoperatively, P<.001. 87.2% (75/86) of patients had a clinically significant improvement in OKS with a large effect size (g-Hedges=−1.4, P=.000). 19.3% of women had a clinically non-significant result, while all men had clinically significant results (Table 2).
Clinically significant results of the Oxford Knee Score.
| Variables | OKS with clinically significant result | ||
|---|---|---|---|
| Yes (n=75) | No (n=11) | P value | |
| Age, median (range) | 76 (70–83) | 74 (70–79) | .220a |
| Female sex, n (%) | 46 (61) | 11 (100) | .013b |
| Right side, n (%) | 32 (42.7) | 9 (81.8) | .022b |
| Weight (kg), mean±SD | 79.2±11.8 | 79.5±5.7 | .783a |
| Height (m), mean±SD | 1.6±.1 | 1.6±.1 | .268a |
| IMC (kg/m2), mean±SD | 31.2±3.6 | 32.5±3.4 | .342a |
| Ahlbäck | 3 (2–3) | 3 (2–3) | .539a |
| Initial radiolucency, n (%) | 43 (57.3) | 5 (45.5) | .459b |
| Final radiolucency, n (%) | 23 (30.7) | 3 (27.3) | .999b |
BMI, body mass index; OKS, Oxford knee score; SD, standard deviation.
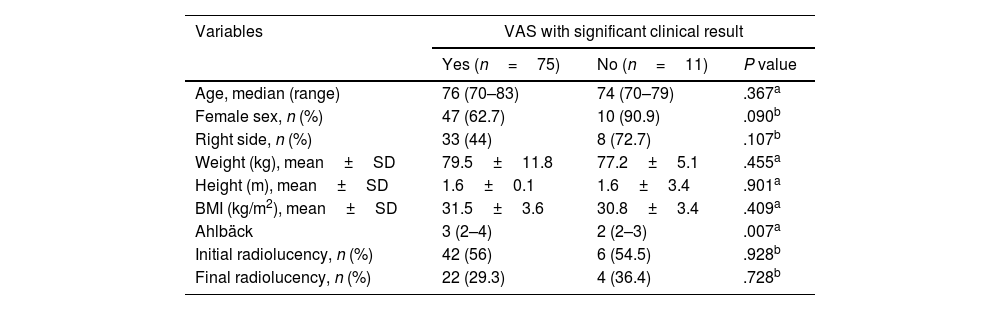
In terms of pain, the median visual analogue scale score was 8 (range: 4–10) pre-surgery and 2 (range: 1–9) post-surgery, P<.001. 88.3% (76/86) of patients had a clinically significant decrease in pain (Table 3) with a large effect size (g-Hedges=2.3, P=.000).
Significant clinical results of the visual analogue scale.
| Variables | VAS with significant clinical result | ||
|---|---|---|---|
| Yes (n=75) | No (n=11) | P value | |
| Age, median (range) | 76 (70–83) | 74 (70–79) | .367a |
| Female sex, n (%) | 47 (62.7) | 10 (90.9) | .090b |
| Right side, n (%) | 33 (44) | 8 (72.7) | .107b |
| Weight (kg), mean±SD | 79.5±11.8 | 77.2±5.1 | .455a |
| Height (m), mean±SD | 1.6±0.1 | 1.6±3.4 | .901a |
| BMI (kg/m2), mean±SD | 31.5±3.6 | 30.8±3.4 | .409a |
| Ahlbäck | 3 (2–4) | 2 (2–3) | .007a |
| Initial radiolucency, n (%) | 42 (56) | 6 (54.5) | .928b |
| Final radiolucency, n (%) | 22 (29.3) | 4 (36.4) | .728b |
BMI, body mass index; SD, standard deviation; VAS, visual analogue scale.
Mean range of motion improved from 107.2° (range: 90–130) [95% CI: 104–106] preoperatively to 110.5° (range: 90–130) [95% CI: 107–113] at the end of follow-up, P=.001.
Radiographic results72.9% of patients had an Ahlbäck grade ii/iii radiographic deformity, 4.7% grade i and 22.4% grade iv.
