One of the most frequently treated pathologies in our department are tendon lesions that affect the rotator cuff of the shoulder. There are different types of treatment for massive or irreparable tears. For a few years, a low-invasive technique was introduced based on the placement of a biodegradable subacromial spacer. The objective of the work is to analyse the results of our experience with the use of this device (InSpace™).
Material and methodThe study collects the results obtained in 25 patients with irreparable ruptures of rotator cuff defined by RM, in which they were implanted a balloon subacromial in our centre in the period from January 2015 — until December 2017. All patients were evaluated preoperatively and one year after surgery including the visual analogue scale (VAS), the Constant test (CS) and the QuickDASH (QD).
ResultsOf the 25 patients, 5 patients (20%) were operated by arthroscopy and 20 (80%) By open approach (mini-open). A total of 22 patients completed the follow-up year. At 12 months, 64% of the patients obtained an improvement of at least 10 points in the CS. Patients departed from an initial average CS of 32 points that improved to 54.9 points of average in the postoperative evaluation at 12 months (average improvement 22.9 points; value-p < 0.05). In terms of pain assessment, in our study, 87% of patients obtained an improvement of at least 2 points in the EVA at 12 months of follow-up (p-value < 0.05). Patients departed from an initial average EVA of 8.7 that improved to 3.7 points average at 12 months. 73% of the patients responded to be satisfied with the intervention and would return to the surgery.
ConclusionThe results obtained in our series to one year of follow-up speak in favour of the use of the Subacromial Balloon (InSpace™), as a therapeutic option available for patients with irreparable ruptures of the rotator cuff. It can be used as an interim procedure, delaying the need for more invasive surgery, or as a definitive procedure in patients medically non-candidates for reverse arthroplasty. It is important to have clear indications of this procedure in order not to make mistakes.
Una de las patologías más frecuentemente atendida en nuestro medio son las lesiones tendinosas que afectan al manguito rotador del hombro. Existen diferentes modalidades de tratamiento para las roturas masivas o irreparables. Desde hace unos años, se introdujo en el mercado una técnica poco invasiva basada en la colocación de un espaciador subacromial biodegradable. El objetivo del trabajo es analizar los resultados de nuestra experiencia con el uso de este dispositivo (InSpace®).
Material y métodoEn el estudio se recogen los resultados obtenidos en 25 pacientes con roturas irreparables del manguito rotador definidas mediante resonancia magnética (RM), en los que se les implantó un balón subacromial en nuestro centro en el periodo comprendido entre enero de 2015 hasta diciembre de 2017. Todos los pacientes fueron evaluados preoperatoriamente y un año después de la cirugía incluyendo la escala visual analógica (EVA), el test de Constant (CS) y el QuickDASH (QD).
ResultadosDe los 25 pacientes, cinco pacientes (20%) fueron intervenidos mediante artroscopia y 20 (80%) mediante abordaje abierto (mini-open). Un total de 22 pacientes completaron el año de seguimiento. A los 12 meses, el 64% (14/22) de los pacientes obtuvo una mejoría de al menos 10 puntos en el CS. Los pacientes partían de un CS promedio inicial de 32 puntos que mejoró hasta los 54,9 puntos de media en la evaluación postoperatoria a los 12 meses (Promedio de mejoría 22,9 puntos; p < 0,05). En cuanto a la evaluación del dolor, en nuestro estudio, el 87% (19/22) de los pacientes obtuvo una mejoría de al menos 2 puntos en la EVA a los 12 meses de seguimiento (p < 0,05). Los pacientes partían de una EVA media inicial de 8,7 que mejoró hasta los 3,7 puntos de media a los 12 meses. Un 73% de los pacientes contestaron estar satisfechos con la intervención y volverían a someterse a la cirugía.
ConclusiónLos resultados obtenidos en nuestra serie a un año de seguimiento hablan en favor de la utilización del balón subacromial de tipo InSpace®, como opción terapéutica disponible para pacientes con roturas irreparables del manguito rotador. Puede ser utilizado como procedimiento provisional, retrasando la necesidad de una cirugía más invasiva, o definitivo en los pacientes médicamente no candidatos a una artroplastia inversa. Es importante tener claras las indicaciones de este procedimiento para no cometer errores.
