The aim of this study is to assess the time to return to work (TRW) in patients undergoing trapezial resection using the Mini TightRope® system at our centre and to investigate factors that might delay return to work following this surgery.
Material and methodsA retrospective study was conducted on patients who underwent Trapezial resection and suspensionplasty using the Mini TightRope® system between 2015 and 2016, with a minimum one-year follow-up. Telephone interviews were conducted along with a review of medical records and radiology reports, as well as temporary work disability documents, collecting epidemiological and occupational data. Groups were compared based on age, gender, dominant hand, biomechanical occupational requirements of the patients, and whether they had experienced prior temporary work disability.
ResultsA total of 36 patients (29 women and 7 men) with an average age of 55.7 years were included. The median time to return to work was 126 days. Self-employed workers re-entered the workforce 72 days earlier on average; workers who had experienced prior temporary work disability had a greater total temporary work disability duration and took 91 days longer to return to work compared to those who had not.
ConclusionsPatients employed by others and those who had experienced prior temporary work disability before the surgery had longer temporary work disability periods. In our study, no differences were observed based on gender, dominant hand, or biomechanical work demands of the intervened patients.
El objetivo de este estudio es evaluar el tiempo de reincorporación al trabajo (TRW) en pacientes sometidos a resección trapecial utilizando el sistema Mini TightRope® en nuestro centro e investigar factores que podrían retrasar el reincorporación al trabajo después de esta cirugía.
Material y métodosEstudio retrospectivo de los pacientes a los que se realizó una trapecectomía y artroplastia de suspensión mediante el sistema Mini TightRope® entre los años 2015 y 2016, con un seguimiento mínimo de un año. Se realizó una entrevista telefónica y una revisión de la historia clínica y de la radiología, recogiendo datos epidemiológicos y laborales. Se compararon los grupos por edad, sexo, mano dominante y requerimientos profesionales biomecánicos de los pacientes, así como haber estado en incapacidad laboral temporal (ILT) previo a la cirugía.
ResultadosSe incluyeron un total de 36 pacientes (29 mujeres y 7 varones) con una edad media de 55,7 años. La mediana para la vuelta al trabajo fue de 126 días. Los trabajadores autónomos se reincorporaron 72 días antes (p=0,004); los trabajadores que estaban en ILT previa a la cirugía tuvieron una ILT total mayor, y tardaron en volver al trabajo 91 días más que aquellos que no lo estaban (p<0,001).
ConclusionesLos pacientes que trabajan por cuenta ajena y aquellos que estuvieron en ILT previa a la cirugía presentaron tiempos de ILT mayores. En nuestro estudio no encontramos diferencias por sexo, mano dominante o grado biomecánico laboral de los pacientes intervenidos.
Trapeziometacarpal osteoarthritis is the second most common degenerative disease of the hand, after osteoarthritis of the distal interphalangeal joint. Its prevalence increases over the years, affecting mainly postmenopausal women in 25–33%.1–5 This disease affects a working population, with strong impact on the patient and the health systems. There are several surgical techniques described for its treatment, such as trapeziectomy combined with some type of ligamentoplasty, trapeziometacarpal (TMC) arthrodesis, osteotomy of the first metacarpal, or TMC prostheses. There is not enough quality scientific evidence to demonstrate the superiority of any of the aforementioned.6
Occupational disability is the situation that occurs when a worker is no longer able to perform the usual functions of his or her job, either due to illness or accident.7
To our knowledge, there is no study that analyses the time to return to work (TRW) after trapeziectomy with an associated first metacarpal suspension system with Mini TightRope® (Arthrex).
The objective of this study was to assess the average times of temporary occupational disability (TOD) in patients operated on in our centre during the years 2015 and 2016 using open trapeziectomy and the Mini TightRope® (Arthrex) suspension system.
