Currently, there is a lack of prospective studies to unify criteria about type and time for postoperative immobilisation in surgical distal radius fractures. The aim of this study is to compare functional and radiological results in two groups of distal radius fractures treated with internal fixation with locking plate, and immobilised with antebrachial splint or compression bandage for 3 weeks.
Material and methodA randomised clinical trial was carried out with two parallel groups with 3, 6, and 12 weeks of follow-up. Main and secondary functional variables were measured, such as pain on VAS scale, values on PRWE, DASH and MRS scale, range of motion in flexion–extension, complications, etc. In addition, some radiological variables were measured at preoperative period and one week after surgery, such as union time, dorsal displacement, shortening, ulnar variance, etc.
ResultsA total of 62 patients were evaluated: 27 immobilised with bandage and 35 with splint. Analysis of the results obtained showed significant differences in both groups for almost all radiological variables from pre to postoperative period, and for all functional variables from 3 to 12 weeks after surgery. No significant differences were found between the two groups for any of the radiological and functional variables evaluated (VAS 3–12 weeks: p=.584; PWRE 3–12 weeks: p=.248; flexion range of motion 3–12 weeks: p=.959; extension range of motion: p=.50; union time: p=.89).
ConclusionsWe do not find clinical or radiological differences between immobilisation with antebrachial splint or compression bandage for distal radius fractures operated with locking plate. A greater number of patients and follow-up are necessary to extrapolate the results to the general population and to establish criteria for good postoperative management of these fractures.
Actualmente, faltan estudios prospectivos que permitan unificar criterios sobre el tipo y el tiempo de inmovilización posoperatorio en fracturas de radio distal intervenidas. El objetivo del trabajo es comparar los resultados funcionales y radiológicos en dos grupos de este tipo de fracturas de radio distal mediante osteosíntesis con placa, e inmovilizadas con férula antebraquial o con vendaje compresivo durante tres semanas.
Material y métodoSe realizó un ensayo clínico aleatorizado con dos grupos paralelos con un seguimiento a las tres, seis y 12 semanas posoperatorias donde se midieron variables funcionales principales y secundarias, como dolor en escala visual analógica (EVA), valores en evaluación de la muñeca según el paciente (PRWE), discapacidad de brazo, hombro y mano (DASH) y escala de muñeca de la Clínica Mayo (MRS), rango de movilidad en flexión-extensión, complicaciones, etc., además de algunas variables radiológicas en el preoperatorio y a las tres semanas de la intervención, como el tiempo de consolidación, el desplazamiento dorsal, el acortamiento, la varianza cubital, etc.
ResultadosSe evaluaron un total de 62 pacientes: 27 inmovilizados con vendaje y 35 con férula. El análisis de los resultados mostró diferencias significativas en ambos grupos de tratamiento para casi todas las variables radiológicas del pre al posoperatorio y todas las funcionales de la tres a las 12 semanas. No se obtuvieron diferencias relevantes entre los dos grupos para ninguna de las inconstantes radiológicas y funcionales evaluadas (EVA tres a 12 semanas: p=0,584; PWRE tres a 12 semanas: p=0,248; rango de movilidad en flexión tres a 12 semanas: p=0,959; rango de movilidad en extensión: p=0,50; tiempo de consolidación: p=0,89).
ConclusionesNo encontramos diferencias clínicas o radiológicas entre la inmovilización con férula antebraquial o con vendaje compresivo para fracturas de radio distal intervenidas mediante osteosíntesis con placa. Son necesarios un mayor número de pacientes, así como un incremento en el seguimiento para poder extrapolar los resultados a la población y establecer criterios para el buen manejo posoperatorio de estas fracturas.
Distal radius fractures (DRFs) are the most frequent upper limb fractures, with an incidence of about 62 cases/100,000/year in our country. They are among the most frequent trauma emergencies in hospitals and entail major economic and occupational repercussions from the functional incapacity they cause. The incidence of DRF is expected to increase by 50% by 2030 due to the increase in life expectancy in industrialised countries.1,2
The most common surgical treatment for DRF is volar locking plate fixation, and the most common postoperative treatment is immobilisation with a splint or cast for a variable length of time. Numerous studies on non-surgical and/or non-displaced fractures have shown that immobilisation no longer than 3–4 weeks improves the functional recovery and strength of the injured limb with respect to prolonged immobilisation.1
However, there is currently no consensus on the optimal time to start mobilisation in intervened fractures, although it has been shown that early mobilisation helps to reduce oedema and prevent adhesions, stiffness, and muscle atrophy, improving pain and functional disability in the first weeks of treatment.3 However, a 2011 guideline from the American Academy of Orthopaedic Surgery (AAOS) states that patients should not necessarily start an early mobility programme after surgery. This guideline does not suggest any specific protocol based on functional and radiological criteria.4
There are currently few prospective studies that analyse immobilisation time and initiation of mobility in groups of DRF patients who have undergone surgery. There is a lack of homogeneous studies to unify criteria and recommendations. Few studies compare groups of patients with different types of immobilisation. Rigid splints could be replaced by an elastic compression bandage in the immediate postoperative period, allowing controlled assisted active mobility until a specific rehabilitation protocol is initiated.
The aim of the study is to compare functional and radiological results, and to evaluate potential complications in two groups of DRF undergoing open reduction and volar plate fixation: one group treated by immobilisation with compression bandage for 3 weeks, and the other treated by immobilisation with antebrachial plaster splint for 3 weeks. The following hypothesis was established: the group treated with compression bandage achieves equal or better short-term results, and none of the treatments is superior to the other at 3 or 6 months, from the literature reviewed.5–8
Material and methodDesignWe conducted a prospective, longitudinal, randomised clinical trial with two parallel groups of non-inferiority in terms of allocation ratio. The trial was conducted at Clinica de la Mano de Buenos Aires (CLIMBA), Hospital Universitario Costa del Sol, Malaga, Spain, and Hospital Santa Ana, Motril, Granada, Spain. The study was approved by the Costa del Sol Research Ethics Committee with a favourable opinion and a high level of evaluation. Patients were recruited from June 2021 to December 2022 and the trial ended in March 2023.
ParticipantsTo conduct the study, patients with DRF and candidates for surgical treatment by volar plate osteosynthesis, attended both in the emergency department and in the outpatient traumatology department of the hospitals involved, were selected. Patients with AO classification type A, B, C fractures,9 aged between 18 and 75 years, who underwent surgery in the first 3 weeks after the trauma, and independent in basic activities for daily living (BADL) were included in the trial. Patients with open fractures, patients with mental disorders (dementia, alcoholism, etc.), BADL dependent patients, fractures with great articular and metaphyseal comminution and/or great soft tissue distress (AO type 2R3C3), and patients with previous diseases or anatomical abnormalities in the injured wrist (previous DRF, rheumatoid arthritis, etc.) were excluded from the study. For each participant, data were collected on age, sex, comorbidities, dominant hand, type of work activity, time from injury to surgery, and type of fracture according to the AO classification presented.
Patient distributionAfter the corresponding surgery, consisting of open reduction and internal fixation with anatomical locking distal radius plate, the patients were distributed into two homogeneous groups (A and B). Patients in group A received immobilisation treatment with compression bandage (lined gauze bandage reinforced with cohesive elastic bandage, changed after the first and second postoperative week) for 3 full weeks, allowing immediate assisted passive mobility. Subjects in group B received immobilisation treatment by antebrachial splint (plaster of Paris type bandage, padded with lined gauze bandage changed after the first and second postoperative week) for 3 full weeks.
