Symptomatic posttraumatic arthritis of the elbow in young patients is a disorder for which there is currently no satisfactory solution. In this case report, we show the evolution of a comminuted fracture of the capitellum with trochlear extension (McKee type IV) treated initially with open reduction and internal fixation that eventually required a resurfacing hemiarthroplasty of the capitellum and reconstruction of the lateral ligament complex. After this surgical procedure, the patient had evident improvement of pain and of elbow range of motion, keeping the possibility of performing other rescue techniques open if they were to be necessary in the future.
El tratamiento de la artrosis postraumática sintomática del codo en el paciente adulto joven supone una patología que no tiene una solución satisfactoria en la actualidad. Presentamos en este caso clínico la evolución de una fractura conminuta del capitellum con extensión a la tróclea (tipo IV de la clasificación de McKee), que siendo tratada inicialmente con reducción abierta y fijación interna, requirió finalmente la implantación de una hemiartroplastia de resuperficialización del capitellum asociada a una reconstrucción del complejo del ligamento colateral externo. Este procedimiento quirúrgico ha supuesto para el paciente una mejoría evidente del dolor y del balance articular del codo, manteniendo intacta la posibilidad de realizar otras técnicas quirúrgicas de rescate si fuera necesario más adelante.
Coronal plane articular fractures of the distal humerus are rare in adults. They comprise around 6% of the total fractures affecting this anatomical area, most commonly involving the capitellum; the remainder of the trochlea can be involved in different ways. Similarly, they are characterised by the absence of involvement of the lateral or medial column of the humerus above the olecranon fossa.
CT scanning is often added to plain X-ray for diagnosis of these injuries. It enables better definition of the fracture with a view to planning treatment, and can identify more complex patterns than those that might initially appear on plain X-ray, with implications for later functional outcomes.1
Conservative treatment is reserved for fractures that are not displaced or if the patient has a major concomitant medical disease and very low functional demand. Surgical treatment is routinely open reduction and osteosynthesis using cannulated headless screws, it can also be necessary to implant a support plate if there is metaphyseal comminution.
