Anterior glenohumeral bone loss reconstruction reduces failure rates after soft tissue surgery in patients with large glenoid bone defects. Multiple bone block techniques have been described, most with metal hardware fixation. The objective of this study is to evaluate the safety, as well as the short term functional and radiological results of an arthroscopic bone block metal-free fixation or Bone Block Cerclage (BBC).
Materials and methodsRetrospective study of patients with glenohumeral instability and >15% glenoid bone loss operated during 2019 with follow-up (FU) of at least 12 months. Radiography and computed tomography (CT) studies were performed. Functional outcomes were evaluated before and after surgery with the Western Ontario Shoulder Instability Index (WOSI) and Rowe score.
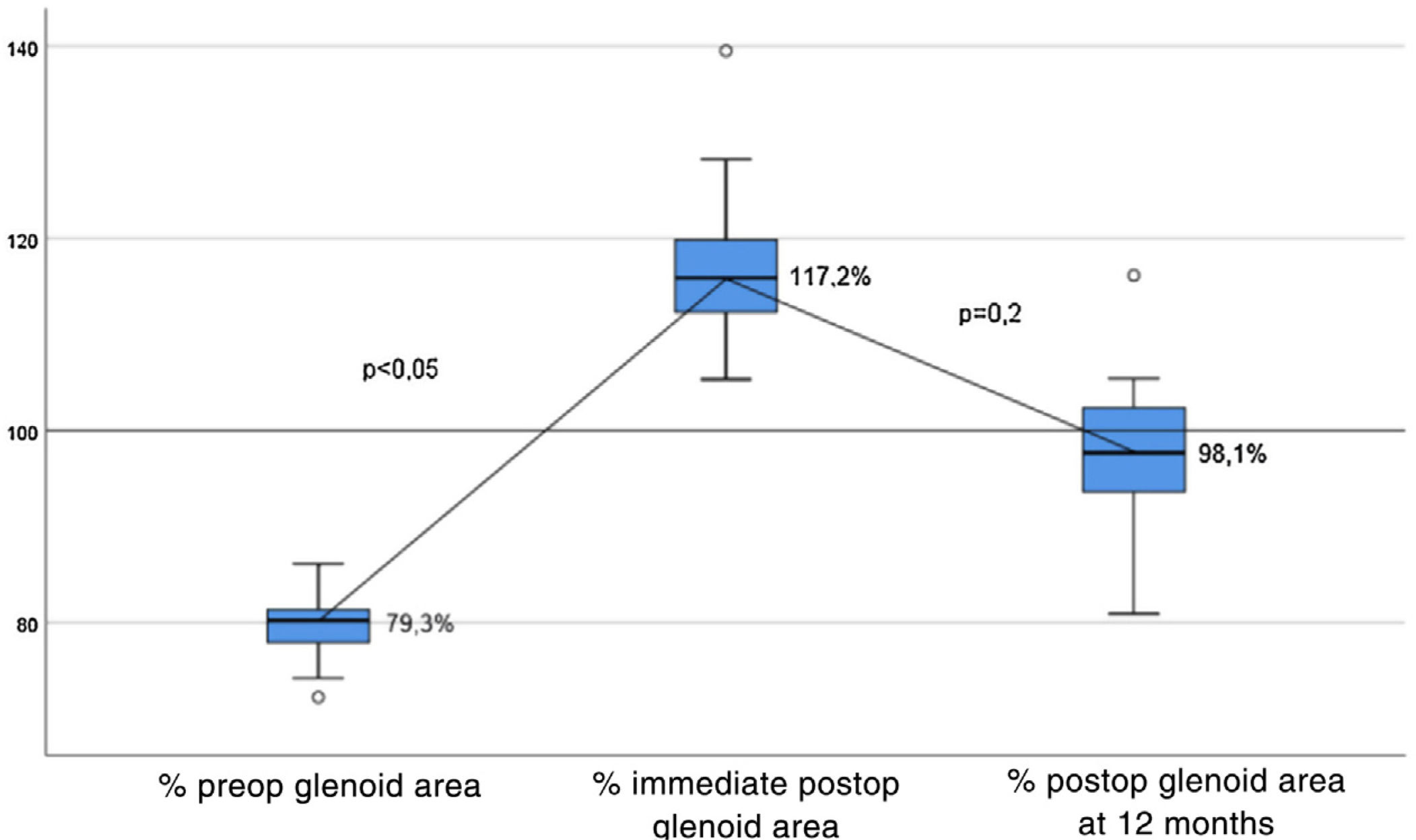
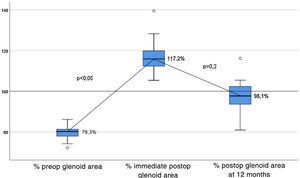
ResultsA total of 21 patients with a median age of 30.6 (SD-7.1) were included. All showed radiographic consolidation at 3 months FU. 90.4% of bone grafts presented osteolysis at peripherical areas and 95.2% revealed consolidation in the areas with contact to the glenoid. The median glenoid estimated surface went from 79.3% before surgery to 98.4% at 12 months. Functional scores were statistically significant (p<0.001) for WOSI (35.6–86.9) and Rowe Score (25.2–96.4). No serious complications were reported.
ConclusionsThe Bone Block Cerclage (BBC) is a safe, metal-free technique that achieves total consolidation of the bone graft and favourable functional and radiological outcomes at 12 months FU. Further studies with a larger number of patients and follow-up time are needed.
Existen múltiples técnicas para la reconstrucción del defecto óseo glenoideo con bloque óseo en la inestabilidad glenohumeral anterior, que reducen el riesgo de recidiva tras cirugía de partes blandas, la mayoría utilizando fijación metálica. El objetivo de este estudio es evaluar la seguridad quirúrgica, los resultados funcionales y radiológicos a corto plazo de los pacientes sometidos a una técnica artroscópica con bloque óseo y fijación sin metal o Bone Block Cerclage (BBC).