The two interventions were assigned by a simple randomisation method following the order of a random number table generated by an expert practitioner external to the study. The principal investigators included or excluded each patient evaluated in the study. To implement the randomised allocation sequence, another practitioner not collaborating in the study in each hospital controlled the randomisation order of the table and concealed it from the investigators until the time of allocation, which was undertaken by telephone at the end of each surgery. The inclusion of each patient and the treatment allocated were recorded at the end of the procedure on a database shared by all the principal investigators to respect the randomisation between the different centres and the consecutive inclusion of patients. All the treatments used were given after obtaining informed consent in which the different possible treatment alternatives were explained to the patient and the allocation sequence was concealed from the patient. During follow-up it was not possible for masking to be maintained for the participants and the principal investigators, but allocation concealment was respected for the professional evaluating the results of the study.
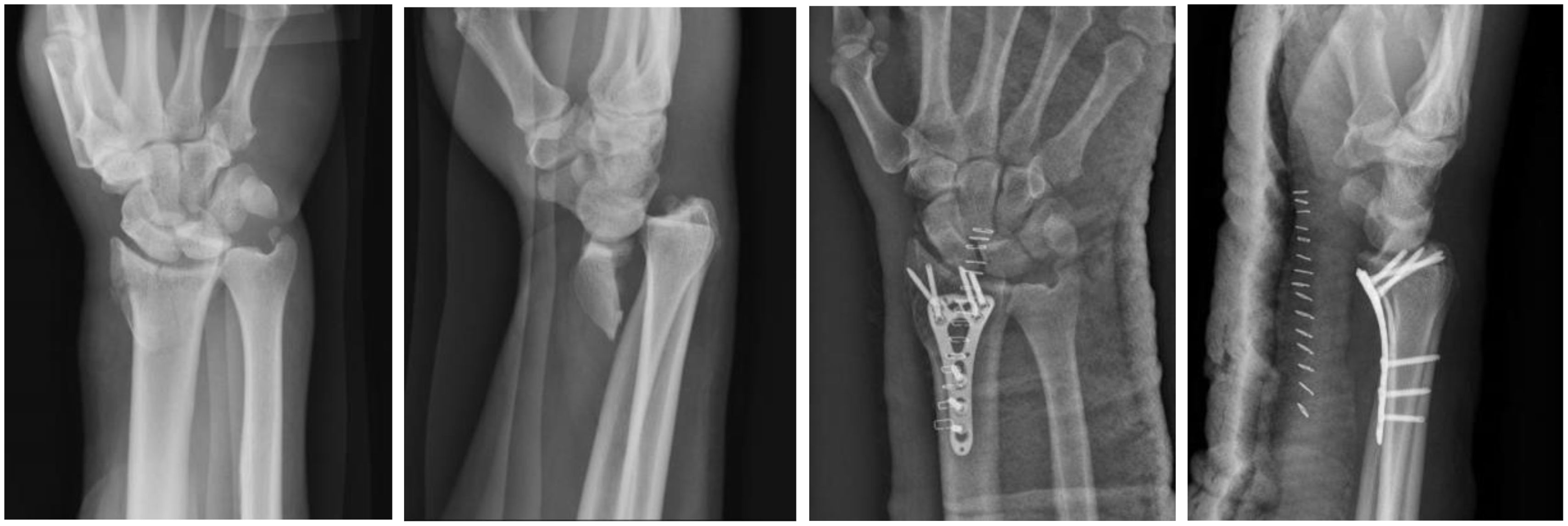
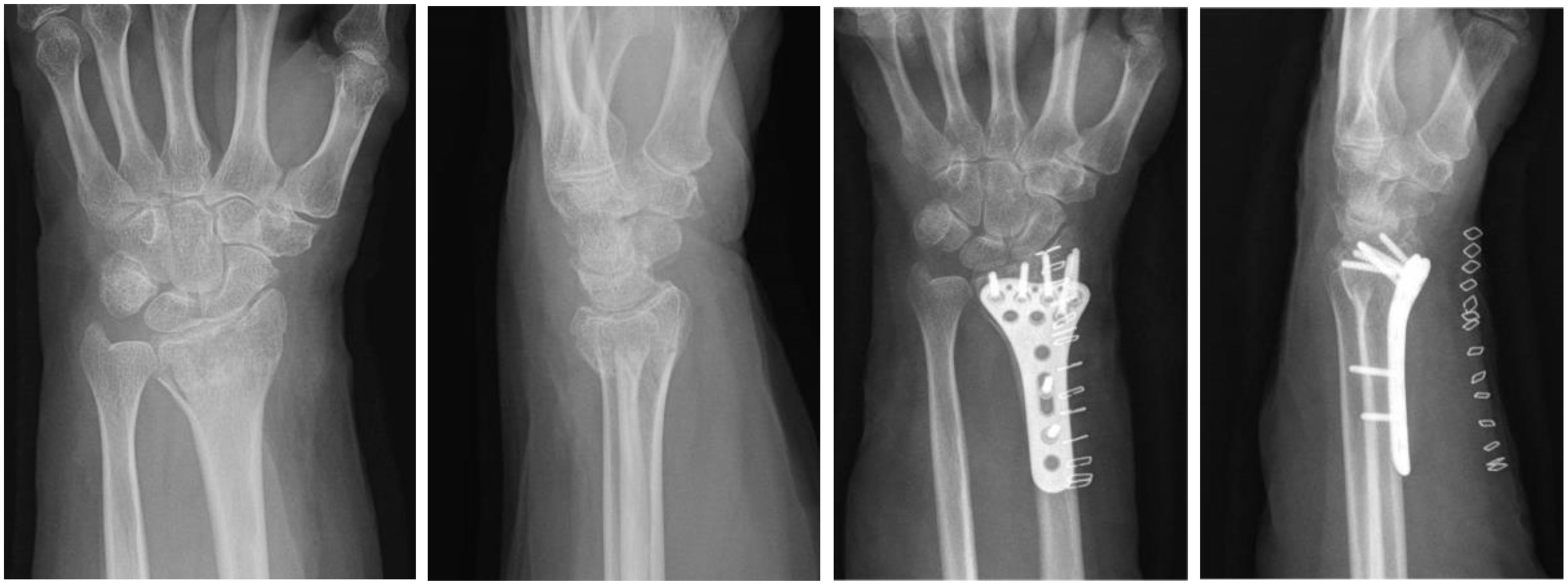
Measurement of resultsThe different visits were performed at 3, 6, and 12 weeks postoperatively where main and secondary functional variables were measured. The main variables studied were pain scores on the VAS,10 functional scores on the Patient-Rated Wrist Evaluation (PRWE) scale,11 and range of motion (ROM) in flexion and extension. The secondary variables were ROM in radial and ulnar deviation, ROM in pronation and supination, functional scores on the Disabilities of Arm, Shoulder and Hand (DASH) scale,12 functional scores on the Mayo Wrist Score (MWS),13 strength values in kilograms, and contralateral wrist strength in kilograms measured with a dynamometer. Other secondary variables to be measured were the number of complications and adverse effects (complications evaluated: shortening, secondary displacement, implant mobilisation, infection, complex regional pain syndrome, implant discomfort, tendon rupture, carpal tunnel syndrome), number of physiotherapy sessions performed on the rehabilitation ward and at home, in addition to the following radiological parameters measured preoperatively and at 3 weeks postoperatively: time to consolidation in weeks, number of fracture instability criteria according to La Fontaine (dorsal angulation >20°, dorsal or palmar comminution, ulnar styloid fracture, osteoporosis, shortening >5mm, displacement >1cm), dorsal displacement in degrees, shortening in millimetres, joint involvement in millimetres, and ulnar variance in millimetres. Radiological consolidation was assessed by plain X-ray at 3, 5, 6, and 8 weeks and by high-resolution cone-beam tomography at 6 weeks, verifying the presence of bone bridges in two planes, coronal and sagittal. The analysis of the demographic characteristics of the patients was performed by intention-to-treat and the analysis of the radiological and functional variables was performed by protocol. Preoperative and 3-week postoperative images of two DRFs are shown in Figs. 1 and 2.
