Persistent or recurrent glenohumeral instability after a previous operative stabilization can be a complex problem.
Our aim is to establish the incidence of recurrence and its revision surgery, and to analyze the functional results of the revision instability surgery, as well as to determine surgical protocols to perform it.
Materials and methodsA retrospective analysis was conducted on 16 patients with recurrent instability out of 164 patients operated on between 1999 and 2011. The mean follow-up was 57 months and the mean age was 29 years. To evaluate functional outcome we employed Constant, Rowe, UCLA scores and the visual analog scale.
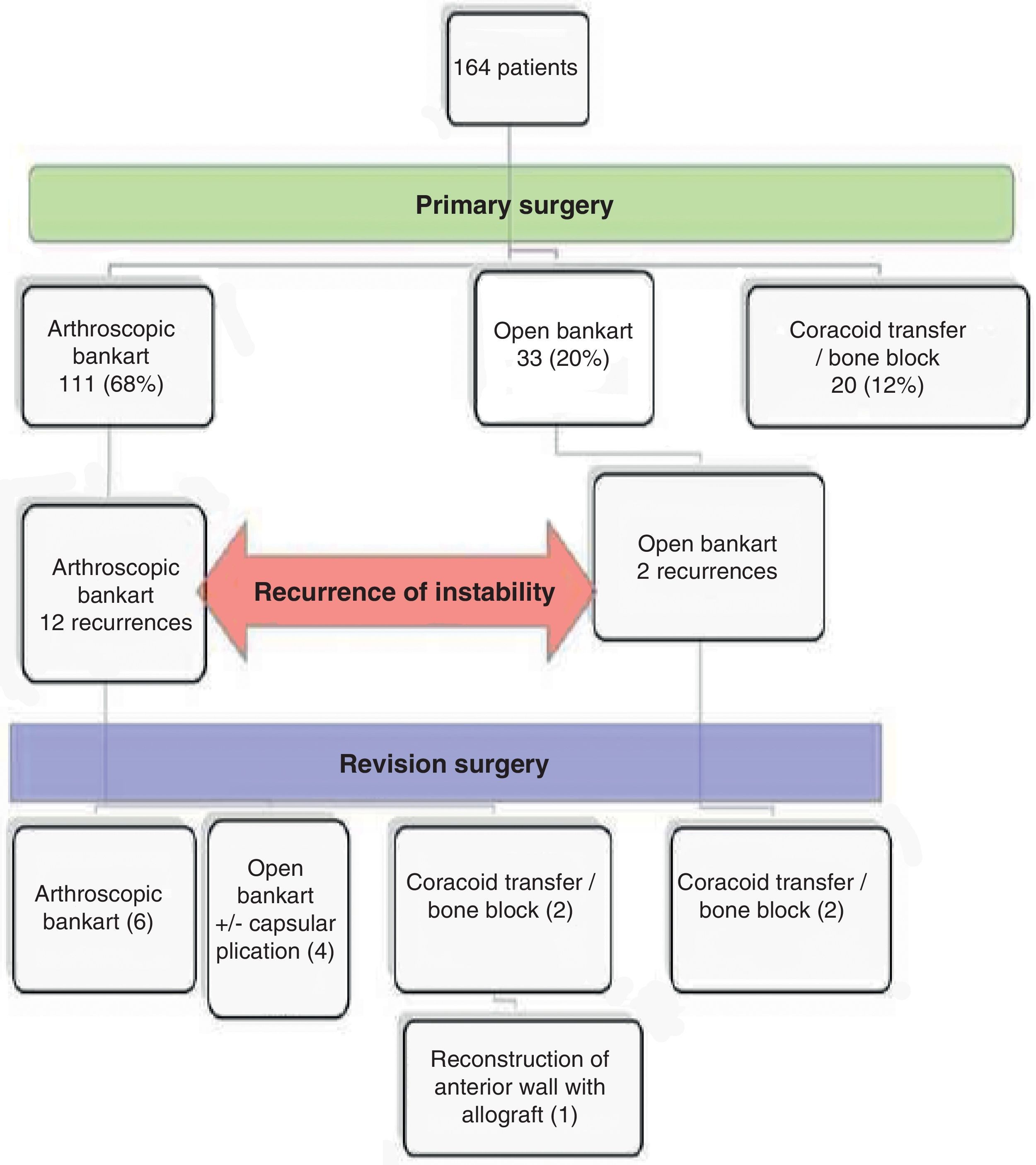
ResultsOf the 12 patients who failed the initial arthroscopic surgery, 6 patients underwent an arthroscopic antero-inferior labrum repair technique, 4 using open labrum repair techniques, and 2 coracoid transfer. The two cases of open surgery with recurrences underwent surgery for coracoid transfer. Results of the Constant score were excellent or good in 64% of patients.
ConclusionsSurgical revision of instability is a complex surgery essentially for two reasons: the difficulty in recognizing the problem, and the technical demand (greater variety and the increasingly complex techniques).
Aunque las tasa de recidiva tras la cirugía primaria de la inestabilidad no son despreciables son pocos los estudios que encontramos sobre su cirugía de revisión.