Material y métodosEstudio retrospectivo de pacientes con inestabilidad y defecto óseo glenoideo >15% con 12 meses de seguimiento mínimo. Se sometieron a estudio radiográfico y tomografía axial computarizada (TAC). Se cumplimentaron escalas funcionales de manera pre y postoperatoria: Western Ontario Shoulder Instability Index (WOSI) y la escala de Rowe.
ResultadosSe incluyeron un total de 21 pacientes con edad media de 30,6 (DE: 7,1). Todos mostraron consolidación radiográfica a los 3 meses. El 90,4% de los injertos presentó osteólisis en las áreas más periféricas y el 95,2% presentó consolidación en las áreas de contacto con la glenoides. La media del área de superficie de la glenoides pasó de 79,3% preoperatorio al 98,4% a 12 meses. Los resultados funcionales medios resultaron estadísticamente significativos (p<0,001), tanto para el índice WOSI (de 35,6 a 86,9) como para la escala de Rowe (de 25,2 a 96,4). No se presentaron complicaciones graves.
ConclusiónLa técnica BBC es una técnica de fijación segura, sin componentes metálicos. Consigue una consolidación completa del injerto con buenos resultados funcionales y radiográficos a los 12 meses.
Shoulder instability is very common in young adults, and is particularly important in athletes who compete in contact sports.
There is considerable incidence of glenoid and humeral bone defect in recurrent anterior shoulder dislocation. The prevalence of glenoid bone injury varies according to the degree of glenoid involvement, but is described in up to 90% of dislocation cases and is intrinsically related to the total number of dislocations and the age at which it first occurs.1,2 The prevalence of a Hill-Sachs lesion in recurrent dislocation varies from 84% to 93%.3 Bipolar injury, i.e., glenoid bone injury associated with a concomitant Hill-Sachs lesion, is found in up to 81% of cases.4
Anterior glenoid or Hill-Sachs glenoid bone lesions on the posterior aspect of the humeral head are determining risk factors in recurrent glenohumeral instability. The loss of glenoid bone support leads to an insufficient concavity-compression effect that affects the main static stabilizers of the glenohumeral joint.5
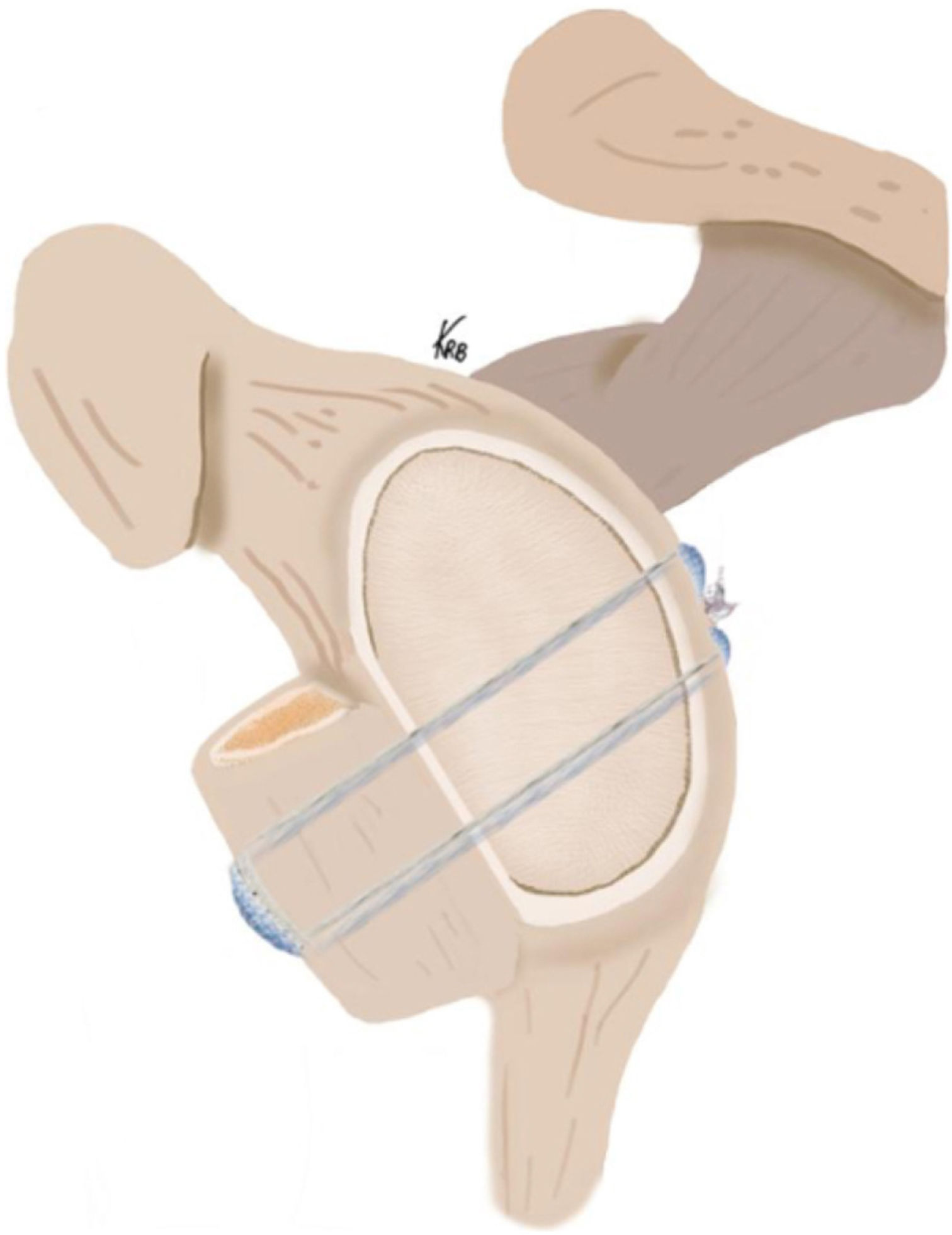
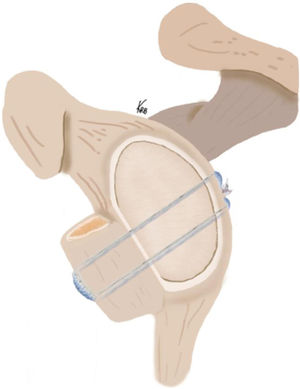
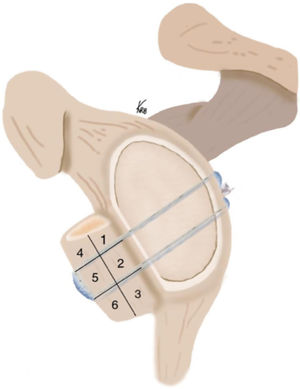
Confronted with the problem of bone lesions in anterior glenohumeral instability, an arthroscopic technique with anatomical reconstruction of the glenoid using tricortical iliac crest auto or allograft was used to treat these lesions. Considering the significant rate of complications associated with metal implants in bone reconstruction techniques,6 the aim of this study is to present the surgical safety and results of the bone block cerclage (BBC) technique,7 which uses mechanical compression fixation with high-strength tape cerclage sutures (Tape Cerclage Sutures, Arthrex, Naples, FL, USA) (Fig. 1).
