Developmental dysplasia of the hip is the cause of approximately one third of secondary coxarthrosis. Anatomy alterations make it difficult to place a total hip prosthesis in its anatomical position and for it to be stable in the long term; there are several techniques to achieve this goal. In the present work, we used autograft of the femoral head (shelf graft or reinforced roof), to improve the coverage of the acetabular component with favourable results.
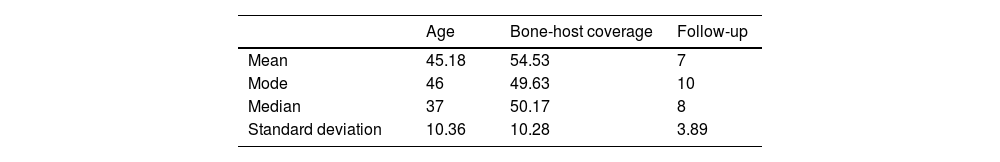
Materials and methodsSixteen cases were included in 14 patients with a diagnosis of developmental dysplasia of the hip (13 women and one man), the mean age was 44.3 years (range 35–68 years), with a mean follow-up of 7 years (range 1–15 years). All the cases were evaluated clinically and radiographically, to demonstrate the osseointegration of the graft and the functional results in the medium term.
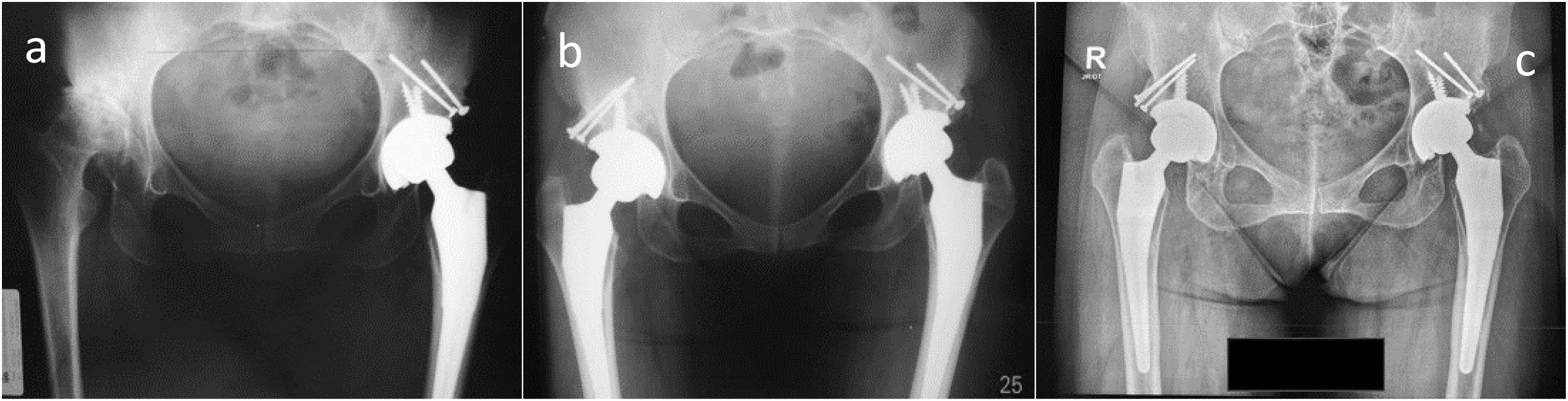
ResultsAll the acetabular components were placed in anatomical position (Ranawat technique), the mean percentage of host bone coverage was 54.53% (range 43.28–79.05%), obtaining additional coverage with the bone graft of 45.13%. Osseointegration of the graft of 100% at 12 weeks, resorption of the graft from the sixth month, stabilising in the third postoperative year. Only one case of dislocation is reported, no cases of infection, loosening, heterotopic ossification or revision.
ConclusionThis procedure has shown good functional results in the medium term with 100% osseointegration, despite cases of severe bone resorption of the graft that does not compromise the stability of the prosthesis.
La displasia del desarrollo de cadera es causante de aproximadamente un tercio de las coxartrosis secundarias. Las alteraciones de la anatomía dificultan la colocación de prótesis total de cadera en su posición anatómica, y que la misma sea estable a largo plazo; hay varias técnicas para lograr ese objetivo. En el presente trabajo utilizamos autoinjerto de la cabeza femoral (shelf graft o techo armado), para mejorar la cobertura del componente acetabular con resultados favorables.
Materiales y métodosSe incluyeron 16 casos en 14 pacientes con diagnóstico de displasia del desarrollo de cadera (13 mujeres y un varón), la edad media fue de 44,3 años (rango: 35-68 años), con un seguimiento medio de 7 años (rango: 1-15 años). Todos los casos fueron valorados clínica y radiográficamente, para demostrar la osteointegración del injerto y los resultados funcionales a mediano plazo.