Los objetivos de esta serie son establecer la frecuencia de recidiva de la inestabilidad en la misma y de su cirugía de revisión; analizar los resultados funcionales obtenidos y determinar un protocolo quirúrgico de actuación ante la necesidad de realizar una cirugía de revisión.
Material-MétodoAnálisis retrospectivo. 16 pacientes con recidiva de inestabilidad tras cirugía previa en 164 pacientes intervenidos entre 1999–2011. Seguimiento medio de 57 meses y edad promedio 29 años. Evaluación de resultados mediante las escalas Constant, Rowe, UCLA.
ResultadosDe los 12 casos de cirugía artroscópica que recidivaron, en 6 se reparó el labrum mediante artroscopia, en 4 mediante reparación abierta y plicatura capsular y en 2 mediante trasferencia de coracoides. En los dos casos de cirugía abierta se realizó una cirugía de trasferencia de coracoides. Las puntuaciones obtenidas en la escala de Constant en el hombro intervenido fueron Excelente/Buena en el 64% de los pacientes.
ConclusionesAunque las técnicas de estabilización primaria abierta y/o artroscópica se han perfeccionado mucho, el porcentaje de recurrencia no resulta nada despreciable. De ahí la importancia de establecer un protocolo quirúrgico de actuación como lo existe para la indicación quirúrgica de una estabilización primaria. Podemos afirmar que los resultados funcionales obtenidos tras la cirugía de revisión resultan satisfactorios para las elevadas demandas funcionales que presentan este tipo de pacientes.
There are different options for the surgical treatment of anterior shoulder (or glenohumeral) instability. In general terms, these procedures can be divided into anatomical and non-anatomical techniques. The goal of anatomical repairs is to reinsert the labrum into its normal position and to restore tension to the ligaments and joint capsule (this is normally described as the Bankart procedure1 or capsular plication). The goal of non-anatomical techniques2 is to stabilize the shoulder by compensating the capsulolabral or bone lesion with a bone block (Bristow–Latarjet technique and Eden–Hybinette technique) or soft tissue block, although the latter is currently falling into disuse (Magnuson–Stack technique, Putti–Platt procedure). The aim is to block excessive movement, thus restoring stability. At present, the technical advances experienced by shoulder arthroscopic surgery enable both anatomical (labrum reinsertion) and non-anatomical procedures, that is, bone blocks (coracoid transfers, auto- or allografts) to be performed.
In connection with the failure of these procedures during primary surgery, in early studies, open labral reinsertion with capsular plication presented lower rates of recurrence than arthroscopic reinsertion. However, the evolution experienced by arthroscopic techniques has equaled both recurrence rates, which are currently around 10%.3
Recurrence rates with bone blocks are highly variable: 20% with the Eden–Hybinette technique,4 15% with the Bristow–Latarjet technique,5 and less than 5% with the Latarjet technique.6 Lafosse and Boyle obtained 100% of positive results by performing this technique through arthroscopy. Nevertheless, the high technical demands represented a drawback.7
It is surprising that, although recurrence rates for these processes are not negligible, very little literature can be found regarding the results obtained after surgical revision of glenohumeral instability.8 The main factors which have been suggested as responsible for these failures are: the presence of trauma following the initial surgical stabilization, diagnostic errors (and, therefore, in patient selection and adaptation of the selected technique) and failures in the performance of the surgical technique.9 Diagnostic errors include a lack of recognition of bone defects10 (in glenoid or anterior portion of the cephalic surface) present in up to 89% of primary surgery failures, lack of recognition of associated joint hypermobility (or hyperlaxitude), presence of poor tissue quality and potential problems with proper postoperative rehabilitation. Technical errors encompass non-anatomical repairs with incorrect positioning of the anchors, the lack of recognition of associated injuries or the application of inadequate tension to the capsule, which may be left too mobile.
Although protocols for the initial surgical treatment of instability are perfectly established,11,12 these actions represent an excessive simplification of the problem in the case of revision surgery, leaving the surgeon with little guidance regarding the technique to perform.
Nevertheless, the results of multiple studies following open or arthroscopic revision surgery of anterior instability are globally favorable,13–15 although relapse rates have been reported which have reached as high as 50% among patients who have undergone several procedures.9,16
The current review of case series aims to establish the incidence of recurrence of instability following primary open or arthroscopic stabilization, to analyze the functional results of revision surgery for instability and to determine the percentage of recurrence after it, as well as to establish a protocol for these patients.
Our working hypothesis focuses on the idea that adapting revision surgery for instability to the anatomopathological and functional status of each patient provides good results and a low rate of recurrence.
Materials and methodsStudy designThis was a retrospective and observational study conducted with patients who had undergone failure of glenohumeral instability surgery.
Inclusion criteria:
- •
Patients who underwent 1 or more revision surgeries for instability, after the failure of the previous procedure. The diagnosis was established by verification through simple radiography with at least 1 episode of anterior dislocation after the first surgery and/or episodes of symptomatic instability: sudden onset of crippling pain during activities involving external rotation and abduction, such as throwing (“dead arm” syndrome) or perception of instability by the patient (apprehension).
- •
Initial surgery by open or arthroscopic approach.
- •
Recurrence of traumatic or atraumatic dislocation.