Drawing of the bone block cerclage technique for reconstructing the bone defect in anterior shoulder instability with iliac crest bone graft fixed with high strength metal-free tapes passed through 2 glenoid tunnels from posterior to anterior and through the graft. The interconnection of the tapes at the posterior glenoid, combined with the use of a mechanical tensioner, achieves a strong fixation in the same plane as the native glenoid cartilage to reconstruct the bony defect in anterior shoulder instability.
A retrospective observational study was conducted to identify and assess all patients diagnosed with anterior shoulder instability in whom computed tomography (CT) measurement determined a bone defect greater than 15%, and treated using the BBC technique during 2019, with a minimum of 12 month postoperative follow-up.
This study was evaluated by the Research Ethics Committee of the Hospital Universitari de Bellvitge. Informed consent was waived for the use of the data given the observational and retrospective nature of the study. Data processing complied with current legal regulations.
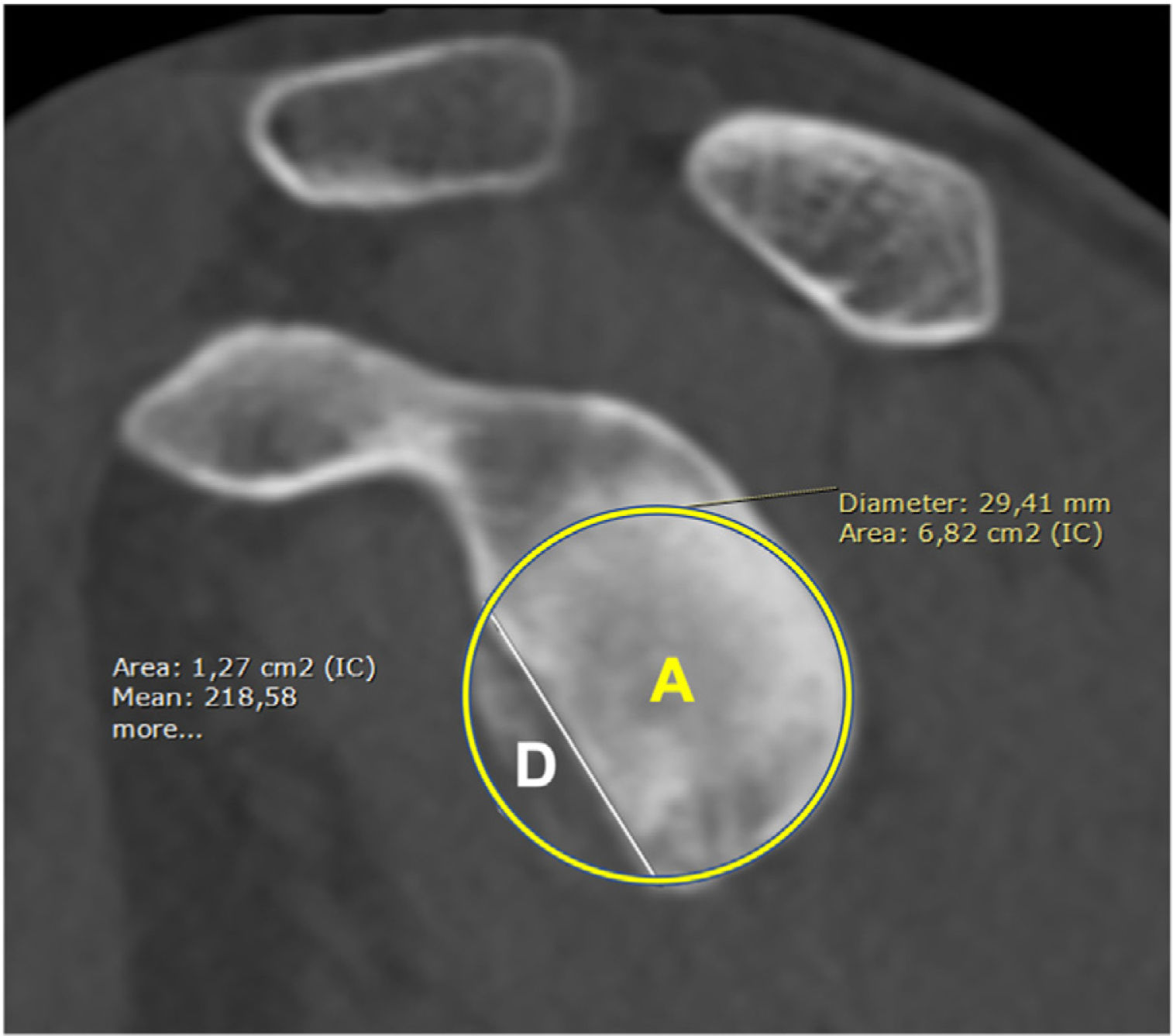
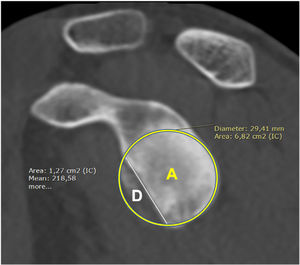
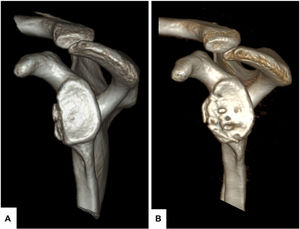
Bone defect measurementAll patients underwent a 2D CT scan of the affected side and the glenoid defect was assessed in the sagittal section immediately medial to the humeral head. The best-fit circle was then drawn, passing through the 2 points furthest from the posterior and inferior border of the glenoid, to obtain the normal area of the glenoid in cm2. The defect area was then measured using the computer programme's measurement tools and calculated as a percentage of the total best-fit circle area using the formula D/A×100 (where D is the defect area and A is the best-fit circle area) according to Sugaya et al.1 (Fig. 2). Reconstruction surgery with tricortical iliac crest bone graft was indicated in all patients who had a defect greater than or equal to 15% of the circle area, which corresponds to about 4–6mm of its diameter. The choice of graft, either autogenous or allogeneic, was as preferred by the patient, after informing them of the risks and benefits of each.