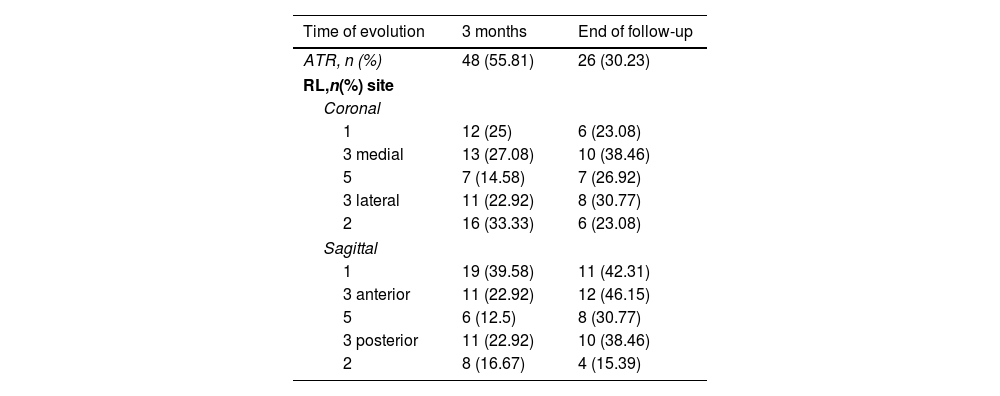
Around the tibial plateau, at 3 months after surgery, 55.81% of the TKAs had LR. In the coronal plane, LR were present in 38.37% of the TKAs, with zones 2 and 3M being the most commonly affected. In the sagittal plane, 41.86% of arthroplasties showed LR, with zones 1 and 3 (anterior and posterior) being the most affected (Table 4).
Frequencies, n (%) of the radiolucencies by region at the beginning and termination of follow-up.
| Time of evolution | 3 months | End of follow-up |
|---|---|---|
| ATR, n (%) | 48 (55.81) | 26 (30.23) |
| RL,n(%) site | ||
| Coronal | ||
| 1 | 12 (25) | 6 (23.08) |
| 3 medial | 13 (27.08) | 10 (38.46) |
| 5 | 7 (14.58) | 7 (26.92) |
| 3 lateral | 11 (22.92) | 8 (30.77) |
| 2 | 16 (33.33) | 6 (23.08) |
| Sagittal | ||
| 1 | 19 (39.58) | 11 (42.31) |
| 3 anterior | 11 (22.92) | 12 (46.15) |
| 5 | 6 (12.5) | 8 (30.77) |
| 3 posterior | 11 (22.92) | 10 (38.46) |
| 2 | 8 (16.67) | 4 (15.39) |
TKA, total knee arthroplasty; RL, radiolucencies.
% of total for each plane and follow-up time.
At the end of follow-up, we observed a decrease in the frequency of LRs, present in 30.23% of the TKAs, as well as a relative increase in the frequency of LRs around the prosthetic stem. In the coronal plane we observed LR in 19.77% of the arthroplasties, and these were concentrated in zones 3M, 5 and 3L. In the sagittal plane, 27.91% of the TKAs showed lucid lines, and these were concentrated in zones 1 and 3 (anterior). The recorded LRs are listed in Table 4. LR progression occurred in patients with aseptic loosening and in two patients who remain asymptomatic.
Complications and survivalRegarding complications, one patient had a sensory neuropathy of the external popliteal sciatic nerve after surgery that remains at the present time. Another patient had a popliteal artery injury, which required in situ repair without subsequent ischaemia. Immediately postoperatively, another patient had a transient ischaemic event that resolved without sequelae.
Three patients had clinical signs of superficial infection with negative culture. One of these patients evidenced cellulitis in the calf area which required the use of oral antibiotics for 2 weeks. The other two patients had erythema at the surgical wound site requiring oral antibiotic treatment for 2 weeks. None of these patients had prosthetic infection.
Finally, two patients presented acute prosthetic infection during the first month of follow-up. Both were treated with DAIR (debridement, antibiotics and implantretention) and progressed favourably.
All-cause survival was 91.86% [95% CI: 91.2–92.4] at 77.2 months [95% CI: 73.2–81.29] (Fig. 1) and 96.5% [95% CI: 96.1–96.9] for aseptic loosening. Of the seven revisions, the cause was aseptic loosening in three patients, instability in one patient, patella fitting in one patient and the remaining two patients had acute prosthetic infection as previously mentioned. Aseptic revisions were performed between 8 months and 2 years follow-up, survival of 79.1 months [95% CI: 75.8–82.3] (Fig. 2). These patients had RL lines at the tibial plateau that progressed. Patellar fitting occurred in one patient with clinical anterior pain.
There were no further complications in any of the patients.
DiscussionCementless fixation in TKA was developed with the aim of increasing implant survival, preserving bone stock and reducing cement-related implant failures. Despite the high failure rates of older implants, the emergence of new biomaterials and improved designs of cementless TKAs led to better initial fixation and faster osseointegration, with significantly improved outcomes.11
However, the use of uncemented TKAs has been questionable in older patients due to doubts about the fixation capacity of osteoporotic bone and competence to withstand force transmission.11,19 Despite this, the available literature is sparse, so we aimed to provide evidence on this topic in this study.