- •
Open or arthroscopic revision surgery.
Exclusion criteria:
- •
Absence of revision surgery after recurrence of instability.
- •
Lack of previous clinical data or impossibility to conduct evaluation.
- •
Significant comorbidities (hypermobility, epilepsy).
- •
Diagnostic errors (atraumatic, multidirectional instabilities).
We conducted a review of 164 medical records, located through the Archive and Clinical Documentation Department at our hospital, corresponding to patients treated for anterior shoulder instability at our center and followed through outpatient consultation until their discharge, so there was no loss of follow-up. Patients were intervened during the time period between January 1999 and December 2011. Of these cases, 68% (111 patients) underwent arthroscopic reinsertion of the labrum-ligament complex (LLC), with capsular plication being associated in 76% of patients (84 cases) in order to reduce the anteroinferior recess through suture stitches from the same anchors used in the Bankart lesion repair. This technique was the first choice, being used in all those cases with evidence of LLC disinsertion. The association of capsular plication took place in cases in which the labrum was not only disinserted but also deteriorated, thus not offering sufficient intraoperative guarantees for the isolated reintegration of the complex.
In total, 20% (33 cases) underwent a reinsertion of the anteroinferior labrum through open surgery, always associated to anteroinferior capsular recess reduction by plication. Since this was a historic series, the choice of this open technique versus the arthroscopic alternative varied in its criteria. Originally, it was based on the pre- or intraoperative presumption of an impossibility to perform an optimal repair through the arthroscopic technique.
Lastly, 12% (20 cases) underwent open surgery with coracoid transfer. This technique was the main choice for patients who presented a significant glenoid bone defect (over 30% of the glenoid surface).
Out of the total intervened patients, 16 (9.75%) presented recurrent dislocation after the initial procedure. We excluded from the final study (functional outcome assessment) 2 patients who decided not to undergo reoperation. The evaluation of the remaining 14 patients at the end of the follow-up period was performed in outpatient consultation following telephone appointment by an independent examiner not involved in the surgical procedures. A personal interview was conducted, along with a detailed physical examination and application of the appropriate rating scales to establish the functional status.
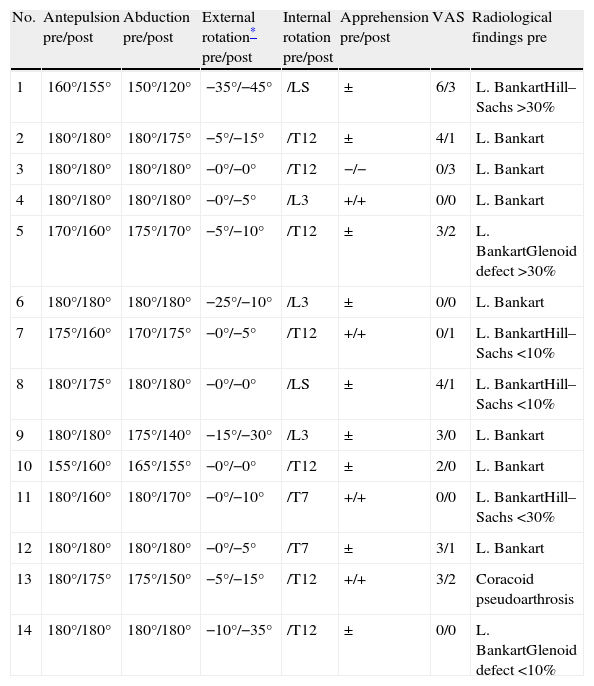
The clinical condition prior to revision surgery of these 14 patients is summarized in Table 1 (range of motion of the shoulder joint, external rotation deficit, presence of apprehension and visual analog scale [VAS]).
Most relevant radiographic findings prior to revision surgery.
| No. | Antepulsion pre/post | Abduction pre/post | External rotation* pre/post | Internal rotation pre/post | Apprehension pre/post | VAS | Radiological findings pre |
| 1 | 160°/155° | 150°/120° | −35°/−45° | /LS | ± | 6/3 | L. BankartHill–Sachs >30% |
| 2 | 180°/180° | 180°/175° | −5°/−15° | /T12 | ± | 4/1 | L. Bankart |
| 3 | 180°/180° | 180°/180° | −0°/−0° | /T12 | −/− | 0/3 | L. Bankart |
| 4 | 180°/180° | 180°/180° | −0°/−5° | /L3 | +/+ | 0/0 | L. Bankart |
| 5 | 170°/160° | 175°/170° | −5°/−10° | /T12 | ± | 3/2 | L. BankartGlenoid defect >30% |
| 6 | 180°/180° | 180°/180° | −25°/−10° | /L3 | ± | 0/0 | L. Bankart |
| 7 | 175°/160° | 170°/175° | −0°/−5° | /T12 | +/+ | 0/1 | L. BankartHill–Sachs <10% |
| 8 | 180°/175° | 180°/180° | −0°/−0° | /LS | ± | 4/1 | L. BankartHill–Sachs <10% |
| 9 | 180°/180° | 175°/140° | −15°/−30° | /L3 | ± | 3/0 | L. Bankart |
| 10 | 155°/160° | 165°/155° | −0°/−0° | /T12 | ± | 2/0 | L. Bankart |
| 11 | 180°/160° | 180°/170° | −0°/−10° | /T7 | +/+ | 0/0 | L. BankartHill–Sachs <30% |
| 12 | 180°/180° | 180°/180° | −0°/−5° | /T7 | ± | 3/1 | L. Bankart |
| 13 | 180°/175° | 175°/150° | −5°/−15° | /T12 | +/+ | 3/2 | Coracoid pseudoarthrosis |
| 14 | 180°/180° | 180°/180° | −10°/−35° | /T12 | ± | 0/0 | L. BankartGlenoid defect <10% |
Post: postoperative; Pre: preoperative; VAS: visual analog scale.