CT-2D image of a shoulder with anterior instability with bone defect. Sagittal view immediately medial to the humeral head with the best-fit circle passing through the 2 points tangential to the most posterior and inferior border of the glenoid. (A) Normal glenoid area in cm2; (D) area of the defect; and calculation in percentage of the total area of the best-fit circle using the formula D/A×100, according to Sugaya et al.1
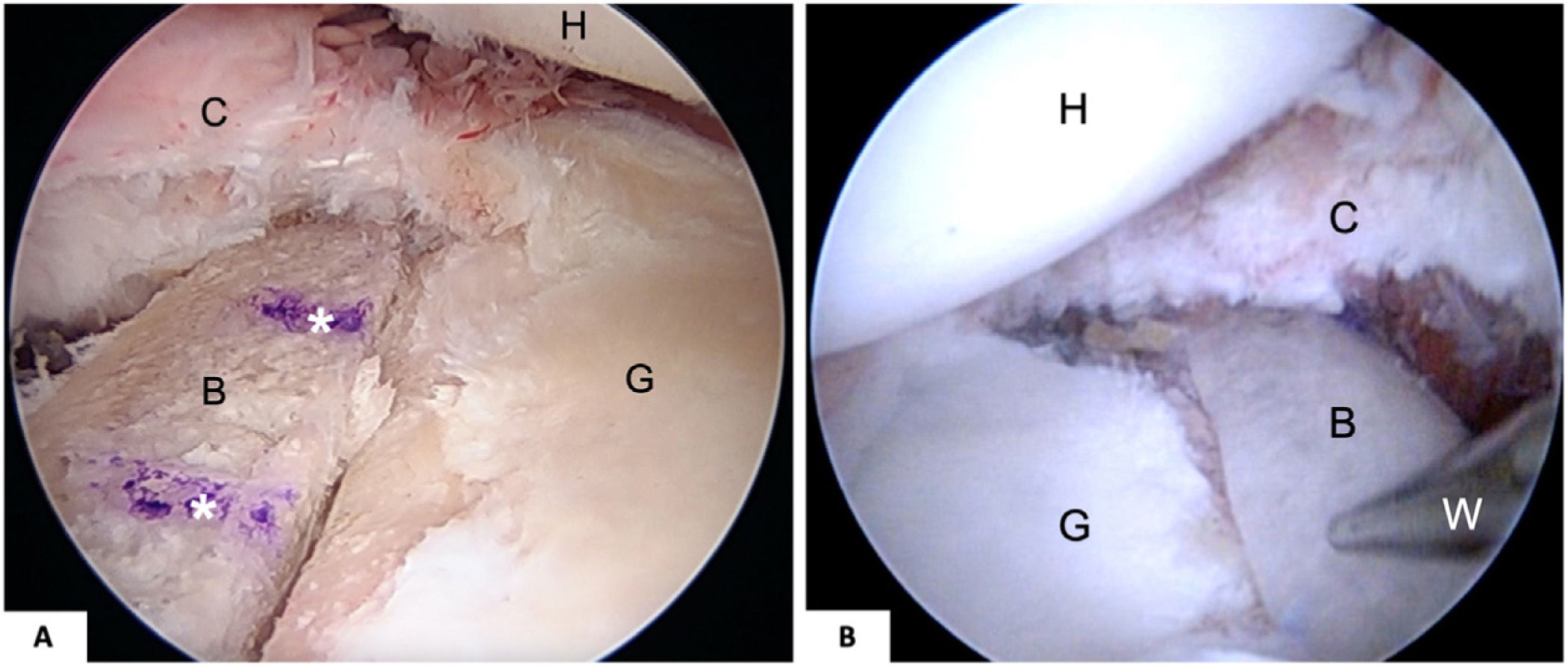
The patient is placed in a lateral decubitus position with standard posterior and anterior arthroscopic portals, with an anterosuperolateral portal over the long potion of the biceps. After identifying the glenohumeral bony lesion, the anterior glenoid rim is prepared by releasing and tractioning the capsulolabral complex in a “tent-pole” fashion.8 Using a special millimetre gauge, the anterior border of the glenoid corresponding to the defect is measured from cranial to caudal. From the posterior portal, the pointed hook of the drill guide is placed in the centre of the previously measured distance to adapt the iliac bone graft to the glenoid in the coronal and transverse planes. Through an accessory portal, 2cm medial to the standard posterior portal, the glenoid drill guide is placed and attached to the hook placed in the first arthroscopic posterior portal. With this guide fixed from posterior, and with arthroscopic visualisation from the anterosuperolateral portal, the glenoid is drilled with 2 parallel tunnels from posterior to anterior using 2 cannulated 2.4mm drills exiting cranial and caudal to the hook, in the central area of the defect. This allows the simmultaneous passage of 2 preconfigured Fibertape and TigerTape Cerclage systems (Arhtrex, Naples, FL, USA), each system consisting of 2 high-strength braided tapes, thus having 4 tapes per glenoid tunnel. These tapes enter from the posterior side of the glenoid, passing through one of the tunnels, and are retrieved through the anterior rotator interval to pass back and forth through the bone graft, which typically measures 25/30×10×10mm, drilled according to the measurements made previously. The holes of the graft are adapted to the distance of the exit of the glenoid tunnels, so that it fits in marquetry and the graft sits in the anterior centre of the defect between 2 and 6 o’clock describing the glenoid as a clock. The aim is to place the graft flat to the anterior cartilage of the glenoid, adjusting it as much as possible to the defect area (Fig. 3). The tapes are then returned posteriorly through the second tunnel. The tapes from each tunnel are interconnected with each other, and initial manual traction is performed. With the use of a mechanical tensioner, the tension in the tapes is sequentially and progressively increased, to reduce the risk of fracture of the graft, until compression of approximately 80 pounds (approximately 350N) is achieved, ensuring absolute stability of the bone graft (Fig. 1). Finally, a biological repair of the capsulolabral complex is performed on the anterior edge of the native glenoid, previously debrided with a curette, all with 1.8mm knotless suture implants (Arthrex, Naples, FL, USA), leaving the bone block in an extra-articular position.
