In this study we evaluate the treatment of displaced mid-shaft clavicle fractures or comminuted fractures with a third fragment using a superior anatomic plate.
Materials and methodsA retrospective study was conducted on 34 patients operated on between January 2006 and June 2010 with this type of fracture. Mean follow-up was 25 months (6–54 months). By Robinson Classification, 12 cases were type 2B, 17 type 2B1 and 5 type 2B2. Clinical evaluation was performed with the VAS and Constant test. For the radiological evaluation, we used neutral AP projections, and another with 30° of cranio-caudal inclination.
ResultsThe mean pre-operative VAS was 6.5 (4–8) and the postoperative was 1 (0–2). The mean Constant test score was 85, with 30% good results and 70% excellent results. The mean consolidation time was 14 weeks.
ConclusionInternal fixation of comminuted fractures with an anatomic plate, particularly those with a vertical third fragment and fracture types 2B, 2B1 and 2B2, provides a good treatment option, as it gives good functional results and minimises the incidence of non-union.
En este estudio valoramos el tratamiento de las fracturas desplazadas de la clavícula con un tercer fragmento o con conminución mediante la osteosíntesis con una placa anatómica y de bajo perfil colocada en la cara superior.
Material y métodoEstudio retrospectivo de 34 pacientes intervenidos desde enero de 2006 hasta junio de 2010, con fracturas de tercio medio de la clavícula conminutas o con tercer fragmento. El seguimiento medio ha sido de 25 meses (6–54 meses). Según la clasificación de Robinson 12 casos eran del tipo 2B, 17 del tipo 2B1, y 5 del tipo 2B2. La valoración clínica se realizó mediante la puntuación obtenida en la escala visual analógica (EVA) y en el test de Constant. La valoración radiológica preoperatoria y durante el seguimiento se llevó a cabo mediante proyecciones AP, una neutra y la otra con haz de Rx inclinado caudocranealmente 30°.
ResultadosLa puntuación media en la escala EVA preoperatoria fue de 6,5 (4–8) y la postoperatoria de 1 (0–2). La puntuación media en el test de Constant fue de 85, con un 30% de casos con buenos resultados y un 70% de excelentes. El tiempo medio en obtener la consolidación fue de 14 semanas.
ConclusionesLa fijación interna con placa anatómica de las fracturas conminutas de la clavícula, especialmente si presentan un tercer fragmento vertical, o fracturas tipo 2B, 2B1 y 2B2, constituyen una buena opción de tratamiento dado el buen resultado funcional y la baja incidencia de pseudoartrosis que presentan.