All patients underwent a radiological study prior to revision surgery with at least 2 simple radiological projections, computed tomography (CT) and magnetic resonance imaging (MRI) studies, in order to evaluate a new detachment of the articular labrum, presence of associated cephalic or glenoid bone lesions and concomitant lesions in the rotator cuff. The most relevant findings of these preoperative imaging studies are also summarized in Table 1.
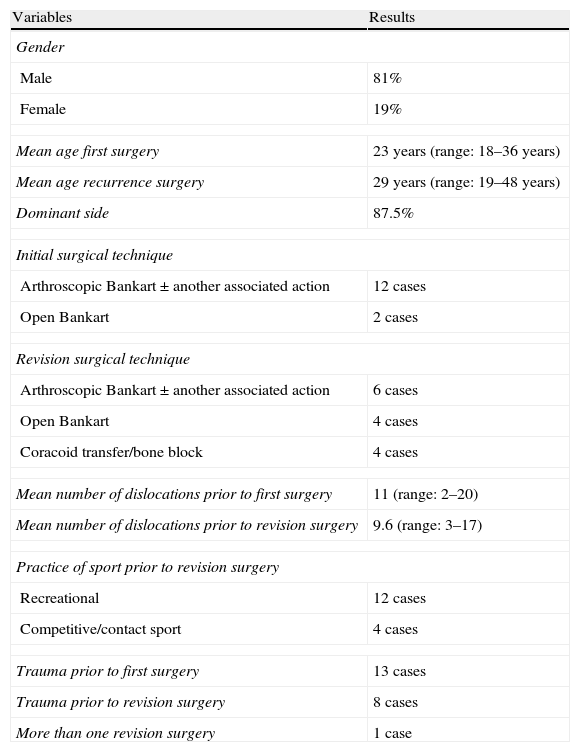
Epidemiological dataThe mean age of patients at the time of postoperative relapse was 29 years (range: 19–48 years). A total of 81% were male. The mean follow-up period was 57 months (range: 34–96 months) (from the completion of initial surgery until the revision conducted for the study). Failure of the initial surgery was associated with a clear history of trauma in 8 patients. We only found 1 case with more than 1 revision surgeries. The epidemiological data are collected in Table 2.
Epidemiological data.
| Variables | Results |
| Gender | |
| Male | 81% |
| Female | 19% |
| Mean age first surgery | 23 years (range: 18–36 years) |
| Mean age recurrence surgery | 29 years (range: 19–48 years) |
| Dominant side | 87.5% |
| Initial surgical technique | |
| Arthroscopic Bankart±another associated action | 12 cases |
| Open Bankart | 2 cases |
| Revision surgical technique | |
| Arthroscopic Bankart±another associated action | 6 cases |
| Open Bankart | 4 cases |
| Coracoid transfer/bone block | 4 cases |
| Mean number of dislocations prior to first surgery | 11 (range: 2–20) |
| Mean number of dislocations prior to revision surgery | 9.6 (range: 3–17) |
| Practice of sport prior to revision surgery | |
| Recreational | 12 cases |
| Competitive/contact sport | 4 cases |
| Trauma prior to first surgery | 13 cases |
| Trauma prior to revision surgery | 8 cases |
| More than one revision surgery | 1 case |
This assessment was performed using the Rowe,1 Constant17 (conducted independently for the operated shoulder and for the non-operated shoulder, measuring strength with a Basic-BFG dynamometer; Mecmesin) and UCLA18 scales and a visual analog scale (VAS).
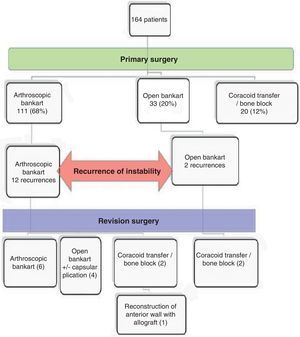
ResultsThe surgical procedures performed, both primary and following recurrence of instability, are summarized in Fig. 1.
In the initial surgery of the 14 patients, 12 were stabilized by arthroscopic reinsertion of the anteroinferior labrum (capsular plication of the lower axillary recess was also performed in 5 of these 12 cases), and a further 2 patients were stabilized by open surgery, reinserting the anteroinferior labrum and plicating the capsule. These 2 patients practiced contact sports, but we do not know whether this was the only reason for the choice of technique or if there was any presumption by the surgeon regarding an inability to achieve an optimal repair through an arthroscopic technique.