One of the most frequently treated pathologies in our department are tendon lesions that affect the rotator cuff (RC) of the shoulder. Treatment for repairable tears using arthroscopic or open surgery techniques produce favourable results. There is debate regarding type of treatment in patients with massive or irreparable tears. Although no consensus has been reached in the definition of massive tears, they are considered to be tears that affect two or more tendons, with a medial retraction of approximately 3–5 cm. It has also be estimated that a tear is irreparable when the tendons cannot be sutured directly to the insertion footprint, due to their size, to retraction, to tissue quality (fatty infiltration over 50%, Goutallier grade 3–4)1 after specific mobilisation and release of the injured tendon ends.2 In these patients different alternatives are suggested, such as wide debridements; tenotomies of the long head biceps (LHB); partial repairs; tendon transfers; use of allografts; superior capsular reconstruction3 or inverse arthroplasty.
Some years ago a low invasive technique was introduced into the market, based on a biodegradable InSpace® type subacromial spacer. As the name suggests, the technique consists in introducing this saline-filled device in the subacromial space, as a spacer between the acromion and the humeral head.4 The spacer is manufactured with 12-month biodegradable polymer, following which the material is reabsorbed. The main objective of the spacer is to restore the biomechanics of the shoulder,5 replicating the effect of a drop in the humeral head by the RC tendons, thereby reducing subacromial friction.
The main reason for this procedure would be pain reduction in patient affected by massive and irreparable TC tears, where an alternative is sought prior to carrying out a more invasive procedure such as, for example, inverse shoulder arthroplasty. However, cases have been described in the literature in which this device has also been used in partial RC tears, combining tendon suture with implantation of the spacer balloon.6,7
A series of criteria have been published to guide surgeons as to which patients would be candidates for this intervention. Firstly, age. This procedure is not recommended in patients under 50 years of age, since in these cases better alternatives may exist for cuff reconstruction, including tendon transfers or superior capsular reconstruction. Secondly, the patient should maintain a correct passive joint range of the shoulder, as favourable outcomes are not obtained in the so-called pseudoparalytic shoulder. Also, there should not be any glenohumeral osteoarthritis (indication only in stages 1–2 of the Hamada classification).8 In patients with advanced osteoarthritis, inverse arthroplasty would immediately be indicated. Another aspect to bear in mind is that the device only increases the subacromial space and it must therefore be retained in this compartment, thereby requiring anatomical “stability” for correct functioning. Stability comes from deltoid muscle action, increasing the pressure in the space, through the acromion in the posterior region and through the coracoacromial ligament in the anterior region. In patients who had undergone previous interventions, such as acromioplasties, where the anatomy was altered, there was increased migration of the balloon outside the subacromial space, mainly with anterior displacements.
The aim of this study was to analyse the outcomes of our experience with the use of biodegradable InSpace® type spacer balloons and compare them with those described in the literature.
Material and methodsA prospective study was conducted of a consecutive case series with irreparable tears of the rotator cuff, where a subacromial balloon was implanted during the period between January 2015 and December 2017. All interventions were made in the same centre by three different surgeons.
Rotator cuffs were considered to be irreparable when no anatomical reconstruction could be made following surgery. They all presented with a complete tear of the supraspinatus tendon with retraction of over 3–4 cm and with a fatty infiltration above 50% (Goutallier grade 3–4)1, defined by MRI. One important criterion was that the patients maintained a good joint range with passive movement of the shoulder. Another criteria used was the absence of significant degenerative changes in plain radiology (Hamada 1–2).8 The decision to perform surgery was made after failure of non surgical treatment and rehabilitation of at least six months. All patients were informed about the treatment characteristics and gave their informed, written consent. Unlike other published works, there was no biceps-associated tenotomy9 in all cases where the biceps was present. This study did not include having been previously operated on as an exclusion criteria for our patients.
The InSpace® type subacromial balloon spacer was implanted in 25 patients, 20 using mini-open approach and five using arthroscopy with the manufacturer’s suggested technique. Regardless of the type of approach, the appropriate device size was selected by measuring the space between the lateral edge of the trochanter and 1 cm medial to the superior edge of the glenoid ridge. Once inserted, correct positioning and stability was confirmed with the passive movement of the shoulder. All patients were assessed preoperatively and one year after surgery. An assessment was made which included the visual analogue scale (VAS), the Constant scale (CS) and the QuickDASH (QD). The main variables of satisfactory evolution were established as an improvement of at least 10 points in the Constant test, an improvement of at least 2 points on the VAS and a drop of 15 points in the QuickDASH test. The statistical technique used for analysis of the three variables was the student’s t-test. A normality test was performed applying the Shapiro–Wilk test, obtaining p > .05 in the three variables.