ResultadosTodos los componentes acetabulares se colocaron en posición anatómica (técnica de Ranawat), el porcentaje medio de cobertura del hueso huésped fue del 54,53% (rango: 43,28-79,05%), obteniéndose una cobertura adicional con el injerto óseo del 45,13%. Osteointegración del injerto del 100% a las 12 semanas, reabsorción del injerto a partir del sexto mes, estabilizándose al tercer año postoperatorio. Solo se reporta un caso de luxación, ningún caso de infección, aflojamiento, osificación heterotópica o revisión.
ConclusiónEste procedimiento ha demostrado buenos resultados funcionales a medio plazo con osteointegración del 100%, a pesar de presentarse casos de reabsorción ósea severa del injerto que no compromete la estabilidad de la prótesis.
Developmental dysplasia of the hip (DDH) is one of the main causes of secondary coxarthrosis. Studies conducted in 1955 and 1978 reported that one third of cases of coxarthrosis are attributable to DDH. More recent studies report results similar to those mentioned previously, with an incidence between 30% and 40% of patients with coxarthrosis secondary to DDC.1–3
In adults, DDH has a worldwide prevalence between .1% and 12.8%, occurring more frequently in females.4–7 In Ecuador, there are no data on DDH in adults. However, a prevalence of 15.3% is reported in the population 3–6 months of age and 20% in children under 3 months of age.8,9 On the contrary, there is data on the prevalence of coxarthrosis in Ecuador, which is approximately 7.4%, so it can be inferred that DDH is the cause of 1.11–1.48% of all cases of coxarthrosis.10
DDH produces anatomical changes at the bone level and in soft tissues in the acetabulum and femur. There are multiple therapeutic options in the treatment of this pathology, from conservative treatment (analgesics, anti-inflammatories, physiotherapy and change in lifestyle) to surgical treatment through joint preservation surgeries (periacetabular osteotomies) or total joint replacement as definitive treatment.11 In cases of joint replacement, when the acetabular deficit does not allow coverage of at least 70% of the acetabular component, there are multiple alternatives that will allow the bone stock to be restored such as: maintaining the neoacetabulum with a high centre of rotation, placing the acetabular component in the paleoacetabulum in a medialised or protruded position (cotyloplasty); or placing the structural graft on the superolateral aspect of the acetabulum (shelf graft); We will focus on the latter for this study.11
The radiographic classifications most used in adult DDH are those of Crowe12 and Hartofilakidis,13 the former having more subjectivity, which is why it will be the one used for this study.
Finally, it will focus on patients with osteoarthritis secondary to DDH with Crowe type I, II and III, who underwent shelf graft with femoral autograft in cementless total hip arthroplasty where the osseointegration of the allograft and functional results will be assessed long term with an average follow-up of 7 years. The objective of the study is to demonstrate that the placement of a shelf graft to restore the bone stock in total hip arthroplasty in patients with DDH is a valid and technically reproducible therapeutic option, with low rates of bone graft resorption and loosening of the prosthetic components with good functional results in the medium term. This is the first study of its kind in Ecuador.
Material and methodsA retrospective study was carried out with patients diagnosed with coxarthrosis secondary to DDH, treated by cementless total hip arthroplasty with a shelf graft technique with femoral head bone autograft. Fourteen patients were included, representing a universe of 16 cases from May 2007 to June 2022 in Quito – Ecuador. Ninety-two percent of the patients were women, with a mean age of the sample of 46.6 years (σ=10.64; CI=41.9–52.3) (Table 1). Eighteen-point seventy-five percent of patients had previous surgeries, 33.33% had four unspecified surgeries on the affected hip, 33.33% had Chiari surgery, 33.33% had osteosynthesis due to a viciously consolidated proximal femur fracture. Follow-up was 15 years with an average of 7 years (σ=3.8; CI=5–9) (Table 1). The classification of Crowe and his study group12 was used, with 31.3% hips being type I, 25% type II and 43.7% type III. All patients were requested to have presurgical anteroposterior radiographs of the pelvis and axial hip, and computed axial tomography only in Crowe type III cases. All procedures were performed with the same surgical technique, using the posterolateral hip approach and in one case it was necessary to perform an osteotomy of the greater trochanter for the surgical approach. Presurgical planning was carried out in all cases. In 87.5% of cases the defect was superolateral and in 12.5% posterolateral, which determined the location of the bone graft at the defect site. The lack of acetabular coverage for the prosthetic component had a mean of 54.54% (σ=10.2; CI=49.1–60.02) (Table 1).