The following sample size calculation was performed: to detect a standardised measurement difference of .75 points assuming equal variance between groups for the PWRE outcome variable between both study arms according to study (Watson et al.14), for a confidence level of 95%, a power of 80%, and a ratio between arms 1:1, a total of 28 patients per group will need to be evaluated, increasing by 10% to minimise potential losses to follow-up (33 patients per group and 66 in total).
Statistical methodsThe IBM SPSS Statistics programme (2022) was used for statistical analysis. Descriptive analysis was performed using measures of central tendency, dispersion, and position for quantitative variables, and frequency distribution for qualitative variables. The χ2 test (or Fisher's exact test in the case of expected frequencies of less than 5) was used for qualitative variables, and the Student's t test (or Mann–Whitney U test in the case of non-normal distribution) for quantitative variables to evaluate differences according to the study group with variables of an independent nature. Linear regression models for repeated measures with polynomial contrast were constructed to evaluate the change in radiological and functional quantitative variables at weeks 3, 6, and 12, with respect to the two treatment groups. In the different analyses, the level of statistical significance was set at p<.05.
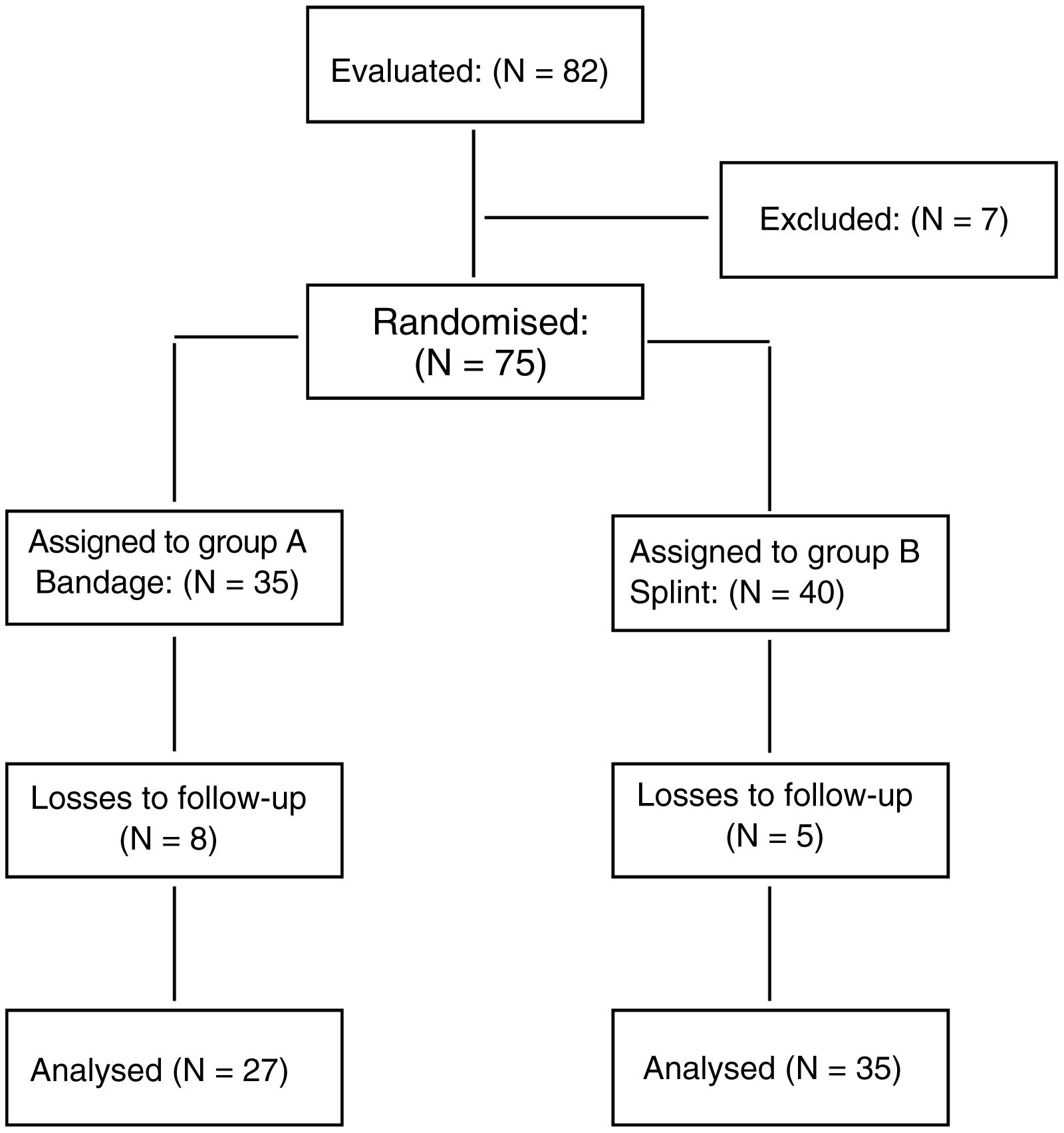
ResultsA total of 82 patients were evaluated in the study, of whom 7 were excluded prior to randomisation because the surgeons decided to treat them with plaster splinting. A total of 75 patients were randomised (35 to group A, with bandaging, and 40 to group B, with splinting). Thirteen patients were lost to follow-up due to difficulties in contacting them via telephone or mail, and a total of 62 patients were analysed for the different demographic, radiological, and functional variables (27 in group A and 35 in group B). Fig. 3 shows the distribution of the patients in the study.
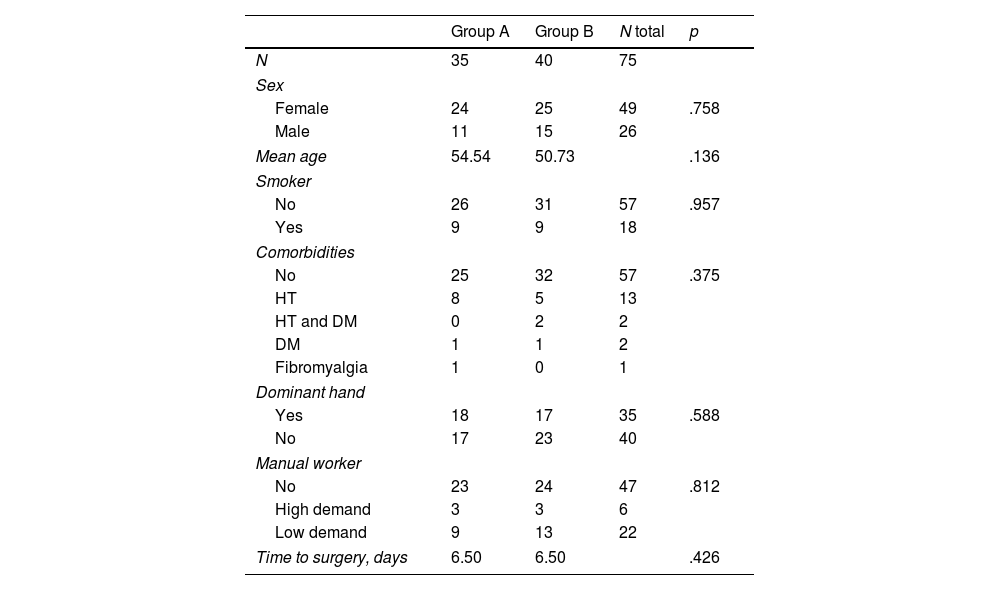
A bivariate analysis was performed between study groups of baseline sociodemographic and clinical characteristics. The results after analysis are shown in Table 1. For the patients analysed who completed follow-up there were no significant differences in these variables, and therefore it was assumed that they did not influence or confound the relationship between intervention group and outcome variables. An analysis was performed of the baseline characteristics of the losses and no differences were observed for losses in each of the groups, nor a higher percentage of losses between groups. The mean age was 54.5 and 50.7 years in the bandage and splint immobilisation groups, respectively (p=.136). The time from injury to surgical intervention was 6.5 days vs. 6.5 days in both groups (p=.426). The fractures analysed affected the female sex more frequently (49 cases in women vs. 26 cases in men; p=.758). In 57 cases studied there were no associated comorbidities, 13 cases had hypertension (HT), 2 cases had diabetes mellitus (DM), and 2 had DM and HT (p=.375). There was a higher frequency of fractures in the non-dominant limb (35 cases) with respect to the dominant (40 cases) (p=.588). Regarding work activity, patients with no or low strength demand were studied in the main (6 cases high demand vs. 22 cases low demand; p=.812).