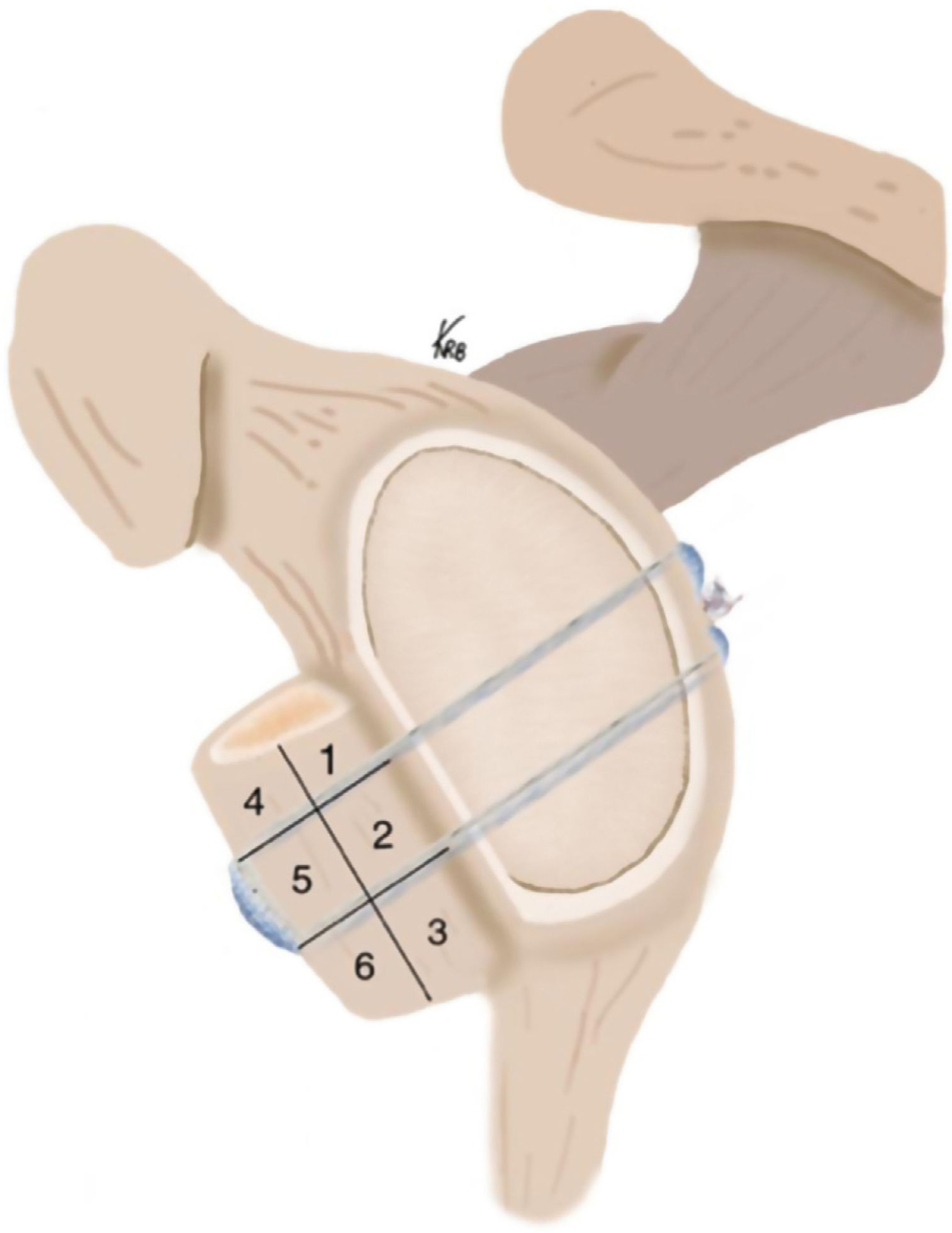
Illustrative drawing of the bone block cerclage technique to reconstruct the bone defect in anterior shoulder instability with the iliac crest graft divided by areas for measurement and analysis by CT. When osteolysis affected more than 50% of one quadrant it was considered positive for osteolysis.