Clavicular fractures make up approximately 4% of all fractures in adults, affecting the middle third of the clavicle in 80% of cases.1,2 This kind of fracture has traditionally been treated orthopaedically but the literature is beginning to describe pseudoarthrosis rates of up to 15% with this kind of treatment in the case of displaced fractures.3–5
The onset of pseudoarthrosis usually translates clinically into pain, distal neurological problems and, in consequence, a functional deficit of the upper limb.6,7 Although it has been proposed to treat this complication with endomedullary devices or external fixation, the technique providing the best results consists in the internal fixation with a compression plate and the provision of a bone graft.8,9
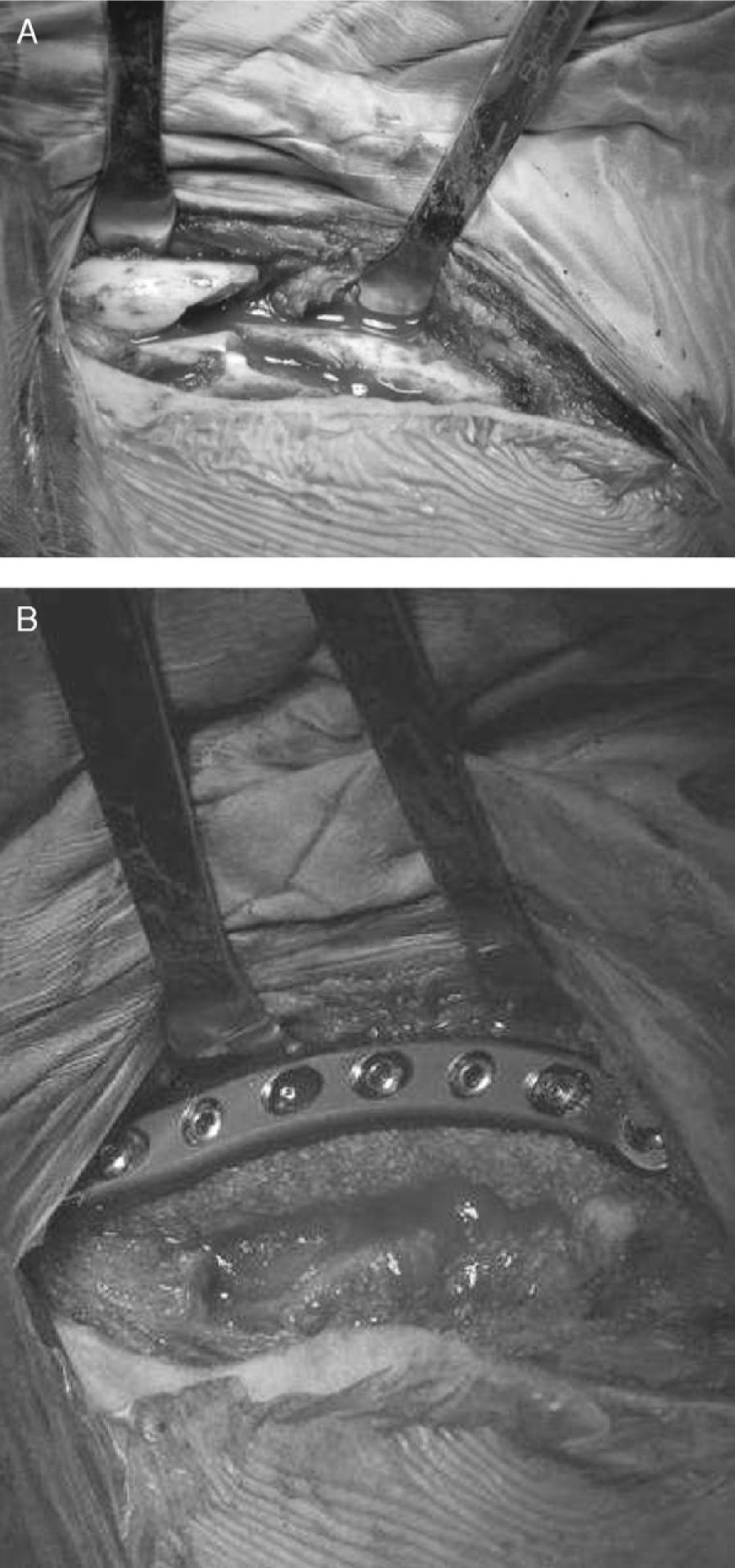
In this study, we attempt to assess the result obtained after the treatment of displaced comminute fractures (Fig. 1) or with a third fragment of the middle third of the clavicle through osteosynthesis with a low-profile anatomical plate placed on the upper face of the bone.
Materials and methodsBetween January 2006 and June 2010, we conducted a retrospective study that included 34 patients undergoing surgical treatment and presenting a displaced fracture of the middle third of the clavicle (Fig. 2). The exclusion criteria were open fractures, under 18 or over 60 years of age, fracture of the proximal or distal third, associated nerve lesions, associated fractures on the same or the contralateral side, previous fractures of the clavicle, abnormal function on the injured side or inflammatory or rheumatic disease. Twenty-nine of the cases were male and five females, with a mean age of 43 (19–57 years). The mechanism causing the injury was a traffic accident in 22 cases, sports-related trauma in 7 and falls in 5. In terms of laterality, 8 were affected in the left clavicle and 26 in the right. The classification of clavicular fractures proposed by Robinson2 was used and 12 cases corresponded to type 2B fractures, 17 were type 2B1, and 5 were type 2B2.
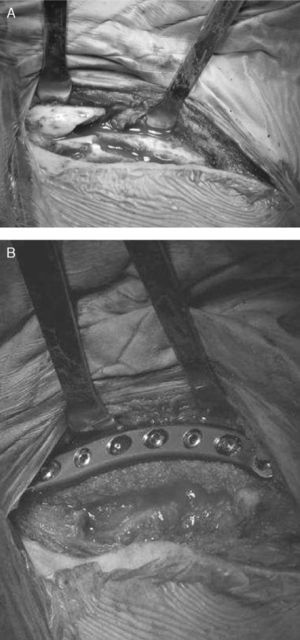
All patients were operated on by the same surgeon. Placed in the deckchair position, the approach used followed the longitudinal axis of the clavicle. Once the ends of the fracture were located, a currettage was performed on the focus, releasing any interposed soft tissue and temporarily reducing the fragments with reduction clamps. The definitive fixation of the clavicle was done through a preshaped anatomical plate always placed on the upper face (Acumed, Hillsboro, OR®). In 15 of the 34 patients (44.1%), in whom more than three weeks had elapsed since the fracture, a bone substitute (BMX, Synthes® Oberdorf) was used (Fig. 3).