Demographic variables.
| Group A | Group B | N total | p | |
|---|---|---|---|---|
| N | 35 | 40 | 75 | |
| Sex | ||||
| Female | 24 | 25 | 49 | .758 |
| Male | 11 | 15 | 26 | |
| Mean age | 54.54 | 50.73 | .136 | |
| Smoker | ||||
| No | 26 | 31 | 57 | .957 |
| Yes | 9 | 9 | 18 | |
| Comorbidities | ||||
| No | 25 | 32 | 57 | .375 |
| HT | 8 | 5 | 13 | |
| HT and DM | 0 | 2 | 2 | |
| DM | 1 | 1 | 2 | |
| Fibromyalgia | 1 | 0 | 1 | |
| Dominant hand | ||||
| Yes | 18 | 17 | 35 | .588 |
| No | 17 | 23 | 40 | |
| Manual worker | ||||
| No | 23 | 24 | 47 | .812 |
| High demand | 3 | 3 | 6 | |
| Low demand | 9 | 13 | 22 | |
| Time to surgery, days | 6.50 | 6.50 | .426 | |
DM: diabetes mellitus; HT: hypertension.
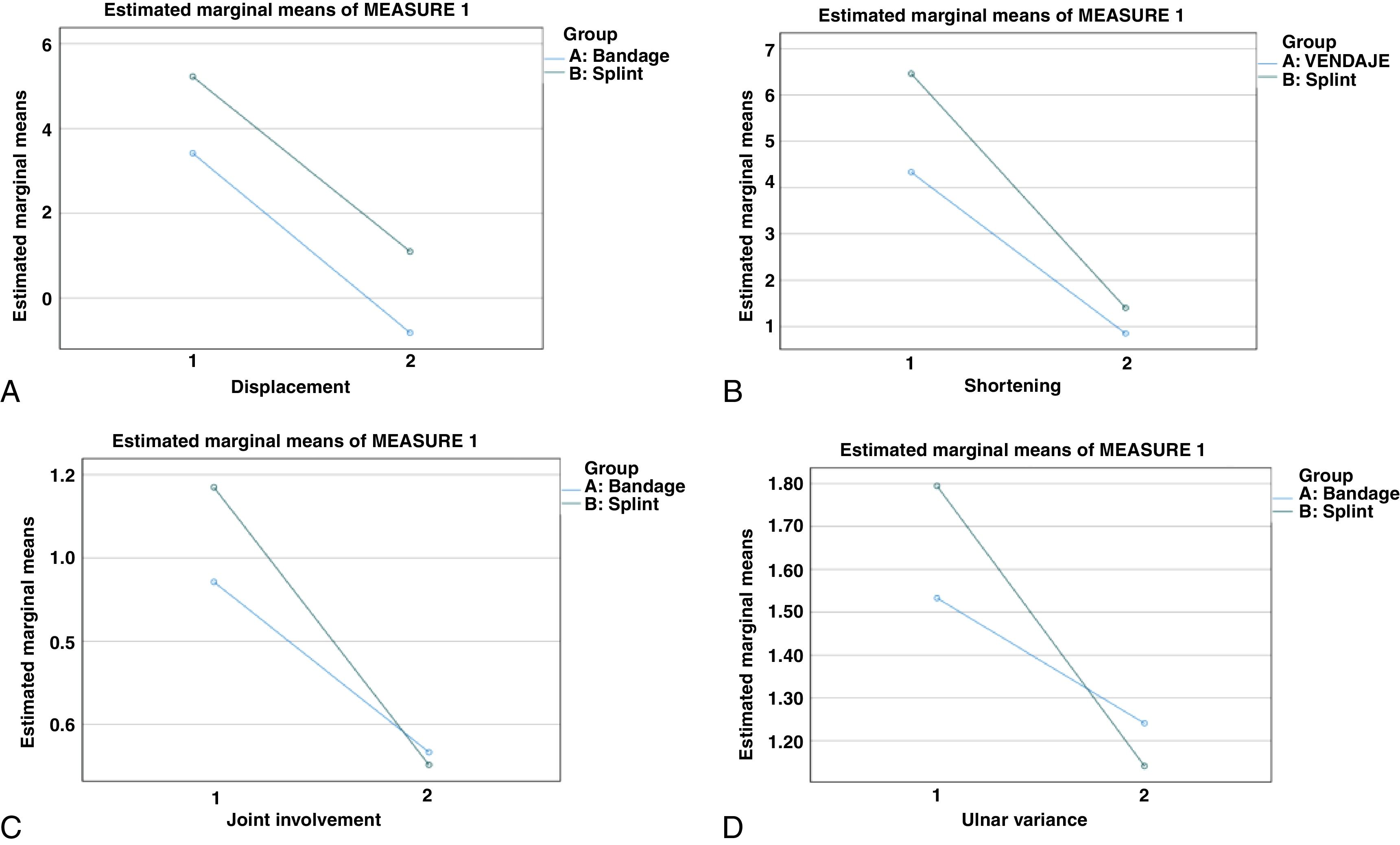
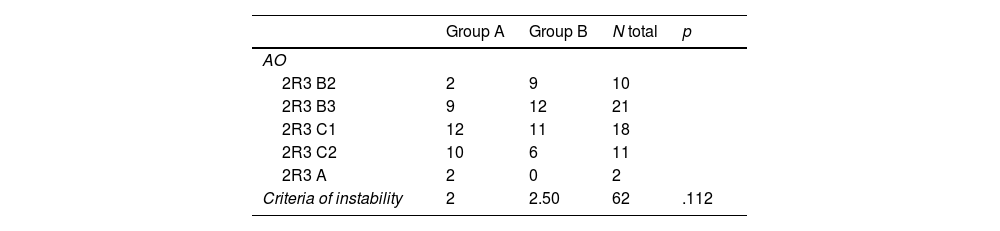
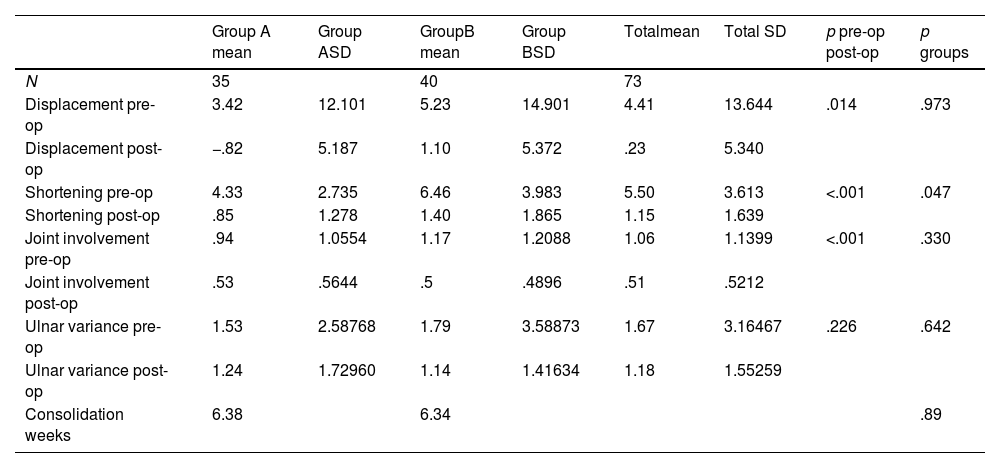
The results of the radiological parameters analysed in the study patients are shown in Tables 2 and 3 and Fig. 4. Fracture types were analysed according to the AO classification. The most frequent were classified as 2R3C1 (23 cases) and 2R3B3 fractures (21 cases). There was no difference between the two treatment groups in the number of fracture instability criteria (2 in the bandage group and 2.5 in the splint group; p=.112). No differences were obtained in the mean time to consolidation in weeks between the two groups (6.38 in the bandage group vs. 6.34 in the splint group; p=.89). Analysing the radiological variables of displacement, shortening, joint involvement, and ulnar variance, significant differences were found from pre to postoperative in both groups for all variables, but no differences were found between the two treatment groups for any variable after applying linear models of polynomial regression contrasts.