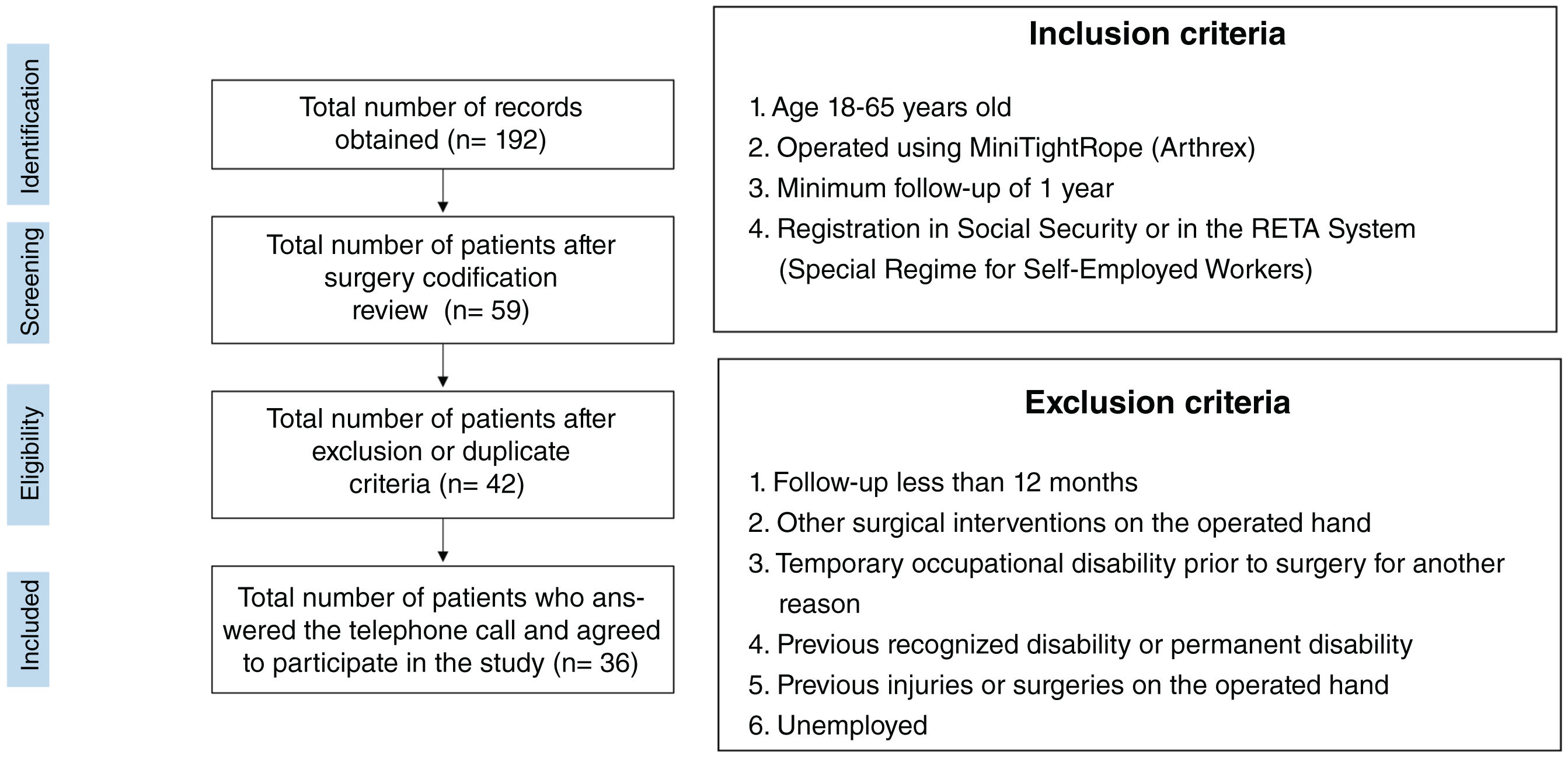
Material and methodOur study is a retrospective observational study, in which we reviewed the surgical procedures coded as “Arthroplasty with/without carpometacarpal implant”, as well as “Carpometacarpal arthrodesis” in our computerised record of medical records between January 2015 and December 2016. One hundred and ninety-two records were recovered. The operating room report was reviewed for these 192 records with a total of 133 records being discarded due to incorrect surgery coding. Following this, a total of 59 TMTR records were included. After reviewing their medical records, another 17 patients who did not meet inclusion criteria in the study or presented exclusion criteria were discarded (Fig. 1). Of the total 42 patients, 36 answered the telephone call, all of them giving their consent for inclusion in the study by signing the informed consent form.