Our results demonstrate that the use of cementless TKAs in patients aged 70 years and older have good functional and radiological results, a low complication rate and adequate survival. The results were clinically significant in 87.2% of patients according to the OKS. However, when reviewing the medical literature, publications that present their results using the term minimal clinically important difference are infrequent. We believe that using this concept in the analysis of clinical outcomes is essential, as obtaining statistically significant differences between pre- and post-surgical scores on a functional scale is not equivalent to a clinically relevant improvement for the patient.20 Clement et al.16 reported that the results that correspond to very good or excellent patient satisfaction are those whose difference is around 17 points. The median difference before and after surgery in our study is 20 points, which shows that patients aged 70 years and older who underwent cementless TKA are in adequate ranges of satisfaction. The only variable associated with unsatisfactory results was sex. Several authors report worse results in women after TKA. Parsley et al.21 studied 698 patients, 61% of whom were women. They observed that women had lower scores on the scale used. Similar results were found by Mehta et al.22 in 494 patients (65.3% women), observing that women seem to have worse outcomes than men possibly due to a worse preoperative profile.
We have also observed a clinically significant improvement in pain in 88.3% of patients. Danoff et al.17 reported that the results that correspond to some or a lot of satisfaction in pain improvement are those whose difference is around 22.6mm. In our study we have been even stricter in this difference, taking it to 3 points, which we consider to be equivalent to, or even greater than, the displacement in millimetres.
With regard to radiological analysis, it should be specified that the appearance of RL, in the absence of implant migration or circumferential radiolucent lines around the implant, is not considered a sign of loosening.2,23 They occur more frequently in cementless TKAs, but their presence does not lead to worse clinical outcomes.23 The percentage of occurrence is highly variable between studies. Mutsuzaki et al.24 recently performed an analysis, concluding that the occurrence of RL in the tibial plateau is maximal during the first year and decreases thereafter, obtaining rates of 64% at the time of study completion at 3 years of follow-up, higher than the maximum present in our study (30.23%). These authors believe that the reduction in LR over time may be due to continued bone growth between the trabecular metallic components. In our study, we observed a significant decrease in the LR in the coronal plane (−48.48%) and a slightly smaller decrease in the sagittal plane at the end of follow-up (−33.33%).
Following this line of research, Hasan et al.25 contrasted the migration of uncemented 3D-printed TKA components with a similar design (with cruciate retention) cemented in 72 patients. They found greater migration of the cementless TKA components, especially at the expense of tibial plate subsidence, in the first 3 months, with subsequent stabilisation. However, Nivbrant et al.26 compared the migration of uncemented versus cemented post-stabilised TKAs, obtaining a late and continued tibial plateau subsidence in uncemented TKAs, recommending cemented tibial fixation in post-stabilised implants.
When comparing the results with those obtained in younger patients, they are also similar. Dixon et al.13 compared 135 patients with a mean age of 79 years (range: 75–83 years) with 424 patients with a mean age of 66 years (range: 33–74 years) who received a cementless hydroxyapatite-coated TKA. At 5-year follow-up, both groups had similar clinical outcomes. There was a trend towards more infections and revision surgeries in the younger group and a propensity towards more minor medical complications in the older group, but these did not reach statistical significance. In our study we do not consider the observed complications to be related to the non-cementation of the implant.
Using an uncemented TKA model with porous titanium coating, we obtained a survival rate for aseptic loosening of 96.5% and 91.8% for all causes, with a mean follow-up of 5.4 years. Our results are comparable to those previously published. Bouras et al.4 evaluated 136 cementless TKAs in patients with a mean age of 80 years and a mean follow-up of 13.2 years. Survival due to aseptic loosening was 93.6% and 90.4% in the analysis of all-cause revisions. Ferrer-Santacreu et al.7 analysed the results of 96 cementless TKAs in patients with a mean age of 79 years and a mean follow-up of 14.5 years. Survival due to aseptic loosening was 93.75% and 88.54% in the analysis of all-cause revisions. Newman et al.11 analysed 142 cementless implants with a mean follow-up of 4 years in patients older than 75 years. Survival due to aseptic loosening was 99.3% and 98.6% in the analysis of all-cause revisions. Zhou et al.,5 in a recent meta-analysis found no difference in survival and functional outcomes between cemented and cementless TKAs.
There are limitations to this study. Firstly, this is a retrospective study, however, data loss was minimal due to prospective data collection by the surgeons. Another limitation is the lack of a matched cohort control group. In addition, the clinical assessments were performed by the surgeons and not by independent observers as recommended, however, this is inherent to the retrospective nature of the study. Although the mean follow-up of the study is 5 years (range: 3.7–6.9), allowing us to assess short- and medium-term failures, the follow-up time is insufficient to assess long-term outcomes. However, given the scarce medical literature available on cementless TKAs in patients over 70 years of age, this study contributes to reinforce the growing evidence of the good results of these implants.
ConclusionCementless knee replacements are a valid option in patients aged 70 years and older, with good clinical, radiological and survival outcomes.
Level of evidenceLevel of evidence IV.
Conflict of interestThis research has not received specific support from public sector agencies, commercial sector or non-profit organisations.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.