Radiological variables (2).
| Group A mean | Group ASD | GroupB mean | Group BSD | Totalmean | Total SD | p pre-op post-op | p groups | |
|---|---|---|---|---|---|---|---|---|
| N | 35 | 40 | 73 | |||||
| Displacement pre-op | 3.42 | 12.101 | 5.23 | 14.901 | 4.41 | 13.644 | .014 | .973 |
| Displacement post-op | −.82 | 5.187 | 1.10 | 5.372 | .23 | 5.340 | ||
| Shortening pre-op | 4.33 | 2.735 | 6.46 | 3.983 | 5.50 | 3.613 | <.001 | .047 |
| Shortening post-op | .85 | 1.278 | 1.40 | 1.865 | 1.15 | 1.639 | ||
| Joint involvement pre-op | .94 | 1.0554 | 1.17 | 1.2088 | 1.06 | 1.1399 | <.001 | .330 |
| Joint involvement post-op | .53 | .5644 | .5 | .4896 | .51 | .5212 | ||
| Ulnar variance pre-op | 1.53 | 2.58768 | 1.79 | 3.58873 | 1.67 | 3.16467 | .226 | .642 |
| Ulnar variance post-op | 1.24 | 1.72960 | 1.14 | 1.41634 | 1.18 | 1.55259 | ||
| Consolidation weeks | 6.38 | 6.34 | .89 |
SD: standard deviation; p groups: differences between preoperative scores and 3-week postoperative scores between both treatment groups; p pre-op post-op: differences between preoperative scores and 3-week postoperative scores in each treatment group.
Changes in radiological variables from preoperative to postoperative in the bandage immobilisation (green) and splint immobilisation (blue) groups. (A) Changes in displacement. (B) Changes in shortening. (C) Changes in joint step. (D) Changes in ulnar variance. Note that there are no differences between the two treatment groups for the variables analysed.
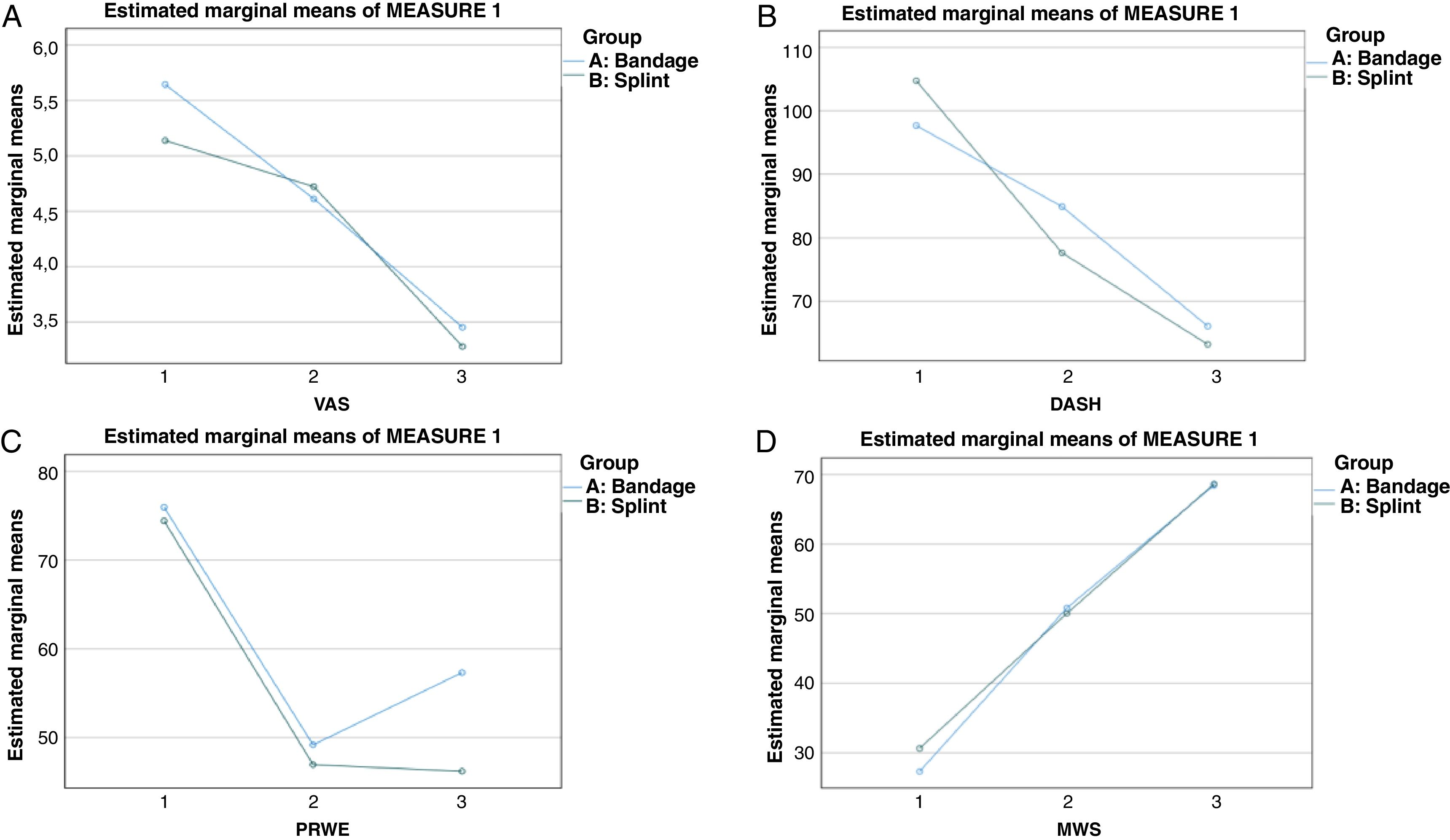
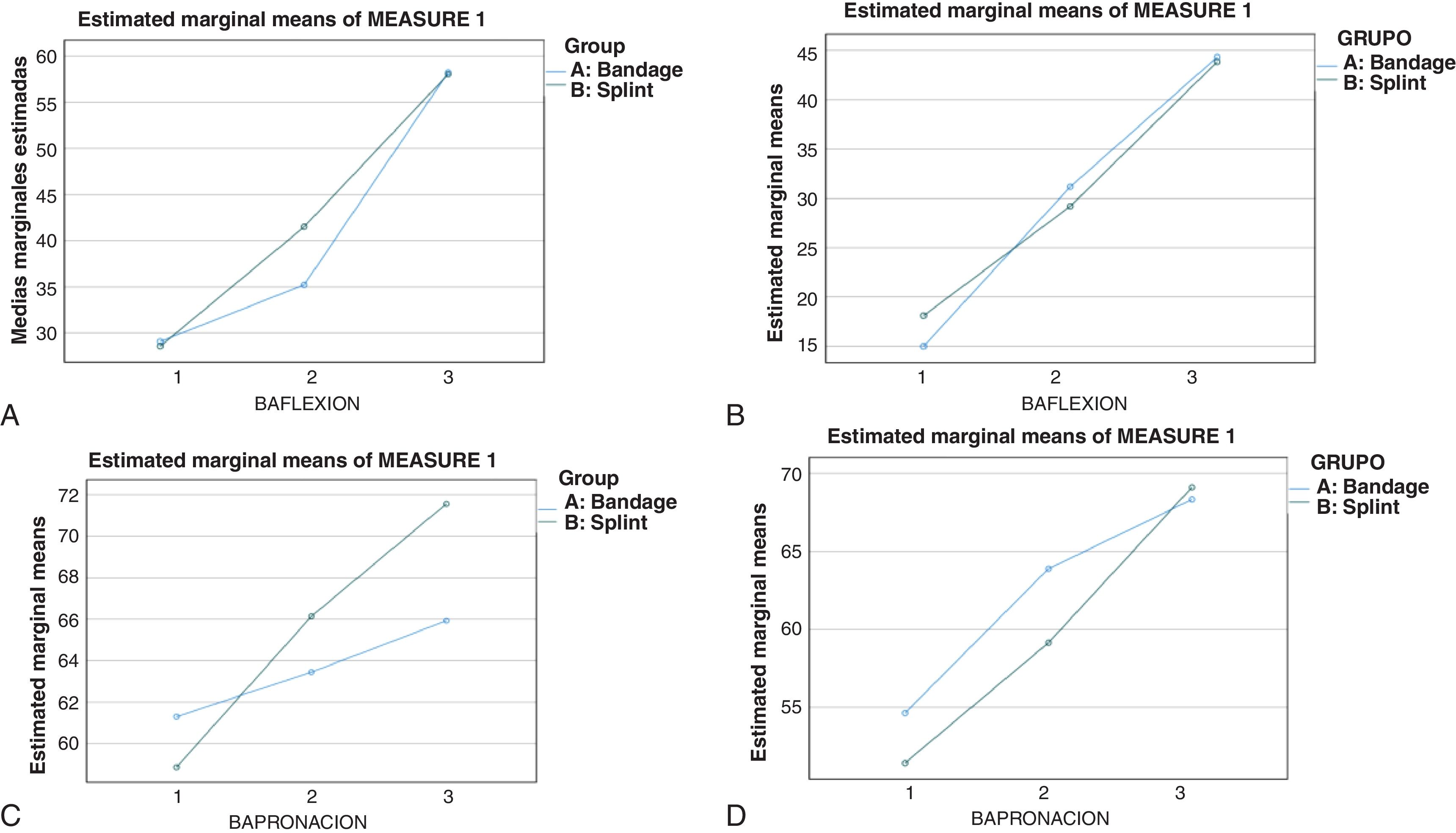
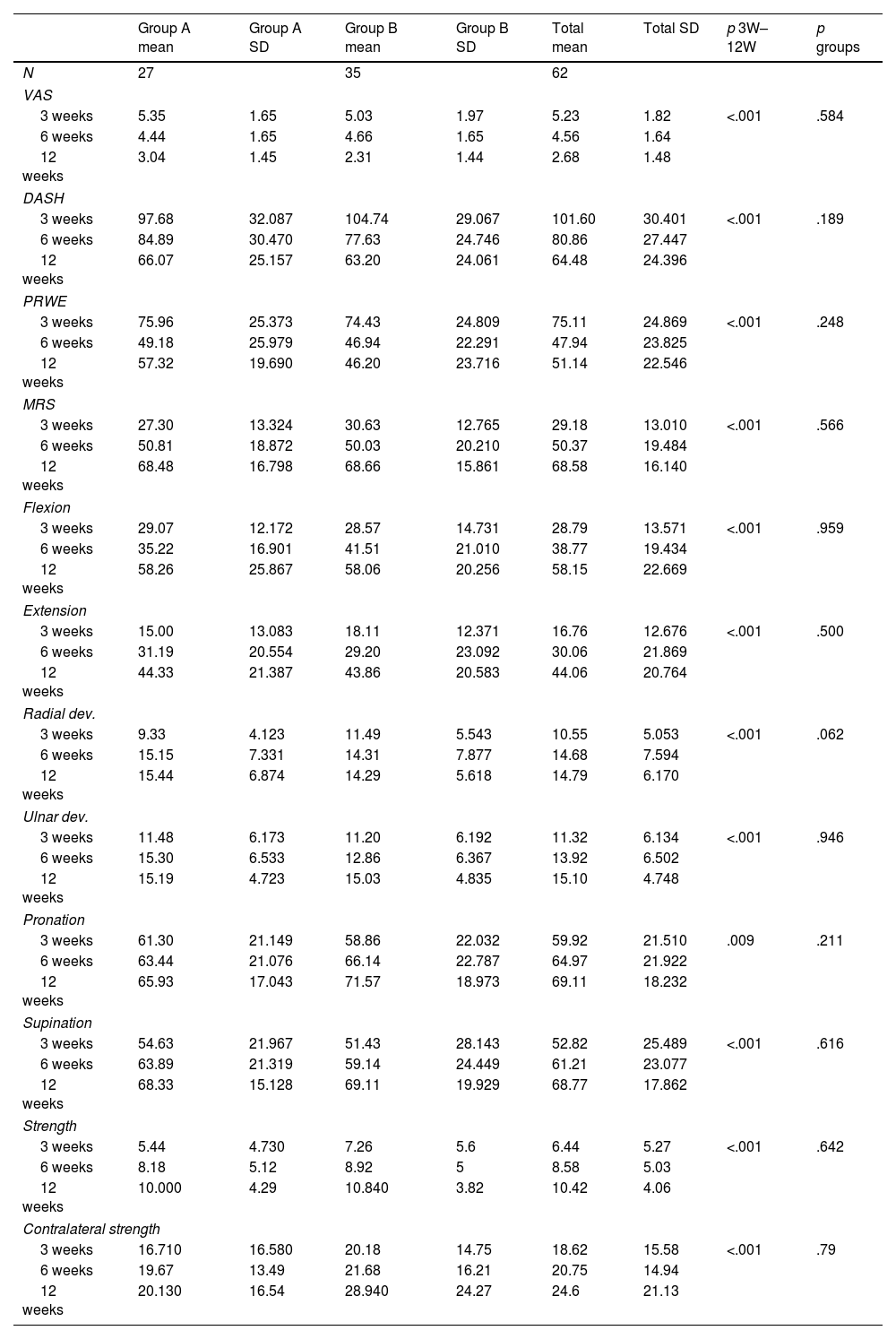
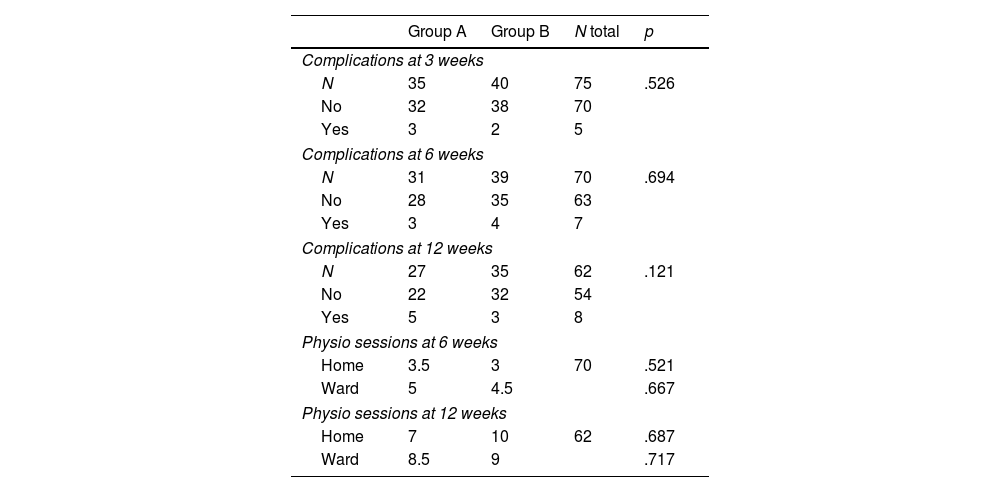
The results of the functional variables studied are shown in Tables 4 and 5, and in Figs. 5 and 6. Analysing both the primary variables (pain on the VAS scale, PRWE score, and ROM in flexion and extension) and the secondary variables (ROM in radial and ulnar deviation, ROM in pronation and supination, DASH and MWS scores, strength values, and contralateral wrist strength) significant differences were found from 3 