Serial pre- and postoperative anteroposterior radiographs were taken at 1, 3 and 6 weeks, 3, 6 and 12 months. A Bernageau view was taken at 6 weeks, 3, 6 and 12 months. All patients underwent postoperative CT to assess the anterior bone block consolidation and remodelling before 6 weeks and at 12 months. On a sagittal section of the 2D CT at the height of the glenoid, 6 areas were established at the level of the graft, numbered from 1 to 6 so that 3 areas are in contact with the glenoid and the other 3 are more distant, without contact (Fig. 4). Based on this division, the consolidation of the areas in contact with the glenoid was studied, as well as the osteolysis of all areas over time. In the comparison between the CT scan performed before 6 weeks and at 12 months, the areas affected by more than 50% bone resorption were rated as positive osteolysis (+) and those with less than 50% rated as negative.
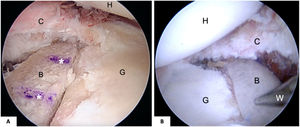
(A) Right shoulder, lateral decubitus, arthroscopic view from the anterosuperolateral portal, showing placement of the bone block on the anterior border of the glenoid at the level of the glenoid cartilage. The asterisks indicate the path of the tunnels. (B) Left shoulder, lateral decubitus, arthroscopic view from the anterosuperolateral portal, showing the stability of the bone block fixation. B: bone block; C: capsulolabral complex; G: glenoid; H: humerus; W: Wissinger rod.
The patients were assessed functionally using the Western Ontario Shoulder Instability Index (WOSI) adapted to Spanish and the Rowe scale, preoperatively and postoperatively at 6 and 12 months. IBM® SPSS® version 25 was used for the statistical analysis. The Shapiro–Wilk test was used to check for the normal distribution of the variables. Descriptive data of the variables were obtained and compared using the Student's t-test, the Wilcoxon test and the χ2 test or Fisher's exact test.
ResultsTwenty-three patients were treated with the described technique; one did not have the minimum follow-up, and another was lost during follow-up, leaving a total of 21 patients (91%) who met the inclusion criteria. The gender distribution was 20 men and one woman, and the mean age of the sample was 30.6±7.1 years. The mean±SD and median [range] preoperative bone defect measured in the total series were 20.7±3.6 and 19.8 [15; 27.8], respectively.
In terms of the type of graft used, iliac crest allograft from the bone bank was used in 14 patients and iliac crest autograft was used in 7 patients obtained during the surgical procedure from the side of the affected shoulder, as preferred by the patient. Radiographic assessment at 3 months postoperatively using a Bernageau view showed apparent consolidation of the graft in all but one case, which was classified as delayed consolidation.
The comparative study between CT scans performed before 6 weeks and at 12 months, according to the segmental division of the graft, revealed a mean of 32.5% of graft areas affected by osteolysis in the whole series. The osteolysis by graft area is detailed in Table 1. Of the grafts, 90.5% showed some type of osteolysis at 12 months in the whole series, corresponding generally to the most peripheral or distant areas, those numbered 4 and 6, at the cranial and caudal ends of the graft. Areas 1, 2 and 3 from cranial to caudal in contact with the glenoid consolidated in 95.2% of the patients (Fig. 4).
Results of the statistical analysis of osteolysis in the 6 areas of graft division of all patients assessed on CT at 12 months.
| Total number of positive areas per graft (N=21) | n (%) |
|---|---|
| 0 | 3 (14.3) |
| 1 | 4 (19.0) |
| 2 | 8 (38.1) |
| 3 | 5 (23.8) |
| 4 | 0 (.0) |
| 5 | 0 (.0) |
| 6 | 1 (4.8) |
The corresponding number and percentage of the total number of cases is shown in relation to the number of areas with osteolysis. The highest percentage corresponds to two areas, which were the most peripheral called 4 and 6 in Fig. 4.
Osteolysis or almost complete resorption of the graft was observed in the case that had been previously classified as delayed consolidation, with involvement of all 6 zones, corresponding to an allograft of suboptimal quality in terms of the tricortical thickness of the iliac bone, which was 7mm and which presented clear fragility of the bone trabeculae. This case was the only osteolysis found in the contact areas between the graft and the glenoid (zones 1, 2 and 3).
In relation to the percentage of the defect as it relates to the best-fit circle, and with the addition that the graft represents with respect to the native glenoid according to the CT measurement, a postoperative variation of 117.2±7.8 on average was observed with respect to the preoperative percentage of 79.3±.8, which at 12 months is set at 98.1±7.1, and significant differences were found between the preoperative and immediate postoperative results (p<.05), but not so between these and the 12-month results (p=.2). As measured on CT, the global remodelling of the graft at the expense of the peripheral areas makes the final postoperative glenoid shape at one year resemble the original size of the best-fit glenoid circle, as it reached 98.1% (Fig. 5). Analysis of the functional scales showed a statistically significant improvement in the preoperative and postoperative comparison, on both the WOSI and the Rowe scale (Table 2).
Variation of the percentage of glenoid area from 100% under normal conditions, measured with CT. The immediate postoperative glenoid area presents a statistically significant oversizing with respect to the preoperative area due to the larger size of the graft placed with respect to the preoperative defect area. It was noted that, at 12 months postoperatively after final bone resorption and remodelling of the peripheral areas without cyclic loading, the final glenoid area was close to 100% of normal, with no statistical significance between immediate postoperative and 12 months.
Global preoperative statistical results of the WOSI and Rowe functional scales preoperatively, at 6 months and at 12 months with the p-value corresponding to the time intervals.
| Functional scale | Preoperative, mean (SD) | 6 months, mean (SD) | 12 months, mean (SD) | p | ||
|---|---|---|---|---|---|---|
| Pre-6m | Pre-12m | 6–12m | ||||
| Total WOSI with total Rowe formula | 35.6 (15.3) | 81.1 (13.9) | 86.9 (10.7) | <.001 | <.001 | <.05 |
| 25.2 (12.2) | 84.7 (23.9) | 96.4 (10.3) | <.001 | <.001 | .116 | |
These are statistically significant when comparing the preoperative condition with the result at 6–12 months, whereas, if we compare the functional tests between months 6 and 12, there is statistical significance only in the WOSI test.