Although good functional outcomes have been described in simple fractures that only affect the external articular region, when the injury extends to the remainder of the trochlea the outcomes can be can be appreciably poorer. Moreover, the onset of complications, such as lack of consolidation or avascular necrosis in the context of elbow instability, can result in a very debilitating condition for an active person, leaving the surgeon with the problem of finding a satisfactory surgical solution.
In the clinical case that we present below, we describe the evolution of a complex articular fracture of the distal humerus operated on several occasions, which eventually required implantation of a capitellar resurfacing prosthesis and the reconstruction of the external ligament complex by autologous ligamentoplasty with the palmaris longus and the tricipital fascia.
Clinical caseThe patient was a 41-year-old, right-handed manual worker who suffered a fall on his dominant arm when he left his house in December 2013.
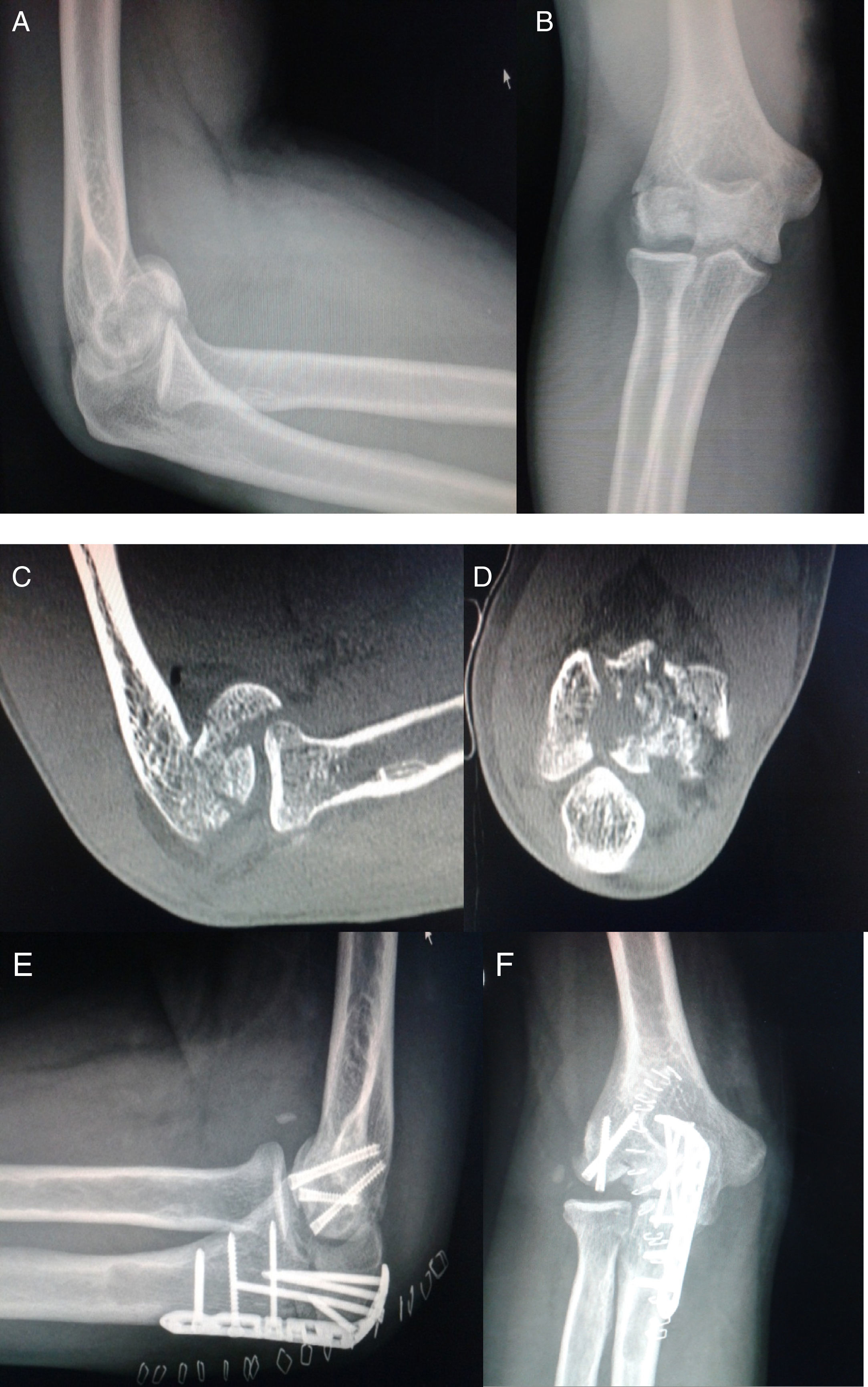
On admission to the Emergency Department, he presented pain and functional impotence in the right elbow, distal neurovascular examination was normal. Antero-posterior and lateral X-rays showed an articular fracture of the distal humerus with at least capitellar involvement (Fig. 1A, B). The affected limb was immobilised with a brachial-antebrachial splint and a CT scan revealed a capitellar fracture in various fragments with extension to the trochlea (Fig. 1C, D), the fracture was classified as a AO/OTA type B3.3 or Bryan and Morrey type IV, as modified by Mckee.2
The patient was operated 6 days after the trauma using a posterior approach with osteotomy of the olecranon. The fracture was synthesised with 3 Acutrak screws, 2 for the capitellar fracture and another for the fracture that was affecting the internal area of the trochlea. The osteotomy of the olecranon was closed using a plate (Fig. 1E, F).
During the first 2 months, the patient made good progress, and the pain and elbow joint range of motion gradually improved.
From the third month after the osteosynthesis, the patient reported an increase in pain, and had articular movement of 110° flexion, −10° extension, complete pronation and loss of 15° on supination, and noticed a “clicking” when performing certain movements. The appearance of the scar was normal, with no signs of infection. Antero-posterior and lateral X-rays showed avascular necrosis of the capitellum with protrusion towards the joint of part of the osteosynthesis material, therefore further surgery was proposed to the patient (and took place 8 months after the first operation) to remove these screws, since it was thought that they were the main cause of the pain.