Six arthroscopic surgical revisions were performed, all of them on subjects who had previously undergone arthroscopic reinsertion of the anteroinferior labrum. A new disinsertion of the LLC was observed in all patients, with the complex being anatomically competent, so we opted for an arthroscopic procedure. Competence of the complex was initially established based on its characterization by MRI imaging in terms of volume and integrity. During surgery we verified once again its integrity and volume, as well as its ability to maintain the joint congruent once reinserted.
In 4 cases we observed the remains of 3 anchors and in 2 cases of 4 anchors from the previous surgical procedure. In 6 cases, in addition to labrum reinsertion we performed plication of the inferior capsular recess through the use of 4 implants. As in the primary surgery, this action was performed after observing a distended recess associated to a less competent LLC, both preoperatively and intraoperatively, with isolated reinsertion of the complex not offering sufficient intraoperative guarantees.
In this group we observed no evidence of bone lesions in the glenoid. In 1 case, as an additional action, we performed tenodesis of the infraspinatus muscle tendon and posterior capsule inside the bone defect of the humeral head (“remplissage”)19,20 due to the presence of a Hill-Sachs lesion affecting more than 30% of the humeral articular surface, which was not found during the first surgery and which hooked on the anterior rim of the glenoid with the arm in abduction and external rotation, hence leveraging the humeral head in an anterior direction (“engaging lesion”).
Four patients underwent reinsertion of the anteroinferior labrum with associated capsular plication through open surgery. All 4 subjects had previously undergone an arthroscopic Bankart repair technique which found no evidence of significant bone defects in the glenoid or the cephalic joint surface. These 4 patients underwent open surgery due to the presence of an incompetent LLC according to the criteria previously expressed. None of these cases associated significant bone defects.
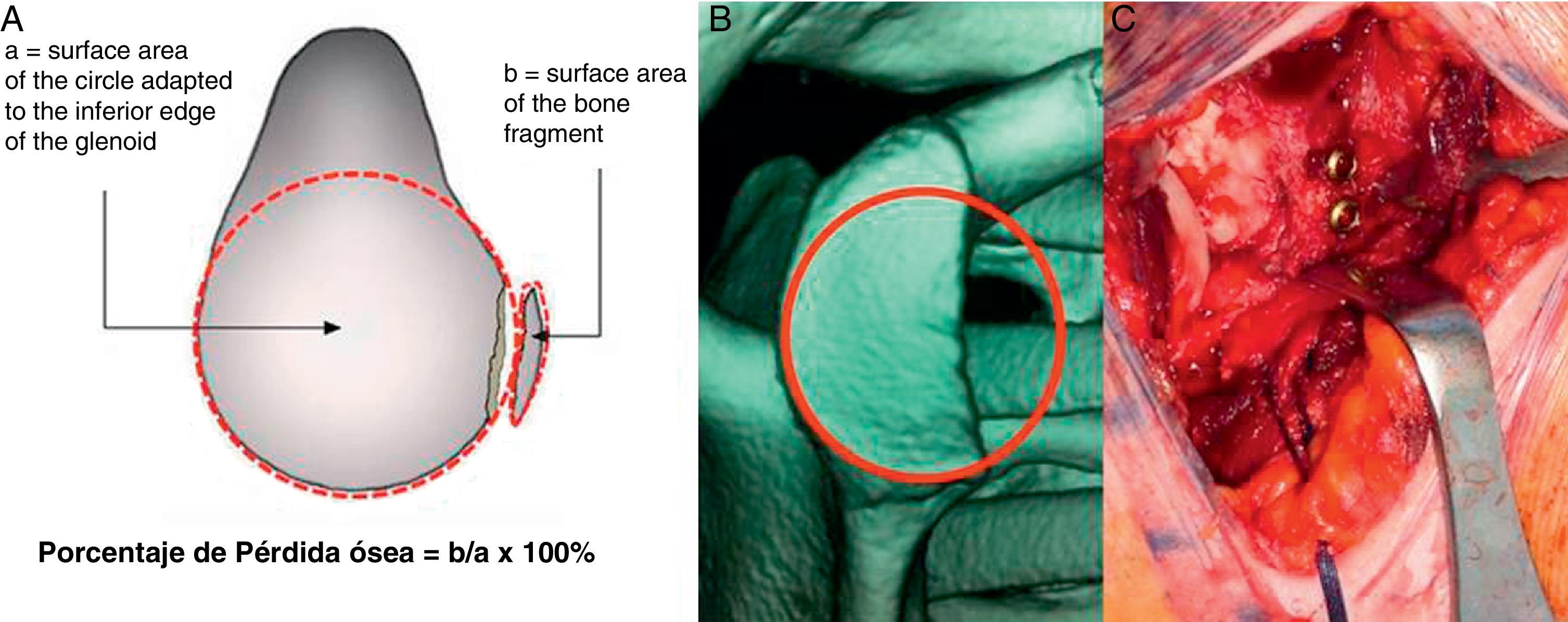
Finally, another 4 cases underwent a transfer technique of the coracoid apophysis (Latarjet technique). Of these, 2 cases had suffered failure of open labrum reinsertion and presented evident trauma, whilst the other 2 had suffered failures of arthroscopic labrum reinsertion. We chose this technique in 3 cases (failure of open surgery and failure of arthroscopic surgery) because it is a technique of choice in revision surgery for instability and also due to the familiarity of the surgeon performing the procedure. In another case it was selected due to the preoperative detection of a bone defect in the glenoid, with a size exceeding 30% (prior arthroscopic surgery) (Fig. 2).