The patients included in the study adhered to the same protocol of rehabilitation in our centre. After surgery, a sling was used for the first two to three weeks. After this period, rehabilitation treatment began, aimed at recovering range of movement and strength.
ResultsOf the 25 patients, five (20%) underwent arthroscopy and 20 (80%) mini-open surgery. A total of 22 patients completed the year-long follow-up. Two patients were excluded because they did not carry out the set clinical controls and another patient did not complete the study as they were re-operated for removal of material, on suspicion of infection.
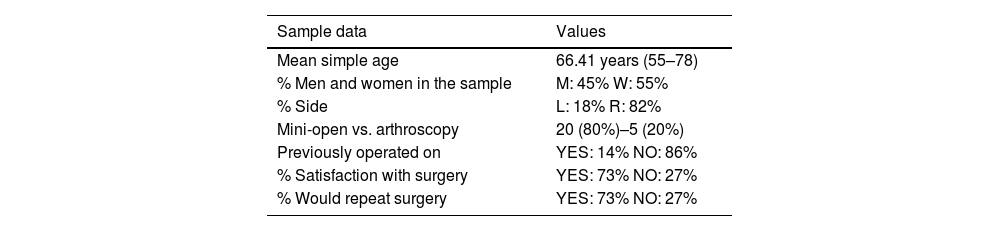
The study patients presented with a mean age of 66.4 years (55–78 year range), and were mostly female (55%) compared with male (45%). The side was predominantly the right (82%). Of the patients who completed follow-up, three (14%) had previously undergone acromioplasty, and with RC-associated repair in two of them.
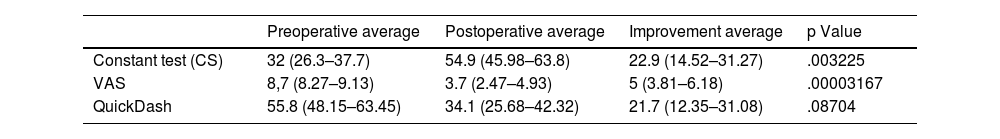
Regarding functional evaluation of the patients 12 months after surgery, 64% of them had improved by at least 10 points in the CS, with statistical significance being observed (p = .003225). With regards to pain assessment, 87% of patients obtained an improvement by at least 2 points on the VAS at 12 months follow-up, with a new statistical significance being observed (p = .00003167). However, despite the fact that 64% of patients obtained an improvement of at least 15 points in the QD, results were not statistically significant (p = .08704).
All patients were asked two questions to assess the level of satisfaction with surgery. Seventy three per cent of the patients replied they were satisfied with the intervention and would receive surgery again.
Of the cases included in the study, one patient had to receive further surgery 15 days after intervention for material extraction, on suspicion of infection. Purulent looking material was observed on extraction of the implant. This extended from subcutaneous cellular tissue to the subacromial area, around the balloon which had deflated. The inflammatory markers showed no significant changes, with the CRP at 5 mg/L. Systemically the patient did not have a fever or general malaise. Cultures tested negative. In the light of the results final diagnosis was reaction to a foreign body.
Outside the follow-up period, 18 months after surgery, one patient received further surgery because there was no clinical improvement, with an inverse arthroplasty of the shoulder.
DiscussionIf we look at the main objectives of an InSpace®, type subacromial balloon spacer which are to relieve pain and restore joint function, we believe that the results obtained from our study are consistently in favour of the use of this device. If we compare them with other studies we have successfully partially reproduced the satisfactory results of Senekovic et al.6 and Gervasi et al.,10 two of the publications which analysed case series with positive results. Notwithstanding, our results are not concordant with those obtained in the study by Lorente Gómez et al.11 On comparison of the patients in our study with these others, we observed that the sample size of the study is similar to that of Senekovic et al. (n = 24) and higher than that of Gervasi et al. (n = 15) and Lorente et al. (n = 15). The mean age of our group, at 66.4 years, is lower, but mostly similar to that of the Senekovic et al. (68.8 years) groups and the Lorente et al. (69.4 years) groups, and quite a lot lower than that Gervasi et al. (74,6 years) group.