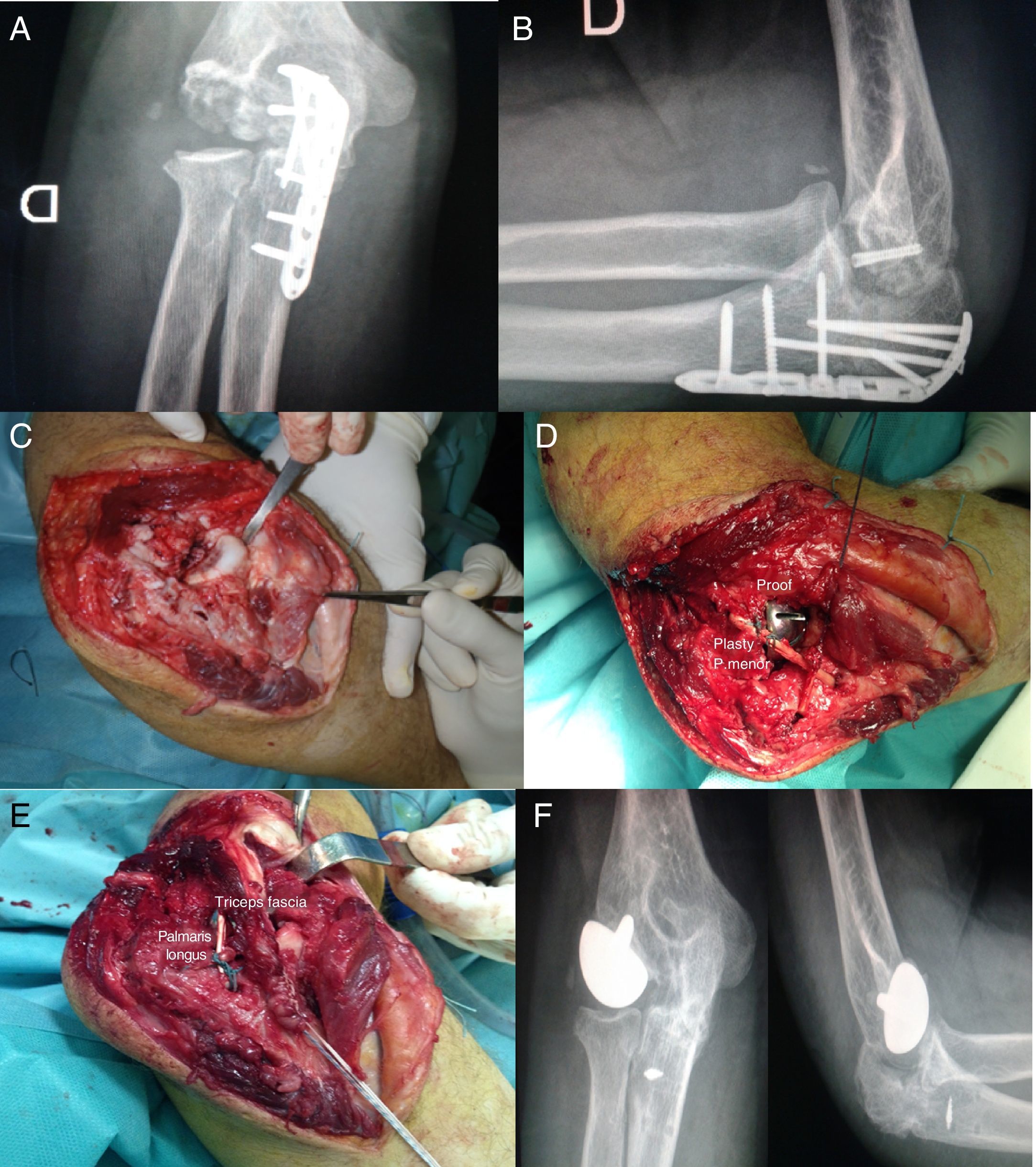
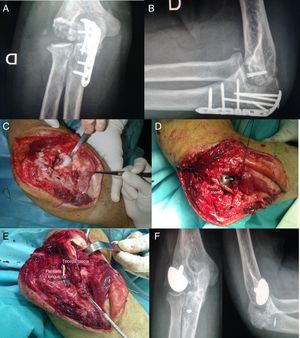
However, the patient continued to experience symptoms of pain, loss of strength and instability in the elbow on applying varus-valgus force. He also had pain in his right wrist and slight radial shortening of around 3mm compared to the contralateral wrist, which indicated some involvement of the interosseous membrane. An X-ray of the elbow showed significant degenerative changes in the capitellar region of the distal humerus (Fig. 2A, B).