All cases were immobilized with a Gilchrist brace for 10 days, after which rehabilitation treatment was started. Clinical assessment was performed using the analogue visual scale (AVS), with a range from 0 (no pain) to 10 (severe pain), and using the Constant test. The maximum score on this test is 100 and it includes 4 items: pain (15 points), activities of daily life (20), joint balance (40) and strength (25). As for radiological evaluation, all patients were subjected to AP projections, one neutral and the other with the X-ray beam angled 30° in a caudocranial direction. The reduction obtained, the degree of consolidation and the onset of complications were all assessed. X-rays were taken in the immediate post-operative phase, after three months, 6 months and at the end of the follow-up.
ResultsThe mean score on the AVS scale prior to surgery was 6.5 (4–8), and 1 (0–2) post-operatively. The Constant test was performed at the end of the follow-up and the mean score obtained was 85, with 30% of cases showing good results and 70% excellent.
Among the complications, two cases (5.8%) presented a delay in consolidation. One of them ended up consolidating while the other developed pseudoarthrosis with loosening of the plate, requiring repeat surgery for the placement of a new plate and the provision of an autologous graft of iliac crest bone. These delayed consolidation and pseudoarthrosis cases coincided with patients who had been first operated on more than three weeks after sustaining the fracture.
One patient presented discomfort with the plate when carrying out day-to-day activities and requested the removal of the osteosynthesis material. Another 7 patients had some discomfort in the scar area, although these disappeared completely by the end of the follow-up. The mean follow-up was 25 months (6–54 months).
With regard to consolidation, this was achieved with a mean time of 14 weeks (8–42 weeks). For the radiological evaluation of fracture consolidation, the passage of bony bridges between the fracture fragments was observed (Fig. 4). In 7 cases, a computed tomography was also requested to confirm consolidation.
DiscussionThe treatment of clavicular fractures has classically been conservative. However, there are numerous studies indicating the onset of complications with this approach. The most frequent of these are pseudoarthrosis, hypertrophic callus, functional impotence under stress, etc.10,11. In the multicentric randomized trial carried out by the Canadian Orthopaedic Trauma Society in 2007 on a total of 134 patients (65 treated conservatively and 67 by fixation with a plate), those treated surgically were seen to have a better clinical and radiographic outcome than those given conservative treatment, with a lower incidence of symptomatic consolidations in an incorrect position and pseudoarthrosis. The conclusion drawn from this study was that surgical treatment is more recommendable for this sub-group of clavicular fractures.12
Although there is still some controversy about whether the best osteosynthesis system for the clavicle is to use plates or endomedullary devices,13 we feel that, in cases with comminute fractures or those with a third fragment, the placement of an anatomic achieves greater stability, favouring the consolidation process. In our series, comparable with others in which the same material has been used and with similar fracture patterns,13 it was necessary to regret a single case of pseudoarthrosis due to material failure. For this reason, we believe that the treatment of comminute fractures, especially those with a third vertical fragment, must be eminently surgical as it avoids the onset of symptomatic hypertrophic calluses and also minimizes the rate of pseudoarthrosis. In this sense, it is not the same to operate on a clavicular fracture in the acute phase as in the pseudoarthrosis phase. It is well known that the outcomes obtained after surgical treatment of a pseudoarthrosis are not as satisfactory as after operating on a clavicular fracture in the acute phase.14–16 Rosenberg et al.14 studied 13 patients with pseudoarthrosis of the clavicle treated with a plate and followed up for 41 months. They observed that only 46% of patients returned to their normal working and leisure activities prior to the fracture, with only three patients being totally pain-free. They conclude that, even if stable fixation is achieved with this method, patients’ clinical condition may persist.
The limitations of our study include the fact that some patients were given a bone graft while others were not, based solely on chronological criteria, and this could distort the results. Bone grafts were placed in comminute fractures or those with a third fragment of clavicle when more than three weeks had passed since the injury was sustained. Nonetheless, all patients who underwent surgery, with or without graft, achieved bone consolidation.
In conclusion, we can state that internal fixation with an upper anatomical plate of comminute diaphyseal fractures of the clavicle, especially with a third vertical fragment, constitutes a very valid option in the fractures under study, i.e. Robinson types B, 2B1 and 2B2, as a good functional result is obtained and the incidence of pseudoarthrosis is minimized.
Level of evidenceLevel of evidence: IV.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflict of interests to declare.
Please cite this article as: Moya E, et al. Tratamiento quirúrgico de las fracturas diafisarias y conminutas de la clavícula mediante placa anatómica de bajo perfil. Rev Esp Cir Ortop Traumatol. 2012;56(2):127-131.