In our study, after 12 months of follow-up, 64% (14/22) of patients obtained an improvement of at least 10 points in the CS. The patients had an initial average CS of 32 points which rose up to 54.9 mean points in postoperative assessment at 12 months (average improvement 22.9 points; p < .05). Gervasi et al., in a series of 15 patients (seven men, eight women) with a mean age of 74.6 years, after 12 months follow-up reported that 85% showed changes of at least 15 points in the CS. The patients began with a Constant mean of 31.9 points initially which improved up to a mean of 69.8 in the postoperative assessment at 12 months. Senekovic et al. Presented a series of 24 patients (12 women, 12 men) with a mean age of 68.8 years, in which, after five years of follow-up 84.6% of patients for the series presented an improvement of at least 15 points in the CS and 61.54% of at least 25 points. Our results differ from those observed in the study by Lorente et al., in that in a series of 15 patients (11 women/four men) when the main variable was assessed (clinically relevant improvement of the Constant and no further surgery) only eight patients (53.3%) met with these criteria. Therefore, the success rate for these subjects after one year was 53.3%.
Regarding pain assessment, in our study 87% (19/22) of patients obtained an improvement of at least 2 points on the VAS at the 12 months follow-up (p < .05). Patients had an initial mean VAS of 8.7 which improved up to a mean of 3.7 points in the postoperative assessment at 12 months. Gervasi et al., described an improvement of 6.4 points in the subjective assessment of pain (using the scales included in the CS and in the American Shoulder and Elbow Society [ASES]). They also referred to pain improvement beginning two weeks after the implantation of the balloon spacer. Senekovic et al., stated that the patients experienced a significant improvement in pain which began the first week after surgery. This improvement remained and even increased, being statistically positive, during posterior follow-up (three years, average improvement 6.11 points [p < .05]). In our series, despite having no objective data after two weeks or in the first months of evolution following surgery, we observed that pain improvement was felt over the months. Initially, many patients did not perceive of a clear improvement, but after one year there was a clearly significant, appreciable difference. Given that one of the main aims of the balloon space is pain relief, we believe results may be considered favourable.
One alternative to using the subacromial balloon would be the consistent technique in superior capsular reconstruction of the shoulder with a fascia lata autograft, as described by Mihata et al.3 in 2013. In their study, they presented the clinical outcomes of a series of 24 shoulders in 23 patients with massive irreparable rotator cuff tears. They described favourable outcomes, with postoperative improvement in both functional assessment –ASES–: increase of 23.5–92.9 points (p < .0001) and in increased joint range (increase in active flexion: from 84° to 148° [p < .001]), and external rotation: from 26° to 40° (p < .01)] at 34.1 months mean follow-up. Although it is a surgical alternative, this intervention, unlike that of the subacromial balloon technique, is technically more demanding and outcomes are often considered to depend greatly upon the surgeon’s experience.
Hypothesis on poor outcomesThere are several hypotheses as to why poor outcomes after balloon implantation are sometimes obtained. One is early migration of the device outside of the subacromial space and the other is mechanical implant failure. In our experience over the last three years we have had three cases (patients not included in the study) of anterolateral balloon migrations confirmed by imaging tests (ECO/MRI). Two of them had previously undergone acromioplasty with RC repair-associated corocoacromial ligament section. The patients had to be re-operated for removal of the device. There are two main hypotheses regarding mechanical implant failure: one could be a failure of the seal after filling with saline (case included in the study where the implant material was removed due to reaction to a foreign body 15 days after the intervention, the balloon having deflated), and the other could be early reabsorption of the device before 12 months, as described in the article by Lorente Gómez et al.11
Another fact which could justify an unsatisfactory evolution with balloon spacer use could be the failure to stabilize the anterior and posterior rotators as far as possible. We believe that partial repair associated with the rotator cuff muscles could help to improve patient evolution. Several authors describe the association of partial repair with the subacromial balloon technique with favourable outcomes.12,13
Aside from the various hypotheses put forward, we believe that the main reason for an unsatisfactory outcome is a poor surgical indication. The balloon spacer is a device whose main function is to reduce pain in patients with an irreparable RC, when an alternative is sought prior to a more invasive procedure. As was explained in the introduction, we believe that the ideal patient is a person aged over 50 years, with an irreparable RC tear, where there is no glenohumeral osteoarthritis, who maintains a good passive joint range of the shoulder and who has not been operated on previously. It has been observed that patients who undergo previous surgery where their anatomy is perceived as altered, may be inclined towards migration of the balloon spacer outside the subacromial space. Most balloon spacer displacements described were anterior, which is why we consider that one of the most important structures for stabilizing the device, together the anterior acromion edge, is the coracoacromial ligament and this structure must therefore be preserved (Tables 1–3).