From left to right and from top to bottom: (A and B) X-ray images that show arthritis of the capitellum (11 months after osteosynthesis). (C) Intraoperative image showing the appearance of the capitellum with major degenerative changes, 16 months after osteosynthesis. (D) Image with the test component of the hemiarthroplasty prosthesis. (E) Implanted prosthesis and stabilisation with ligamentoplasty. (F) AP and lateral X-ray image one year after the resurfacing hemiarthroplasty.
Therefore, 14 months after the osteosynthesis, and after assessing the different surgical options bearing in mind the type of injury, and the age and activity of the patient, an implantation of a metal hemiarthroplasy and capitellar resurfacing was decided (LRE, Biomet, United Kingdom). The surgical approach was over the previous scar before the posterior approach, but creating an antero-external extension of same, on elevating the insertion of the extensor musculature of the fingers and the anterior capsule to achieve correct visualisation of the external joint area. We only had two prosthetic sizes of the capitellar component, which had to be implanted in line with the epicondylar column forming an angle of about 60° with the longitudinal axis of the humerus. This position was determined with needles using a system of cannulated guides. The prosthesis was cemented to improve anchoring due to the bone loss in the capitellum. The joint surface of the radial head was acceptable in appearance although it had an eccentric marginal injury (possibly caused by the protrusion of the screws) for this reason it was not prosthetised. Due to the absence of competence of the lateral ligament complex of the elbow, which had in reality been replaced by fibrous tissue, we used an autologous plasty for its reconstruction obtained with the tendon of the palmaris longus supplemented with tricipital fascia, fixing it through bone tunnels to a metal anchorage (Fig. 2C–E).
The elbow was immobilised postoperatively with a brachial-antebrachial splint for 2 weeks, then rehabilitation treatment commenced.
ResultsAlready in the first weeks after the hemiarthroplasty, the patient reported very significant improvement in his symptoms, the pain had disappeared and in the projection that presented when he forced the articular movement of the elbow.
The X-ray one year after implantation of the prosthesis and reconstruction of the ligament, showed correct joint alignment with no radiological signs of loosening (Fig. 2F), with some degenerative changes in the cubito-humeral joint but with no functional impact.
On clinical examination at 18 months after the operation, the patient had almost complete range of motion of the elbow, with a loss of 10° in flexion and 5° in extension compared to the contralateral elbow. Pronosupination was normal, and the patient only reported occasional discomfort that did not require any form of analgesia.
The patient experienced major improvement in elbow function, from a score of 60 points on the Mayo Elbow Performance Score (MEPS) at the consultation prior to the resurfacing arthroplasty, to 85 points after the procedure.
The patient is currently working and is able to perform non-contact sports using the operated limb.
DiscussionSymptomatic post-traumatic arthritis of the elbow in young adults currently has no satisfactory solution; a search of the bibliography revealed few references to this disorder. If conservative treatment fails, we can indicate various surgical procedures to achieve clinical improvement. Of the different options, we attempt to avoid total elbow arthroplasty in this population, since complications associated with the survival of the implant are very common due to the group's high physical demands.