Lastly, for 1 patient in our series this was the third surgical procedure. This subject had already undergone revision surgery through an open surgical technique (Bristow technique) at another center, following the failure of an initial arthroscopic surgery. The second surgery also failed, with the patient presenting persistent apprehension. These episodes of subluxation prevented him from practicing normal sports activities. The imaging study revealed the migration of the osteosynthesis material and coracoid which did not contact with the glenoid. Intraoperatively, we observed a deficit of the entire anterior wall, so we performed a reconstruction technique with a bone block on the glenoid through an Achilles allograft, reconstructing the middle and inferior glenohumeral ligaments.
Recurrence of instabilityAfter the initial surgery we found a recurrence rate (including the 2 patients whom we did not count in the final study of revision surgery) of 10.8% (12 cases) following the completion of an arthroscopic repair of the LLC, of 9.09% (3 cases) following open repair of the labrum with or without capsular plication, and of 5% (1 case) following surgery with coracoid transfer and/or bone blocks.
We found no cases of frank dislocation after the revision surgery, but we did find persistence of apprehension in 4 patients (25%), of which 3 were arthroscopic repairs, and 1 an open surgery (anterior wall reconstruction). This sensation did not alter the performance of work or daily living activities of patients. Thus, since it was not accompanied by excessive pain (VAS of 0–2) they did not wish to undergo another operation.
Clinical resultsThe Rowe scale score was excellent or good in 71.4% of patients. The scores obtained on the Constant scale in the intervened shoulder were excellent or good in 64% of patients, with a limitation of abduction below 161° in 4 patients, flexion below 161° in 5 patients, internal rotation in 5 patients and external rotation of 15–45° measured in abduction in 5 patients. None of the patients presented a deficit of external rotation greater than 45°. The UCLA scale scores were excellent or good in 64% of patients.
In total, 78.5% of these presented absence of pain below 1 according to the VAS and 85% (12 cases) returned to their previous work activity, with this activity involving physical effort of the intervened shoulder in 71% of cases. After revision surgery, 9 cases performed sports activity involving the affected arm.
Table 1 summarizes joint balance and the score on the VAS.
In relation to the causes of failure of the initial surgery, 8 patients suffered a clear history of trauma. In these 8 patients we found detachment of the labrum as a radiographic finding, and in 1 case a defect in the anterosuperior region of the cephalic surface greater than 30%, not present on imaging studies prior to the first stabilization surgery. In another patient with no prior evident history of trauma, the preoperative CT imaging tests identified a bone defect in the glenoid which had not been considered during the first intervention and which led to a reconstruction by coracoid transfer. The patient who had undergone a Bristow technique at another center presented a migration of the osteosynthesis material and the coracoid in the imaging tests. This was probably related to pseudoarthrosis (or nonunion) thereof. In the remaining 4 cases, the only radiographic finding we found was labrum disinsertion, with no other relevant bone defects (>30%) in the glenoid or cephalic surface.
DiscussionRecurrence of instability following surgery ranges between 4% and 18% after arthroscopic techniques and between 0% and 7% after open techniques,9 although these rates are becoming increasingly similar.3
In our study we found recurrence rates following primary surgery (open and arthroscopic) around 10%, which is in line with the findings of previous studies. Of this 10%, 75% (12 cases) followed arthroscopic surgery and 25% (4 cases) followed open surgery (labrum reinsertion and capsular plication bone block). Therefore, the incidence of recurrence after primary surgery depending on the technique employed which we found in our study proved to be 10.8% for arthroscopic reinsertion of the labrum, with or without associated plication, and 9.09% for open reinsertion of the LLC with associated capsular plication. The use of coracoid transfer techniques led to recurrence in 1 case (5%). Vooss et al.21 found rates similar to ours after arthroscopic stabilization. The recurrence rates of primary coracoid transfer techniques are relatively low. There are studies comparing this technique versus arthroscopic reinsertion of the labrum (Bankart procedure) showing superior functional results and lower recurrence rates.22 Our percentage (1 case out of 20 surgical procedures) was similar to that described by Burkhart after employing the Latarjet technique, reporting recurrence rates below 5%.6
In relation to relapses after revision surgery, the problem when studying different series lies in how to define recurrence of instability and, likewise, how to mark the success or failure of revision surgery. Failure can be defined as a frank dislocation, subluxation, persistent apprehension and even through the recent concept of “unstable painful shoulder” (UPS),23 with a painful shoulder representing the only manifestation of an otherwise unnoticed anterior instability. Although we have not recorded any cases of frank dislocation in our series, if we consider the presence of persistent apprehension as recurrence of instability, then our rate of recurrence would be 25% (4 cases), notably lower than that indicated in heterogeneous series intermingling different types of surgical techniques,13,16 like ours, which report relapse rates reaching up to 50%.