The study stages are shown: identification, detection, eligibility and inclusion. Of the 192 patients initially identified, 59 had undergone a trapeziectomy and Mini TightRope® suspension system. After applying the exclusion criteria, the number of eligible patients was reduced to 49. Finally, 36 patients were included in the study after considering those who responded to telephone calls and agreed to participate. The inclusion and exclusion criteria are also shown on the right of the figure.
Demographic data were collected for each patient, including age, sex, dominant hand, medical history, and operated hand. The degree of manual biomechanical loading of each patient was defined based on the “Professional Assessment Guide” of the National Institute of Social Security, with a maximum grading of 4 and a minimum of 1.8
In the telephone interview, the type of work, occupational situation at the time of surgery, together with their degree of satisfaction were recorded on an analogue scale from 1 to 10 (one being the poorest result and 10 the best).
The preoperative X-ray, the postoperative X-ray 12 months after surgery, and the clinical notes were reviewed.
Return to work was defined as the day immediately following the final date of the TOD report issued by each patient's primary care physician.
Statistical analysisThe study of TOD time for the study group was carried out using the Kaplan–Meier method, with survival curves plotted. Performing TOD time analysis in relation to the other variables, the Mann–Whitney U test was used; The dependent variable was the time of TOD and the independent variables were sex, dominant hand, being on TOD prior to surgery, employment status (employee or self-employed) and the employment level of each patient. To evaluate the relationship between TOD time and Eaton–Lambert grade, the Kruskal–Wallis test was used. A p<.05 was considered a statistically significant result.
Surgical techniqueThe patient was placed in the supine position with forearm on a hand table. Surgery was performed by dorsal or volar Wagnerr approach. Dissection was performed and the sensory branches of the radial nerve protected. Part of the Abductor pollicis brevis was released from the base of the first metacarpal and a longitudinal capsulotomy was performed. We freed the trapezius from its ligamen insertions subperiosteally, protecting the radial artery in the most proximal area. Without having yet performed the trapeziectomy, the 1.1mm Kirschner wire (K-wire) of the Mini TightRope® system was passed from the base of the first metacarpal to the second metacarpal. We used this technique so that the trapezius would help us maintain a good height of the first metacarpal when passing through the guide wire. In the expected exit area of the K-wire we made a longitudinal incision (between the 2nd and 3rd metacarpal), we elevated the 2nd interosseous muscle subperiosteally and found the K-wire, which we advanced until we could pass the FiberWire® suture, but without tying it in the 2nd metacarpal, leaving the suture held by mosquito forceps. There are usually some branches of the dorsal radial sensory nerve that must be identified and protected in the incision. We then proceeded to trapeziectomy and performed the associated release of the carpal tunnel using this trans-trapezial approach, as described by Sless et al.9 When performing trapeziectomy, the superficial lamina of the transverse carpal ligament (TCL) is usually sectioned; The remaining part is usually released with scissors. We then retract the Flexor carpi radialis and proceed to section the deep portion of the TCL. Once this is done, we tie the FiberWire® suture over the button in the 2nd metacarpal. Ischaemia is released, we perform coagulation and proceed to closure. In the postoperative plan we include a splint for 2 weeks, followed by a thumb orthosis for another 2 weeks in which the patient can perform passive and active-assisted movements and then begin rehabilitation for 4 more weeks with 2 weekly sessions. Stitch removal is usually done after 10–12 days.
ResultsA total of 36 patients were included in the study. The patient characteristics are summarised in Table 1.
General study sample characteristics.
| Characteristics | Value |
|---|---|
| Age, mean years (SD) | 55.7 (5.6) |
| Sex, n (%) | |
| Women | 29 (80.6) |
| Men | 7 (19.4) |
| Employment level, n (%) | |
| Grade 2 | 4 (11.1) |
| Grade 3 | 31 (86.1) |
| Grade 4 | 1 (2.8) |
| Dominant hand, n (%) | |
| Right | 35 (97.2) |
| Left | 1 (2.8) |
| Hand operated on, n (%) | |
| Right | 15 (41.7) |
| Left | 21 (58.3) |
| Dominant side operate on, n (%) | |
| Non dominant | 20 (55.6) |
| Dominant | 16 (44.4) |
| Workers, n (%) | |
| Self-employed | 12 (33.3) |
| Employee | 22 (66.7) |
Patients with TOD prior to surgery returned to work at 214 days (P25; P75: 154; 255); those who were not on TOD prior to surgery returned to work at 123 days (P25; P75: 92; 193), with this difference being significant as a p<.001.