weeks to 6 and 12 weeks in both groups for all the variables studied (with significant improvement in all parameters; p≤001), but no differences were found between the two treatment groups for any of the variables after applying linear models of regression with polynomial contrast. Neither were significant differences in favour of either treatment group found on analysis of other variables, such as the total number of complications and adverse effects at 3, 6, and 12 weeks, and the number of physical therapy sessions performed on the rehabilitation ward and at home at 6 and 12 weeks. A total of 8 complications were recorded: implant discomfort (3 cases), CTS (2 cases), CRPS (1 case), shortening (1 case), infection (1 case). At 12 weeks, the patients had required an average of 9 physiotherapy sessions in the gym and had completed an average of 10 physiotherapy sessions at home.
Functional variables.
| Group A mean | Group A SD | Group B mean | Group B SD | Total mean | Total SD | p 3W–12W | p groups | |
|---|---|---|---|---|---|---|---|---|
| N | 27 | 35 | 62 | |||||
| VAS | ||||||||
| 3 weeks | 5.35 | 1.65 | 5.03 | 1.97 | 5.23 | 1.82 | <.001 | .584 |
| 6 weeks | 4.44 | 1.65 | 4.66 | 1.65 | 4.56 | 1.64 | ||
| 12 weeks | 3.04 | 1.45 | 2.31 | 1.44 | 2.68 | 1.48 | ||
| DASH | ||||||||
| 3 weeks | 97.68 | 32.087 | 104.74 | 29.067 | 101.60 | 30.401 | <.001 | .189 |
| 6 weeks | 84.89 | 30.470 | 77.63 | 24.746 | 80.86 | 27.447 | ||
| 12 weeks | 66.07 | 25.157 | 63.20 | 24.061 | 64.48 | 24.396 | ||
| PRWE | ||||||||
| 3 weeks | 75.96 | 25.373 | 74.43 | 24.809 | 75.11 | 24.869 | <.001 | .248 |
| 6 weeks | 49.18 | 25.979 | 46.94 | 22.291 | 47.94 | 23.825 | ||
| 12 weeks | 57.32 | 19.690 | 46.20 | 23.716 | 51.14 | 22.546 | ||
| MRS | ||||||||
| 3 weeks | 27.30 | 13.324 | 30.63 | 12.765 | 29.18 | 13.010 | <.001 | .566 |
| 6 weeks | 50.81 | 18.872 | 50.03 | 20.210 | 50.37 | 19.484 | ||
| 12 weeks | 68.48 | 16.798 | 68.66 | 15.861 | 68.58 | 16.140 | ||
| Flexion | ||||||||
| 3 weeks | 29.07 | 12.172 | 28.57 | 14.731 | 28.79 | 13.571 | <.001 | .959 |