In terms of complications, no intraoperative graft rupture was observed during mechanical compression with the tensioner. There was a superficial infection in one of the portals in one patient, which was resolved with wound dressings. No postoperative haematomas, neurovascular lesions or deep infections were observed. One case had stiffness on external rotation (<15° compared to the contralateral) with the elbow pressed against the body. No episodes of subluxation or dislocation were reported in any case in the series. No posterior glenoid symptoms were found in relation to the position of the drill guide or the tapes’ blocking system. The CT study revealed the correct entry location of the glenoid tunnels near their posterior free edge.
DiscussionThis new metal-free, high-compression fixation system resulted in osteointegration and consolidation of the graft in the areas close to the glenoid in 95.5% of cases, despite finding 32.5% global osteolysis, most of which affected peripheral areas. The excellent functional results obtained, together with the absence of short-term complications, demonstrate the safety and reproducibility of this technique.
Numerous attempts have been made to find the critical defect size that determines, on the one hand, the imperative need to reconstruct the glenoid bone defect and, on the other, the reason soft tissue procedures fail.9 Burkhart and De Beer8 initially described 25% as the “critical” bone lesion for predicting failure of isolated arthroscopic Bankart repair, and this concept was complemented by the biomechanical studies of Itoi et al. who established that the risk of recurrent instability increased significantly in glenoid lesions greater than 20%.10,11 Shaha et al. demonstrated that, in a certain group of patients, functional outcomes based on the WOSI decreased with what they termed “subcritical” lesions above 13.5% of the defect.12 However, Shin et al. found that there was a 42.3% recurrence and/or apprehension rate in arthroscopic Bankart repair with bone lesions greater than 17.3%.13
More recently, Di Giacomo et al.,14 as well as Provencher et al.,9 indicate reconstruction surgery with bone block in defects greater than 15% for patients with certain characteristics and concomitant humeral defect. Yamamoto et al.15 concluded that contact athletes with peripheral on-track Hill-Sachs lesions should be treated as off-track lesions, restoring the glenoid track using a bony reconstruction technique.16
The concept of the critical glenoid bone injury continues to evolve, as it is dependent on multiple variables. It is clear that further comparative studies with larger numbers of patients and prolonged follow-up are still needed to standardise surgical indications, especially in subcritical bone lesions.
Anterior glenoid reconstruction using a tricortical iliac crest graft is used to anatomically restore glenohumeral stability in patients with shoulder instability and significant bone defect. The first descriptions treating anterior shoulder instability with subperiosteal free autograft without fixation were by Eden17 with distal tibial autograft and by Hybinette18 with iliac crest autograft. Since then, this procedure and its modifications have been referred to as “Eden-Hybinette”. De Palma19 modified the technique, fixing the iliac crest graft with a screw in the defect. Tauber et al.20 designed a self-stable implant-free iliac crest graft, giving it a “J” shape (hence the name, J-graft) to treat instability with bony defect, which Anderl et al.21 adapted for a fully arthroscopic technique.
The functional results of the iliac crest graft are promising in published series. In a level 1 clinical trial, Moroder et al.,22 compared 2-year clinical outcomes between iliac crest grafting with J-graft technique and Latarjet for bone defects>15%, and found no statistically significant differences in WOSI, Rowe or Subjective Shoulder Score at any follow-up point. In addition, the Latarjet patients had slightly decreased internal rotation at 90° abduction, greater scapular dyskinesia and less glenoid area covered with the coracoid at 12 and 24 months.
Kraus et al.23 evaluated the results with 20.6 months of follow-up of patients treated using an autogenous iliac crest graft technique, initially described by Scheibel et al.,24 reporting a Constant score of 85, a Rowe score of 88, a Subjective Shoulder Score of 84.5% and a WOSI of 76.7%, with consolidation of the graft in all cases. Boehm et al.25 later assessed the same series at 5 years follow-up, maintaining comparable results in the functional scales, finding recurrence of dislocation in one case (7.1%), secondary to trauma, and one reoperation with capsular plication due to persistent apprehension and sensation of instability. These results are comparable to those obtained in this study.
In relation to the origin of the graft, there are also different published series that emphasise consolidation and osteolysis rates in procedures with autograft or iliac crest allograft. Ernstbrunner et al.26 presented a radiological analysis of the J-shaped autograft, reporting good coverage of the defect with restoration of the glenoid surface and joint congruency. Giannakos et al.27 reported up to 67% good to excellent results in a small series of 12 patients managed with autograft at 28 months follow-up. However, only 7 showed signs of consolidation and one had complete graft resorption.
In contrast, a series published by Zhao et al. showed CT consolidation in 100% of their series using iliac allograft, with a mean osteolysis of 32.3% (range 8–88%) of the graft in the first 12 months, with no progression at 24 months.28 In a recent study with distal tibial allograft fixed with screws, after CT scanning 73% of cases at 6.3 months, Amar et al.29 found complete consolidation and resorption<50% in 42% of cases and >50% in 16% of patients.
After accumulating more than 8 years of experience in the treatment of bone defect associated with instability using biodegradable screws or metal buttons, the BBC technique is now indicated in all patients with recurrent shoulder dislocation and anterior glenoid defect greater than 15% of the best-fit circle area. With the BBC technique, the bone graft is fixed using a mechanical tensioner that leads to high compression of the graft against the anterior glenoid defect area. The bone graft is introduced through the rotator interval while fully respecting the subscapularis tendon and muscle. Any risk of neurovascular injury described in the literature is reduced and avoided by not using fixation screws from an axillary portal that seeks parallelism to the glenoid.30
In this series, consolidation of the iliac crest graft was achieved in all patients, except for one case in which it was partial. Most patients had a defect between 15% and 20%, corresponding to about 4–5mm of the best-fit circle diameter. The iliac crest graft placed is 10mm wider than the defect. At 12 months, 90.5% of the grafts presented some type of osteolysis, most of which affected the areas that exceeded the actual size of the preoperative defect and were the furthest away from the glenoid. However, the areas in full contact with the glenoid did not present osteolysis in 95.2% of the patients, favoured by the biomechanical loads.