The definitive uncemented acetabular cups used were: one Smith&Nephew cup (London-United Kingdom), 7 Aesculap, Inc. cups (Pennsylvania-United States), 2 Quattro Grupe Lépine cups (Lyon-France) and 6 Zimmer-Biomet cups (Indiana-United States), with median diameter of 47mm. The head diameter was: 22mm (31.3%), 28mm (56.2%) and 32mm (12.5%). In all cases the femoral component was cementless.
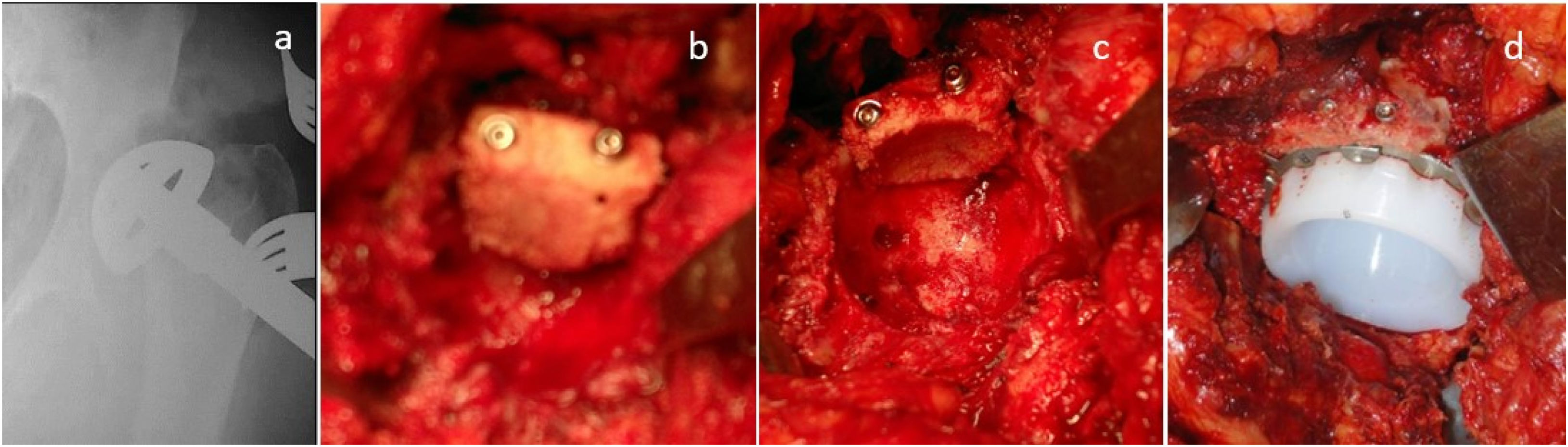
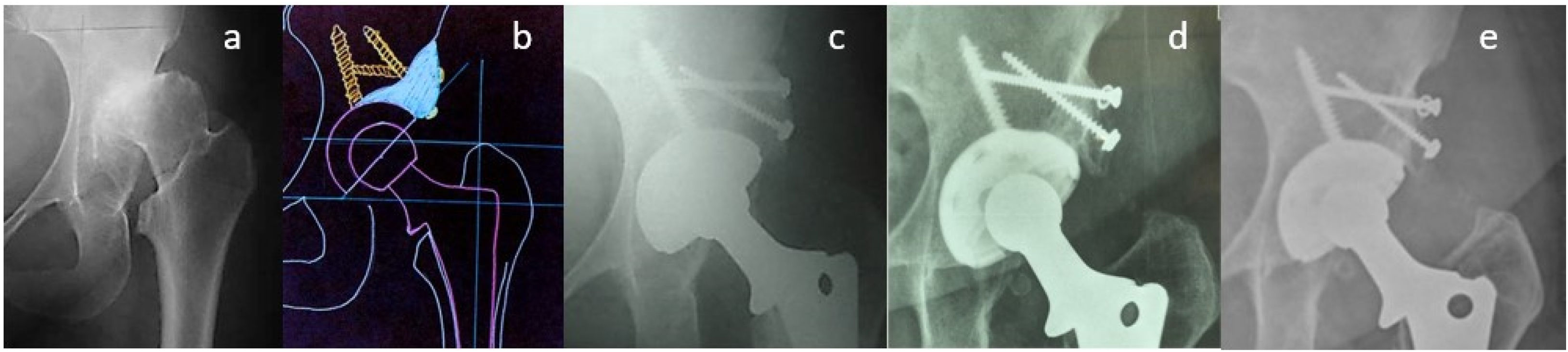
The surgical technique performed for the placement of a shelf graft is described below. First, the transverse ligament is identified as a parameter to locate the paleoacetabulum. Subsequently, the paleoacetabulum is reamed, trying to maintain the physiological centre of rotation of the hip up to the quadrilateral plate to determine the size of the acetabular cup and the acetabular defect. The bone graft, previously harvested and prepared, is then stabilised at the site of the acetabular bone defect using 4.0mm and 6.5mm cancellous screws. Subsequently, reaming is performed starting with the smallest acetabular reamer until adequate coverage of the acetabular cup is obtained. Intraoperative radiographic controls are performed to confirm adequate acetabular cup position. Finally, the final cup is placed 2mm larger than the drilling to obtain an adequate pressure fit (Fig. 1).