| 6 weeks | 35.22 | 16.901 | 41.51 | 21.010 | 38.77 | 19.434 | ||
| 12 weeks | 58.26 | 25.867 | 58.06 | 20.256 | 58.15 | 22.669 | ||
| Extension | ||||||||
| 3 weeks | 15.00 | 13.083 | 18.11 | 12.371 | 16.76 | 12.676 | <.001 | .500 |
| 6 weeks | 31.19 | 20.554 | 29.20 | 23.092 | 30.06 | 21.869 | ||
| 12 weeks | 44.33 | 21.387 | 43.86 | 20.583 | 44.06 | 20.764 | ||
| Radial dev. | ||||||||
| 3 weeks | 9.33 | 4.123 | 11.49 | 5.543 | 10.55 | 5.053 | <.001 | .062 |
| 6 weeks | 15.15 | 7.331 | 14.31 | 7.877 | 14.68 | 7.594 | ||
| 12 weeks | 15.44 | 6.874 | 14.29 | 5.618 | 14.79 | 6.170 | ||
| Ulnar dev. | ||||||||
| 3 weeks | 11.48 | 6.173 | 11.20 | 6.192 | 11.32 | 6.134 | <.001 | .946 |
| 6 weeks | 15.30 | 6.533 | 12.86 | 6.367 | 13.92 | 6.502 | ||
| 12 weeks | 15.19 | 4.723 | 15.03 | 4.835 | 15.10 | 4.748 | ||
| Pronation | ||||||||
| 3 weeks | 61.30 | 21.149 | 58.86 | 22.032 | 59.92 | 21.510 | .009 | .211 |
| 6 weeks | 63.44 | 21.076 | 66.14 | 22.787 | 64.97 | 21.922 | ||
| 12 weeks | 65.93 | 17.043 | 71.57 | 18.973 | 69.11 | 18.232 | ||
| Supination | ||||||||
| 3 weeks | 54.63 | 21.967 | 51.43 | 28.143 | 52.82 | 25.489 | <.001 | .616 |
| 6 weeks | 63.89 | 21.319 | 59.14 | 24.449 | 61.21 | 23.077 | ||
| 12 weeks | 68.33 | 15.128 | 69.11 | 19.929 | 68.77 | 17.862 | ||
| Strength | ||||||||
| 3 weeks | 5.44 | 4.730 | 7.26 | 5.6 | 6.44 | 5.27 | <.001 | .642 |
| 6 weeks | 8.18 | 5.12 | 8.92 | 5 | 8.58 | 5.03 | ||
| 12 weeks | 10.000 | 4.29 | 10.840 | 3.82 | 10.42 | 4.06 | ||
| Contralateral strength | ||||||||
| 3 weeks | 16.710 | 16.580 | 20.18 | 14.75 | 18.62 | 15.58 | <.001 | .79 |
| 6 weeks | 19.67 | 13.49 | 21.68 | 16.21 | 20.75 | 14.94 | ||
| 12 weeks | 20.130 | 16.54 | 28.940 | 24.27 | 24.6 | 21.13 | ||
DASH: Disabilities of Arm, Shoulder and Hand; Dev.: deviation (radial or ulnar); MRS: Mayo Wrist Score; p 3W–12W: differences from 3 to 12-week postoperative scores in each treatment group; p groups: differences from 3 to 12 weeks postoperatively between the two treatment groups; PRWE: Patient-Rated Wrist Evaluation; SD: standard deviation; VAS: Visual Analogue Scale.