Descriptive sample data.
| Sample data | Values |
|---|---|
| Mean simple age | 66.41 years (55–78) |
| % Men and women in the sample | M: 45% W: 55% |
| % Side | L: 18% R: 82% |
| Mini-open vs. arthroscopy | 20 (80%)–5 (20%) |
| Previously operated on | YES: 14% NO: 86% |
| % Satisfaction with surgery | YES: 73% NO: 27% |
| % Would repeat surgery | YES: 73% NO: 27% |
Comparison of Constant test, VAS and QuickDASH, before and after subacromial balloon spacer implantation, at 12 months. Statistical analysis.
| Preoperative average | Postoperative average | Improvement average | p Value | |
|---|---|---|---|---|
| Constant test (CS) | 32 (26.3–37.7) | 54.9 (45.98–63.8) | 22.9 (14.52–31.27) | .003225 |
| VAS | 8,7 (8.27–9.13) | 3.7 (2.47–4.93) | 5 (3.81–6.18) | .00003167 |
| QuickDash | 55.8 (48.15–63.45) | 34.1 (25.68–42.32) | 21.7 (12.35–31.08) | .08704 |
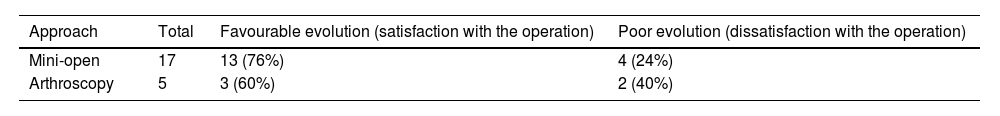
Some aspects of our study design and sample are disputable. One of the limitations of our study is having used two different types of approach in the sample analysis (mini-open [n = 17] vs. arthroscopy [n = 5]). Another limitation is not including having been operated on previously as an exclusion criteria of our patients. Exclusion of these patients was not made, since it was through this study and our experience with the technique that we learned and considered that the preservation of an unaltered anatomy could promote the use and favourable outcomes of this device. Analysing patients re-operated on with the primary surgery patients in the same patient group could have affected the sample and our outcomes.
Future perspectivesOne of the proposals of this intervention is that it would be low invasive. In their article, Gervasi et al.10 described a technique based on the implantation of a fluoroscopy-guided balloon spacer under local anaesthesia. With a 1.5 cm incision in the lateral arthroscopic portal, the device was inserted, assessing its correct positioning by scope. A mean time in surgery of 10 min was reported. No immediate complications with this technique were specified. As this was a low invasive procedure, it could be performed in the outpatient unit, with no need for hospital admission. This is an option to consider for future indications.
ConclusionThe outcomes obtained in our series after one year of follow-up are positive for the use of an InSpace®, type subacromial balloon spacer as a therapeutic option available for patients with irreparable RC tears. It may be used as a provisional procedure, delaying the need for more invasive surgery, or as a definitive method in patients who medically are non candidates for inverse arthroplasty. Seventy three per cent of patients included in the study expressed satisfaction with surgery. As explained in the discussion, it is important to be clear on the indications for this procedure to avoid making mistakes.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García Moreno J, Correa Bellido P, Salazar Aguilar JR, Pérez Correa JI, Montaner Alonso D, Rodrigo Pérez JL. Resultados tras la aplicación de balones espaciadores biodegradables como opción terapéutica en roturas masivas no reparables del manguito de los rotadores del hombro. Rev Esp Cir Ortop Traumatol. 2022;66:67–72.