SD: standard deviation; TOD: temporary occupational disability.
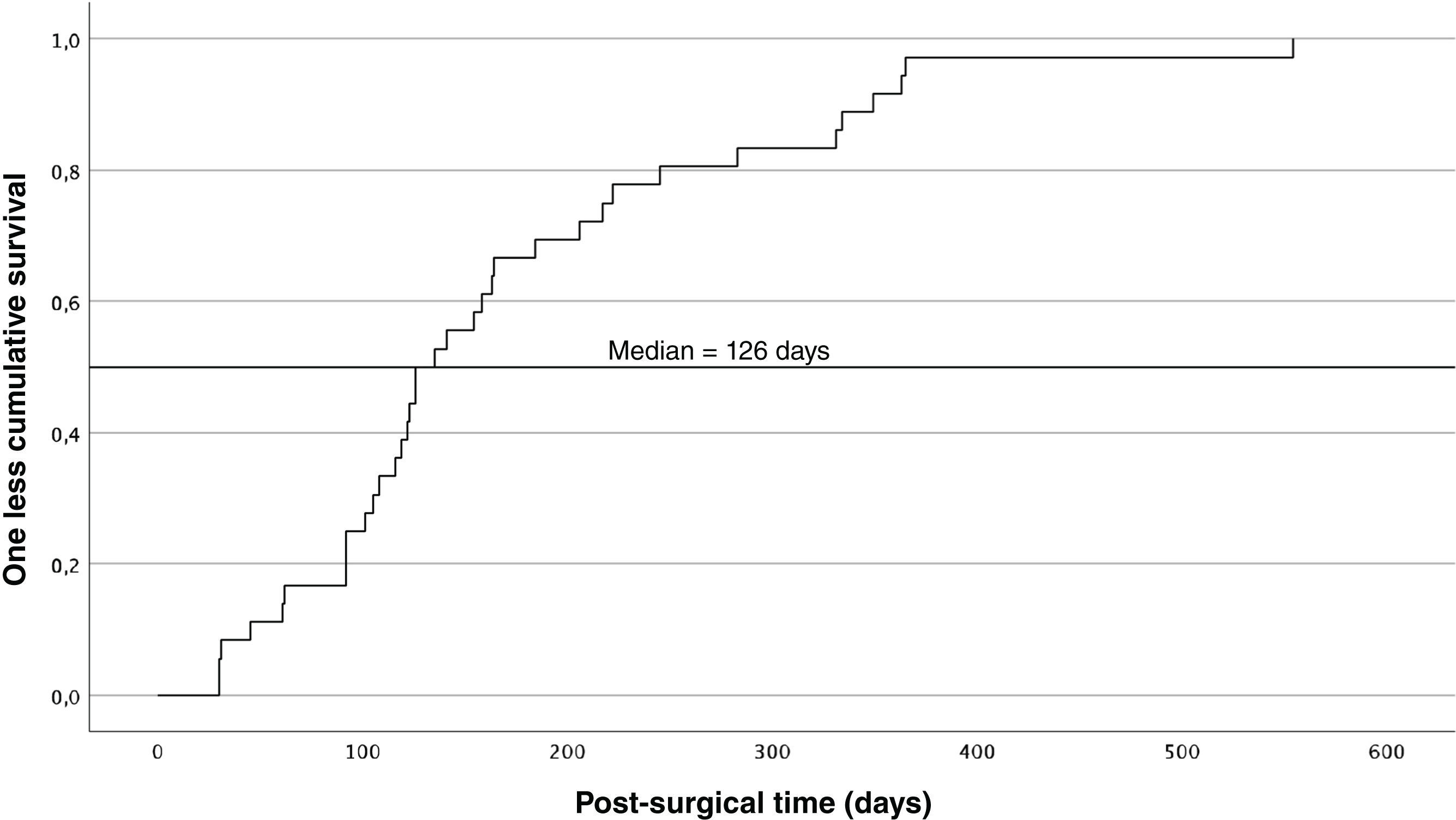
All patients in our study returned to their previous occupation. The median (Q1, Q3) return to work for our patients was 126 days (92, 217). The survival analysis for the time elapsed until returning to work is shown in Fig. 2.