Functional variables (2).
| Group A | Group B | N total | p | |
|---|---|---|---|---|
| Complications at 3 weeks | ||||
| N | 35 | 40 | 75 | .526 |
| No | 32 | 38 | 70 | |
| Yes | 3 | 2 | 5 | |
| Complications at 6 weeks | ||||
| N | 31 | 39 | 70 | .694 |
| No | 28 | 35 | 63 | |
| Yes | 3 | 4 | 7 | |
| Complications at 12 weeks | ||||
| N | 27 | 35 | 62 | .121 |
| No | 22 | 32 | 54 | |
| Yes | 5 | 3 | 8 | |
| Physio sessions at 6 weeks | ||||
| Home | 3.5 | 3 | 70 | .521 |
| Ward | 5 | 4.5 | .667 | |
| Physio sessions at 12 weeks | ||||
| Home | 7 | 10 | 62 | .687 |
| Ward | 8.5 | 9 | .717 | |
Home: rehabilitation sessions at home; ward: rehabilitation sessions on the physiotherapy ward.
Changes in functional parameters at 3, 6, and 12 weeks in the bandage immobilisation group (blue) and splint immobilisation group (green). (A) Changes in VAS score. (B) Changes in DASH score. (C) Changes in PRWE score. (D) Changes in MWS score. Note that there are no differences between the two treatment groups for the parameters analysed.
Changes in functional parameters from 3 to 6 and 12 weeks in the bandage immobilisation group (blue) and splint immobilisation group (green). (A) Changes in ROM scores in flexion. (B) Changes in ROM scores in extension. (C) Changes in ROM scores in pronation. (D) Changes in ROM scores in supination. Note that there are no differences between the two treatment groups for the parameters analysed.
The present study compares functional and radiological parameters between two types of postoperative immobilisation after DRF treated with plate osteosynthesis: immobilisation with plaster splint for 3 weeks, and immobilisation with compression bandage for 3 weeks, allowing immediate assisted passive mobility in the latter group. Analysing the functional variables evaluated over postoperative weeks 3, 6, and 12, improvement was similar in the two groups, without significant differences in favour of one or the other group in terms of pain, range of motion, functional scales, complications, etc. Analysing the different radiological variables evaluated from preoperative to 3 weeks postoperatively, the improvement in these variables was also similar in both study groups. Currently, the choice of the type of postoperative immobilisation after plate osteosynthesis in DRF is a matter of controversy among many hand surgeons. The criteria of choice are mainly based on the characteristics of each fracture, personal experiences, or the experiences of other more experienced surgeons, due to the lack of scientific evidence in the current literature. This clinical trial helps us to advance in the search for evidence on the most appropriate type of immobilisation, a factor that could impact the quality of care and the overall healthcare cost of this type of injury, which is so frequent in our hospital setting.
The most recent literature focuses primarily on the search for the optimal immobilisation time or initiation of mobility after plate fixation in DRF, which remains a matter of controversy. A 2015 Cochrane review concludes that there is insufficient evidence on the effectiveness of different rehabilitation protocols.15 Most studies show no differences in range of motion and strength at 3 and 6 months post-operatively, regardless of when the limb begins to mobilise, and therefore the benefits of early mobilisation would diminish after this period of time.5–7 A study by Lozano-Calderón et al.8 compared the initiation of mobilisation in the first 2 postoperative weeks, and the initiation of mobilisation after 6 weeks postoperatively, and concluded that late mobilisation does not worsen functional outcomes at 3 and 6 months.
However, many other studies show that when immobilisation exceeds 4 weeks, the time to achieve functional mobility ranges is delayed up to 3 months and early mobilisation accelerates the recovery of these functional scores.2,16 Watson et al.,14 after comparing immobilisation for a period of 1, 3, and 6 weeks, conclude that the first two groups show better results at 6 weeks and similar results at 3 and 6 months. In a retrospective study Toemen et al.3 compare the short-term functional results after mobilisation from the first 2 or 4 weeks, concluding that the group mobilised at 2 weeks obtains better functional results, return about 45 days earlier to their work activity, and are discharged earlier from physiotherapy. Prolonging the time required for rehabilitation in patients immobilised for 4 or more weeks would significantly increase the healthcare cost, as indicated by the study by Valdés.16 Some biomechanical studies have shown that simultaneous active digital movement produces an axial load on the wrist greater than that produced by habitual wrist movements in daily life. Fixation with a volar locking plate provides five times greater stability to the forces caused by finger movement, which should be considered to support early mobilisation after surgery.17
Only two reviewed studies analyse results after immediate mobility in DRF fixed with a plate. A study by Quadlbauer et al.2 compared a group immobilised for one week and allowed early mobilisation from the outset with a group immobilised for 5 weeks, and the early mobilisation group obtained superior results in terms of range of motion in the sagittal plane (up to 6 months), range of motion in the frontal plane (up to 9 weeks), forearm rotation (up to 6 weeks), grip strength (up to 6 months), and functional values (up to 6 weeks). This is the only study to analyse radiological variables in fractures according to immobilisation. However, this study was performed with a small sample size (28 patients) and does not specify the immobilisation and non-immobilisation time during the first week in the early mobility group. Osada et al.17 treated 49 operated fractures in a study indicating immediate mobility without immobilisation. At one year, they showed very satisfactory functional and radiological results. However, the patients did not undergo a controlled rehabilitation programme, and they did not compare the results with other groups with immobilised fractures.
A recent study by Stuby et al.18 compares different methods of immobilisation after DRF treated with locking plate: immobilisation with plaster splint and immobilisation with flexible dynamic orthosis for 4 weeks, showing some advantages in the dynamic orthosis group in terms of functional results at 4 weeks and in patient satisfaction with the treatment performed. Therefore, the flexible dynamic orthosis could be considered an alternative to the plaster splint for postoperative immobilisation.
The study has some limitations. First, although the evaluator of the study results was blinded to randomisation at all times, it was not possible to apply masking techniques to the participants and principal investigators (from the time of intervention allocation and throughout follow-up it was not possible to conceal from patients and investigators the treatment group to which each participant belonged). Secondly, the internal validity of the study could be affected by the total number of losses recorded throughout the follow-up of the participants and by the difficulty in obtaining accurate data on variables such as radiological consolidation time, number of physiotherapy sessions performed, and other variables that require very close control and follow-up of the patients, made difficult by the recent pandemic. These aspects should be considered when interpreting the results, as should it not having been possible to achieve anatomical reductions in some cases, which could affect the functional results in both treatment groups. Finally, the sample size is small, and in one of the groups it was not possible to meet the sample size calculated for the study protocol due to losses, which could limit the external validity or the possibility of extrapolating the results to the population to which the results can be applied.
ConclusionsFrom the results of our study, we concluded that we found no clinical or radiological differences between immobilisation with antebrachial plaster splint and immobilisation with cotton compression bandage for joint fractures of the distal radius treated with plate osteosynthesis. Our results do not show differences between the treatment groups, and therefore we cannot confirm that one treatment is superior to the other in terms of postoperative pain, joint range of motion, global function of the affected limb, global complications, and radiological consolidation. However, a larger number of patients and a longer follow-up of these patients are necessary to obtain more valid results and to establish criteria that will help manage distal radius fractures appropriately in the postoperative period.
Level of evidenceLevel of evidence I.
FundingThis research received no specific grant from any funding agency in the public, commercial or not-for-profit sector.
Conflict of interestsThe authors have no conflict of interests to declare.