Articular fractures of the external column of the humerus are usually caused by a fall on the hand or elbow, and the force is transmitted from the radial head to the external region of the trochlea, almost always creating bone disruption in the coronal plane. Diagnosis is achieved by clinical examination and anteroposterior and lateral X-rays, the latter occasionally shows projection of the “double arch sign”. If this sign is not seen, this might be due to the internal rotation of the capitellum and the trochlear component in Mckee type IV fractures.3
A CT scan of the elbow is recommended so as not to underestimate these injuries, to better define their morphology and demonstrate the presence of medial extension towards the trochlea, metaphyseal comminution, radial head injury or ligament involvement. This will enable us to choose the most appropriate surgical approach to fully expose the fracture, increasing the possibilities of obtaining a better functional outcome having achieved improved anatomical restitution.4 In our case we used the posterior approach with osteotomy of the olecranon in an attempt to achieve the widest articular view possible, since there was also medial joint involvement; although it is true that with external Kocher or Kaplan approaches the two most external thirds of the distal humerus joint surface can be well visualised.
Headless cannulated screws are used for osteosynthesis of fractures in this anatomical region, to provide rigid fixation of the articular fragments. On occasion, if these fragments are too small to be synthesised they are removed. It can also be necessary to use support plates and a graft if there is significant bone loss in the metaphyseal area.
“Acute” capitellar joint replacement has been described but is not routinely used. Preservation of the capitellum using osteosynthesis techniques is recommended, especially in young patients, since its removal can cause posterolateral instability of the elbow if the collateral ligaments are involved.
The complications of articular fractures of the distal humerus include a loss of the elbow's full range of motion, avascular necrosis, pain, degenerative articular changes and instability. The latter is sometimes discovered even after consolidation of the fracture. Avascular necrosis secondary to a capitellar fracture is not a common complication, ranging between 0% and 30%.5 Therefore, is it recommended that synthesis should be attempted even if the bone fragments are not anchored to the soft tissues.
The incidence of post-traumatic arthritis is quite low in the series consulted. In our case, we had a capitellar fracture in several fragments majorly involving and impacting the joint cartilage, as can be seen on the CT slices, and might have been a determining factor for the early development of arthritis of the external joint compartment that occurred. In our patient there was also associated instability on applying valgus force to the elbow and pain in the wrist, which was not appreciated on the initial examination after the osteosynthesis.
The two surgical options that we thought were most appropriate in this case can be summarised as follows:
First, to perform an interposition arthroplasty in the radial-capitellar joint compartment with the anconeus, debriding the affected articular areas in the same procedure. This method has been used successfully on occasion for the treatment of arthritis in the elbow,6 but several previous operations might involve muscular damage and fibrosis, and therefore it might be difficult to interpose this muscle effectively.
The technique we used was to perform a capitellar resurfacing hemiarthroplasty exclusively, since the humero-cubital7 joint was sufficiently preserved. Full joint replacement of the elbow was discounted for this reason, and due to the patient's age.
This surgical procedure is rarely used and can be undertaken together with the prosthetic replacement of the radial head, if it is also involved.8,9 In this case, we did not consider replacing the radial head as we found it to be acceptable on surgical examination and because this was a young patient. In line with the opinion of other authors,10 arthroplasty of the radial head can be performed later if degenerative changes appear with clinical repercussions.
The other point that was difficult to resolve was stabilisation of the lateral compartment of the elbow, because the external lateral ligament had been replaced by incompetent fibrous tissue, and we used an autologous ligamentoplasty with the palmaris longus reinforced with tricipital fascia. Ligamentoplasty is the most usual procedure to solve this type of instability.
To conclude, we must highlight that the use of capitellar resurfacing arthroplasty to treat the sequelae of articular fractures of the external column of the humerus can, in selected cases, significantly improve these patients’ quality of life, in eliminating or significantly reducing symptoms of pain, maintaining a good range of movement in the elbow, and finally–and we consider this an important factor–it does not rule out the possibility of other rescue techniques such as allograft of the distal humerus or total elbow arthroplasty if necessary in the future.
Level of evidenceLevel of evidence: V.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that neither human nor animal testing have been carried out under this research.
Confidentiality of dataThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
Associate Professor at the Complutense University of Madrid.
Please cite this article as: Aroca-Peinado M, Cecilia-López D, Jiménez-Díaz V. Artroplastia de resuperficialización como alternativa a las secuelas postraumáticas de la columna externa del húmero en el adulto joven. Rev Esp Cir Ortop Traumatol. 2018;62:80–85.