Although the percentages of recurrence after revision surgery are highly variable (reported rates range from 0% to 70%) numerous studies do agree that the results are worse in direct proportion to the number of revisions conducted.14,16 For this reason, it is essential that all anatomopathological findings are analyzed in detail during the first revision surgery, in order to select the correct technique and avoid another failure.
The presence of a new labrum disinsertion was the most common anatomopathological finding in our series, present in 14 shoulders which had undergone revision surgery.
The causes of recurrence can be multiple and can be summarized in 3 broad groups: misdiagnosis, technical errors and postoperative trauma. Most studies10,24 agree that one of the factors which influence the recurrence of instability is misdiagnosis (diagnosing posterior or multidirectional instability as anteroinferior instability), and especially the underdiagnosis of bone lesions, both in the glenoid and humeral head. Technical errors (non-anatomical repairs due to incorrect positioning of the anchors, inadequate tension of the capsule) are less frequent.25
In this sense, contrary to reports by other studies, significant, undiagnosed bone defects in the glenoid did not seem to play an essential role in the failure of primary surgery in our series (1 case out of 14). The primary cause identified was an evident history of trauma (8 out of 14). This may be related to the protocolized performance of a CT study at our center for patients with instability who are scheduled for an intervention.
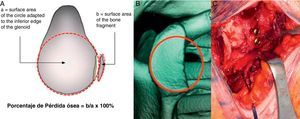
One of the dilemmas present in the literature is the definition of significant bone defect of the glenoid. Although most studies seem to agree that a bone defect is considered significant when it exceeds 25–30%,26,27 there is no such consistency in the measurement method thereof. Some studies use MRI to measure it, whereas some authors consider that this measurement method underestimates the amount of bone loss.28 We used three-dimensional reconstruction with humerus subtraction, and subsequently placed a circle coinciding with the bottom edge of the glenoid before measuring the defect as a percentage of the total glenoid surface. This technique, also used by other authors,29 seems to us (when this type of imaging test is available at a center) a simple method which reliably reproduces the size of the defect (Fig. 2).
Multiple techniques have been described for the reconstruction of the anteroinferior portion of the glenoid. Provided that the patient has not undergone a coracoid transfer previously, we prefer to use this technique rather than a bone block with tricortical iliac crest autograft due to the added dynamic compression effect exerted by the tendon assembly in a position of risk (external rotation and abduction). Moreover, we prefer to perform a Latarjet technique rather than a Bristow technique due to the increased coracoid contact surface in the former, which minimizes the risk of pseudoarthrosis, allows the placement of 2 screws and a greater increase of the reconstruction surface.
Posterosuperolateral bone defects of the humeral head (Hill-Sachs lesion), which are present in approximately 47% of patients,25 are also considered as a significant cause of instability recurrence when they reach a relevant size. Once again, the problem is the definition of “significant bone defect”. Some authors consider as significant a lesion larger than 20–40%, whilst others consider that a defect of 12% already has a biomechanical impact on stability.29 Recently, the orientation of a lesion is being increasingly considered more important than its size.10 In our series, 1 patient who had suffered previous trauma and recurrence presented a lesion over 30% in the imaging tests (CT and MRI) which, intraoperatively, was observed to hook on the glenoid in a position of abduction and external rotation. Therefore, in this case we added the surgical action of infraspinatus tenodesis (“remplissage”). Burkhart and de Beer10 emphasized the importance of recognizing these bone lesions in order to prevent failure of stabilization, reporting recurrence rates of up to 67% in patients with significant bone defects, compared to 4% in patients without such defects.
There are maximum deficit situations, such as the absence of the anterior wall. This loss is usually iatrogenic and does not leave many treatment options for its reconstruction except for the use of tendon allografts in an attempt to replace the static or osteotendinous stabilizers. Occasionally, chronic injury associated to the subscapularis muscle tendon may also require performing a pectoralis major muscle plasty, which is carried out through a subcoracoid approach.