As can be seen, 75% of patients returned to work before 217 days.
Women spent an average of 4.7 (P25; P75: 3.6; 8.2) months on TOD and men 3.5 (1;5.5), with no significant differences found between them (p=.105).
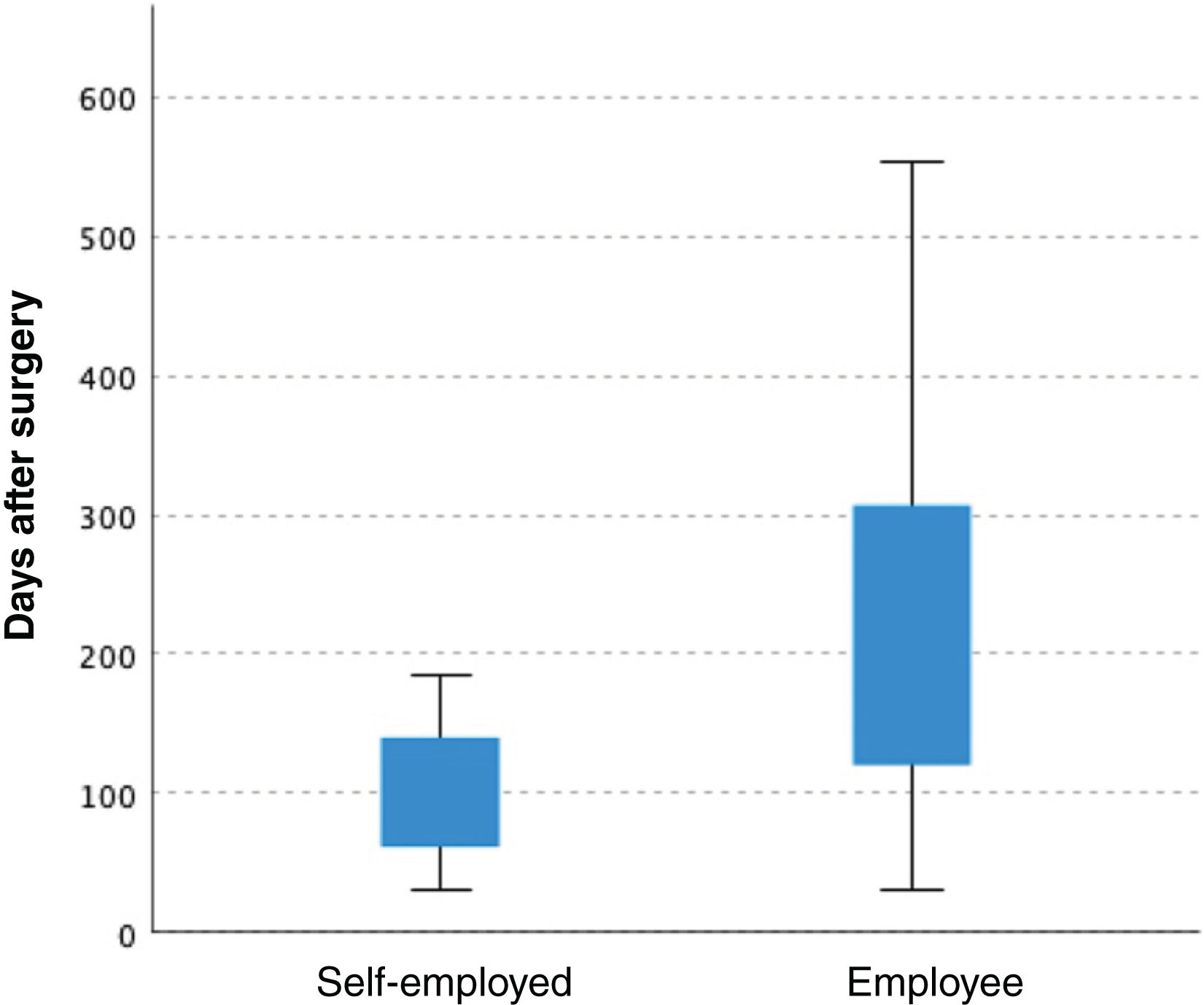
Employees or self-employedEmployed workers, on average, returned to work 164 days after surgery (P25; P75: 120; 319); the self-employed returned to work after 92 days (P25; P75: 62; 147). The difference was statistically significant (p=.004; Fig. 3).