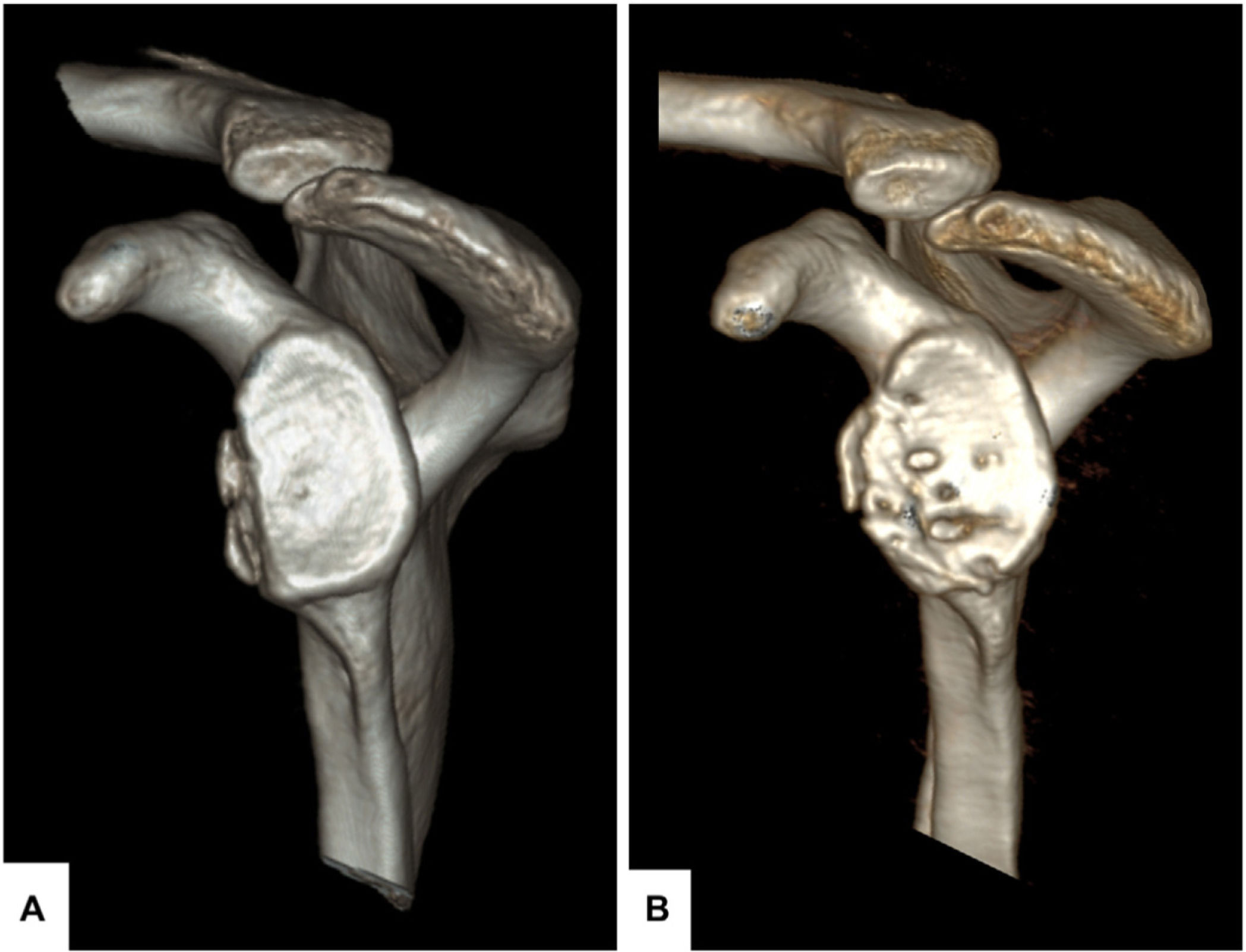
The osteolysis observed affected the areas distal or peripheral to the glenoid, which are the least subjected to cyclic loading due to the oversizing of the graft outside the defect area. This has resulted in global remodelling of the bone graft resulting in coverage of the defect and eventual restoration of the glenoid surface (Fig. 6). Despite these good initial radiographic results, further follow-up is required to assess the rate of bone resorption of the iliac crest graft in the medium term.
(A) En-face 3D CT image with removal of the humeral head of the case presented in Fig. 2 with a defect of approximately 20% of the glenoid area, showing 2 small bone fragments displaced medially with respect to the glenoid surface. (B) Result at 18 months after reconstruction with iliac crest allograft showing how global remodelling, which mainly affects zone 6 in the most inferior part and distal to the glenoid, results in good coverage of the defect with restoration of the glenoid area.
Good functional results were achieved at 12 months on the scales applied using both types of iliac crest graft. There were no serious complications. While the functional results are promising, a larger number of patients and longer follow-up are needed to draw further conclusions on its impact on the management of shoulder instability with bone defect, as well as potential recurrence and possible late osteoarthritic complications.
LimitationsThe indication for surgery did not analyse the humeral defect, as these off-track defects become on-track with the bone block. The lack of assessment of the interobserver difference of the defect is a limitation, although this did not affect the goal of surgical safety. The failure to differentiate between allograft and autograft because they were not numerically balanced may imply a distribution bias. Finally, the short follow-up period limits assessment of long-term complications.
ConclusionsThe BBC technique has been proven to be surgically safe, reliable, effective procedure with good short-term functional and radiological results for the treatment of recurrent anterior glenohumeral instability with glenoid bone defects greater than 15%.
Level of evidenceLevel of evidence iv.
Conflict of interestsDr. Hachem is a consultant to Arthrex and has a patent pending for this fixation system in the USA.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Dr. Karla R. Bascones for her contribution with the illustration of the technique, and Alexander Campagnoli in the development of the metal-free fixation system.