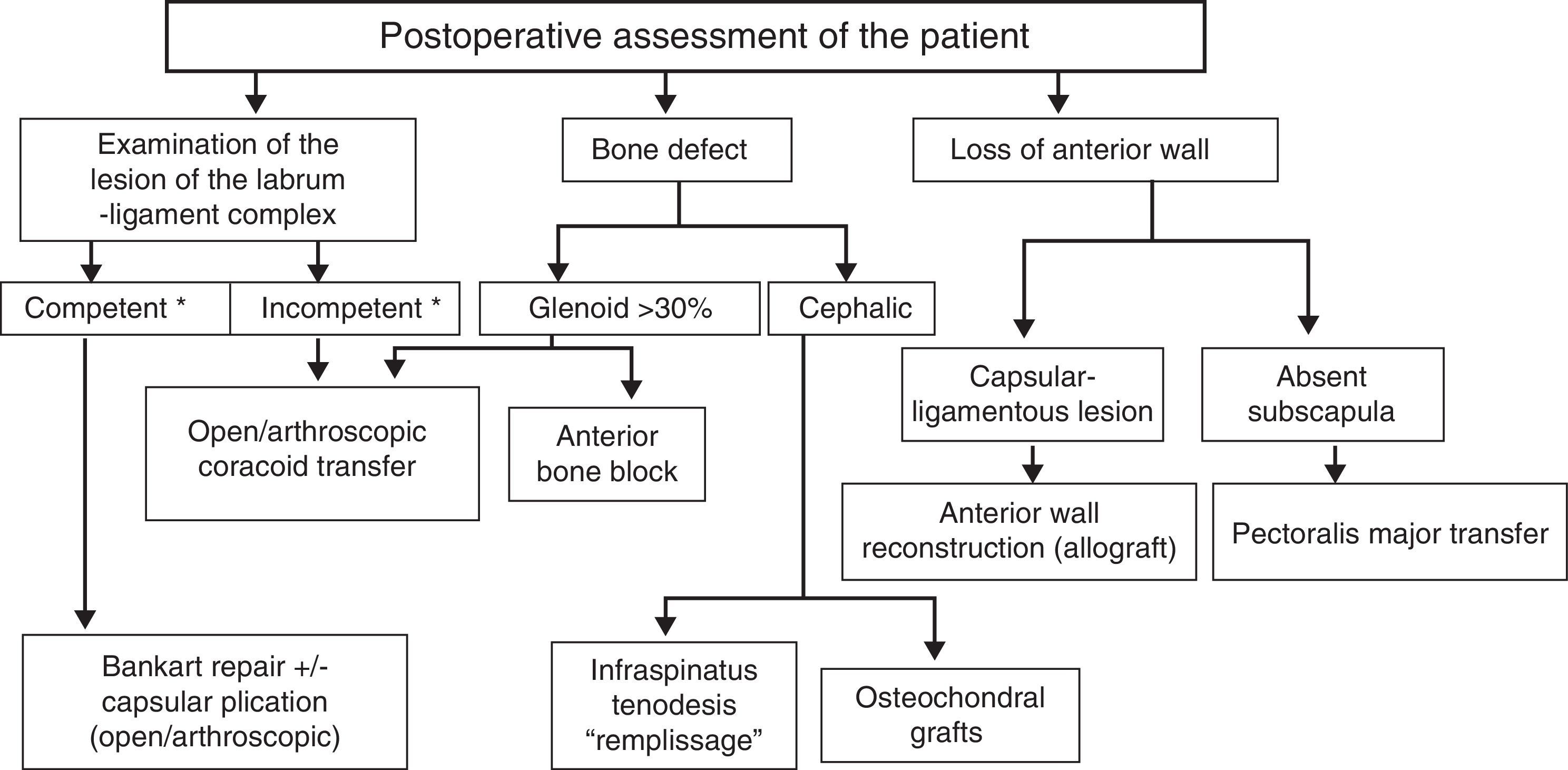
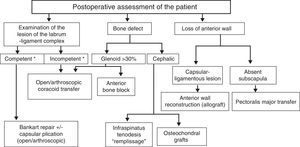
Protocols for initial surgical treatment of instability are perfectly established.11,12 Nonetheless, although the percentage of recurrence after primary stabilization is not negligible, the absence of clear action protocols which guide in therapeutic decision-making in cases of postoperative recurrence of instability is striking. After analyzing our series, we established guidelines to aid surgeons in selecting the technique to be used for instability revision surgery. Thus, after careful preoperative evaluation including complementary imaging studies, examination under anesthesia and arthroscopic findings, our recommendation would follow the guidelines summarized in Fig. 3.
Surgical action protocol for revision of instability. *Anatomically competent labrum-ligament complex: in a preoperative study with MRI a normal volume of the glenoid labrum despite its disinsertion, without losses of continuity or intrasubstance/breakages lesions; intraoperatively capable of maintaining the humeral head reduced after mobilization and repositioning.
In this series of 14 patients undergoing revision surgery for instability we have found no cases in which the technique selected initially had to be modified intraoperatively (i.e. changing from an open to an arthroscopic technique). However, the authors consider that this step is essential if the characteristics of the labrum or capsule are not adequate (excessively damaged labrum, significant capsular laxity), or if there is a significant bone defect in the glenoid and the surgeon does not have the necessary arthroscopic expertise to perform reconstruction with a bone block. Otherwise, the failure of revision surgery is all but assured.
Our own results indicate that if the choice of technique is correct, the functional results obtained are satisfactory in the vast majority of patients.
Study limitationsThis was a small and heterogeneous series which included both open and arthroscopic techniques. Thus, it did not allow us to infer results on a particular technique. Nevertheless, it brought us closer to understanding the functional results following revision surgery.
ConclusionsThe considerable variability in surgical techniques employed in this type of intervention highlights the multitude of factors which influence the recurrence of instability, as well as its anatomical and functional complexity. The application of surgical protocols as suggested herein for revision surgery following failure of the treatment of shoulder instability, should allow us to adapt the techniques to each individual, as well as to analyze the results in a rigorous manner while also improving future indications.
Level of evidenceLevel of evidence ii.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lópiz-Morales Y, et al. Cirugía de revisión de la inestabilidad anterior de hombro. Rev Esp Cir Ortop Traumatol. 2013;57:208–16.