The employed workers, on average, spent a total of 234 days on TOD, including the TOD period prior to surgery (P25; P75: 120; 365); the self-employed, on average, spent a total of 92 days, and all of them started TOD after surgery (P25; P75: 62;147). The difference was statistically significant (p=.003).
Dominant handPatients who underwent surgery on their dominant hand were on TOD for 4.9 months (P25; P75: 3.46; 7.05) and patients whose operated hand was not the dominant one for 4.13 months (P25; P75: 3.21; 7.31), with no significant differences between them (p=.774).
Radiological degree of osteoarthritisThere were no significant differences (p=.787) using the Kruskal–Wallis test, between the operated patients according to their grade in the Eaton–Lambert classification: we found an average TOD of 4.7 months (P25; P75: 2.07; 7.23) in patients with grade 2, an average TOD of 4.15 months (P25; P75: 3.22; 7.13) in those with grade 3 and an average of 5.27 months in grade 4 (P25; P75: 3.5; 7.32).
Biomechanical loadingPatients with grade 2 biomechanical loading work returned to work at 3.85 months (P25; P75: 2.25; 8.15); the return-to-work time was 4.7 months in those with a grade 3 job (P25; P75: 3.37; 7.4). The only patient with a grade 4 returned to work 1.03 months after surgery. The differences were not significant (p=.276 by Kruskal–Wallis test).
Complications19.4% of patients presented postoperative complications, without a significant association with a longer postsurgical TOD time. Of the 7 patients who presented complications, 6 required removal of the suspension system due to irritation and pain in the area of the material, occurring 320 days after surgery in its median. Another patient presented with complex regional pain syndrome, which resolved after 10 months.
Patients with complications had a satisfaction average of 7.43 out of 10, while those who did not have complications had a satisfaction average of 9.24 out of 10.
Patients with TOD prior to surgeryPatients who were on TOD leave prior to surgery returned to work after 214 days (P25; P75: 154; 255); those who were not on TOD leave prior to surgery returned to work after 123 days (P25; P75: 92; 193), with this difference being significant (p<.001).
DiscussionDisability, both temporary and permanent, is an indicator of health outcomes, health management, health effectiveness and is an indicator of public health. It is also an indicator of occupational health and a clear indicator of quality of life.10
Time until reincorporationIn our study we observed that the median for RW was 126 days, with an average of 4.7 months and 3.5 months in women and men, respectively, without this difference being significant. Wolf et al. reviewed the Swedish Employment Registry and compared the TD time in TMC prosthesis versus those operated with trapeziectomy and tendon interposition, with postoperative TD time being significantly shorter in patients with TMC prosthesis. However, they found no differences in the duration of TD between sexes or correlation with age.11
In the study by Van der Oest et al., on patients who underwent trapeziectomy and tendon interposition, the median time to return to work was 12 weeks.12
In a study comparing a total of 21 patients with trapeziectomy and ligamentoplasty with or without tendon interposition, Kriegs et al. found that 15 patients returned to work (71.4%), 5 did not do so due to retirement (23.8%) and only one (0.05%) did not return to their previous job due to persistence of pain.13
In Spain, Paredero et al., in their study on patients with TMC arthrodesis, report that 15 of 16 arthrodeses return to their work activity, 6 of them with some limitation, without specifying the time for RW.5
The study sample, the parameters evaluated, as well as the definition of return to work make it difficult to compare our results with those of other studies. In the study by Hohendorff et al.,14 the “occupational disability” time was established when the patient returned to work 50%. In this study, 90% of the patients (n=47) who underwent resection arthroplasty and FCR interposition, returned to work, 50%, after an 8-week TD period; at 16 weeks the patients returned to work 100%. We would cautiously suggest that our results did not show different recovery times.11
The employment situation significantly influences the days for RW according to our study. Patients who work as self-employed have shorter times for RW (72 days less on average) and total TOD time (142 days less on average) compared to those who work as employees. This conclusion should be viewed with caution since we believe our simple was small and for future studies the difference should be made through subgroups by type or workload, or other means.
Operating on the dominant side, age, sex and radiological grade prior to surgery did not affect the times for RW according to our study, as described in other studies.11,15,16
Unlike other studies, we did not find differences in the days until RW according to the level of manual biomechanical work loading.12,14 In the study by Van der Oest et al. TD time is longer in patients with heavy work compared to those with light work.12 It is not easy to make comparisons since there is great variability when establishing the definition or classification of professions, and even more so when they are different countries. In our case we chose to classify patients based on their biomechanical work loading. For manual biomechanical loading, the requirements of the joints are assessed by postures maintained over time (isometric type) or by repetitive stress on the joint by dynamic movements and 4° are established: low intensity, moderate, medium–high or very high intensity. The majority of our patients had grade 3, making comparisons between subgroups within our study difficult. Moreover, there are other criteria such as load handling and precision work that were not taken into account in our study but that perhaps should be taken into account in future studies.8
Domestic workers returned to work after 3 months according to the study by Hohendorff et al. Interestingly, workers with light manual activities showed worse results than workers with high-demand activities.8
Patients who undergo surgery while on TOD prior to surgery have periods of total TOD greater than those who began their TOD on the day of surgery, with this being statistically significant. The latter has an important socio-economic implication: patients, their company and Social Security could benefit if the surgical waiting list is shortened for patients who are already on TOD prior to it. This difference is 91 days on average according to our study.
Assessing TOD should take into account that this variable is impacted by both medical-surgical factors, and also the patient's socio-work environment. In this environment there are both individual and non-individual factors. The individual ones relate to the employee and their job and interfere with returning to work. Non-individual factors remain separate from the employee and their job. They are transversal and are linked to the process of getting sick. In contrast, they are due to territorial variability, management variability, regulations and economic variability. The factors inherent to work may be summarised as follows10,12,17–19:
- 1.
Occupational variability due to the diversity of professions and their tasks, the employment sector, labour conditions and their specific requirements.
- 2.
Variability due to type of contract and type of company.
- 3.
Psychosocial variability of each patient due to their family, social and occupational settings, and their expectations regarding returning to their previous occupation.
This study has with several weaknesses. First of all, it is a retrospective and observational study. We do not have rating scales or objective measurements of pre- and post-surgical strength and precision to evaluate the relationship between the measured results and TOD time. Meticulous objective measurements could help when establishing returning to work criteria. Furthermore, evaluating the functional requirements according to biomechanical loading may be insufficient to classify the professions evaluated in our study into groups: it is true that there are 4 grades, but a review of the professional guide reveals that many of the professions are grade 3. Also, trapeziectomy and suspension (or with ligamentoplasty and interposition) is a surgery that per se is usually reserved for patients with lower demand. Therefore, being able to further stratify professions according to their requirements could help classify more groups and thus provide more groups to compare. When we studied the differences between self-employed people and employees, although the biomechanical requirements were similar in both groups, there may have been other co-factors that impacted the results. In our study we did not take into account the psychosocial aspect of each patient, which could be assessed in future studies. Finally, a larger sample would help to evaluate the influence that different post-surgical complications have on return to work. In our study, 7 patients presented some complication: 6 of them had intolerance to the suspension system that required its removal, almost a year after surgery (median: 320 days). Complications decreased our patients’ satisfaction from 9.24 to 7.43 on average, but we found no significant differences for their return to work. In our study, the TOD time after extraction was not taken into account due to intolerance to the suspension material, so this aspect should be assessed in future studies.
ConclusionsThe assessment of a TOD requires a multifactorial study due to its complexity. Working as an employee and/or being on TOD leave prior to surgery implies a greater total TOD time. New studies with a greater number of patients are required, along with assessment scales and objective measurements, to evaluate risk factors for a longer TOD time.
Level of evidenceLevel of evidence ii.
FundingThis research received no specific funding from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.