The acetabular cup was placed in the true acetabulum and the centre of rotation of the hip, it was restored to less than .5cm lateral and superior, up to 1cm is accepted as an adequate position. The inclination of the acetabular cup was with a median of 41.6° (σ=5.17; CI=38.3–43.8).
One of the cases presented an incomplete fracture at the calcar level during impaction of the femoral component treated with protective cerclage. Transverse subtrochanteric osteotomy was performed for femoral shortening due to limb discrepancy >4cm in two cases. Finally, joint replacement of the contralateral hip was performed in two cases, 5 days and 6 months after the first surgical intervention.
Hospitalisation time was a minimum of 3 days and a maximum of 9 days. The postoperative period began with walking with partial support (tiptoes) of the affected limb, with the help of two crutches from the second postoperative day for 6 weeks, then full support with the help of a crutch for 6 more weeks. All patients received low molecular weight heparin for 4 weeks as thromboprophylaxis.
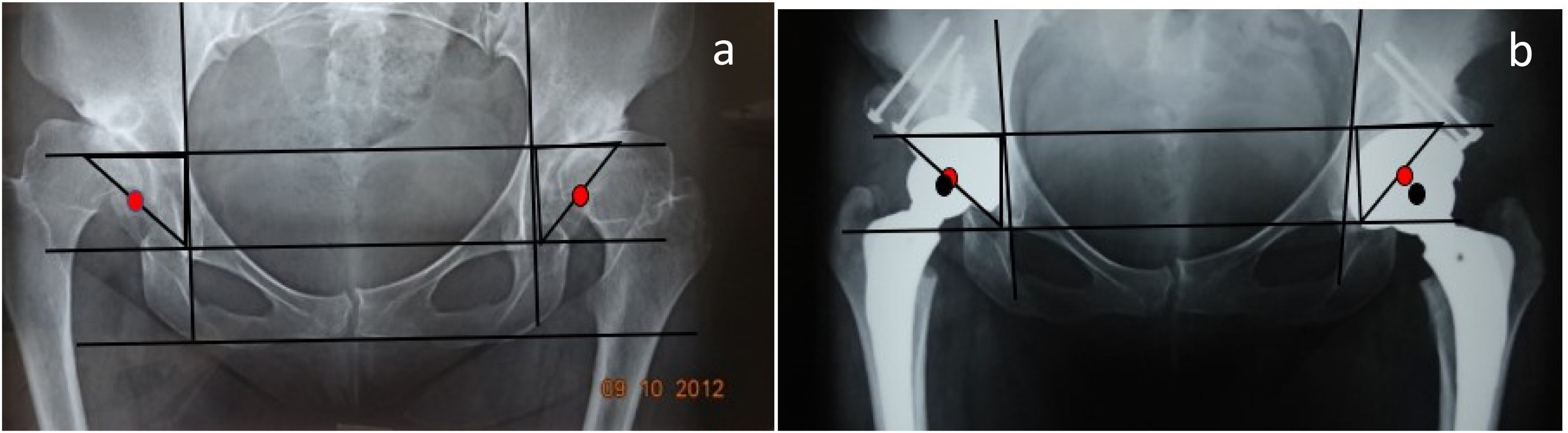
Postoperative follow-up was carried out after 2 weeks, for removal of stitches or staples. Clinical and radiographic controls were performed at 6 weeks, 3, 6, 9 and 12 months, with anteroposterior and lateral incidence. The method of Merle D’aubigne and Postel14 was used for clinical evaluation. In the initial and last control radiographs, the inclination of the cup was measured according to the Russotti and Harris method15 and the centre of rotation of the hip was assessed using the Ranawat technique and the Pagnano method16–18 (Fig. 2).
The incorporation and remodelling of the grafted bone was evaluated according to the method described by Knith.19,20 Rounding of the protruding edge of the graft beyond the cup or a change in graft density was considered an indicator of resorption, with mild resorption being established as radiolucency up to a third of the graft size, moderate up to half, and more than half as serious.
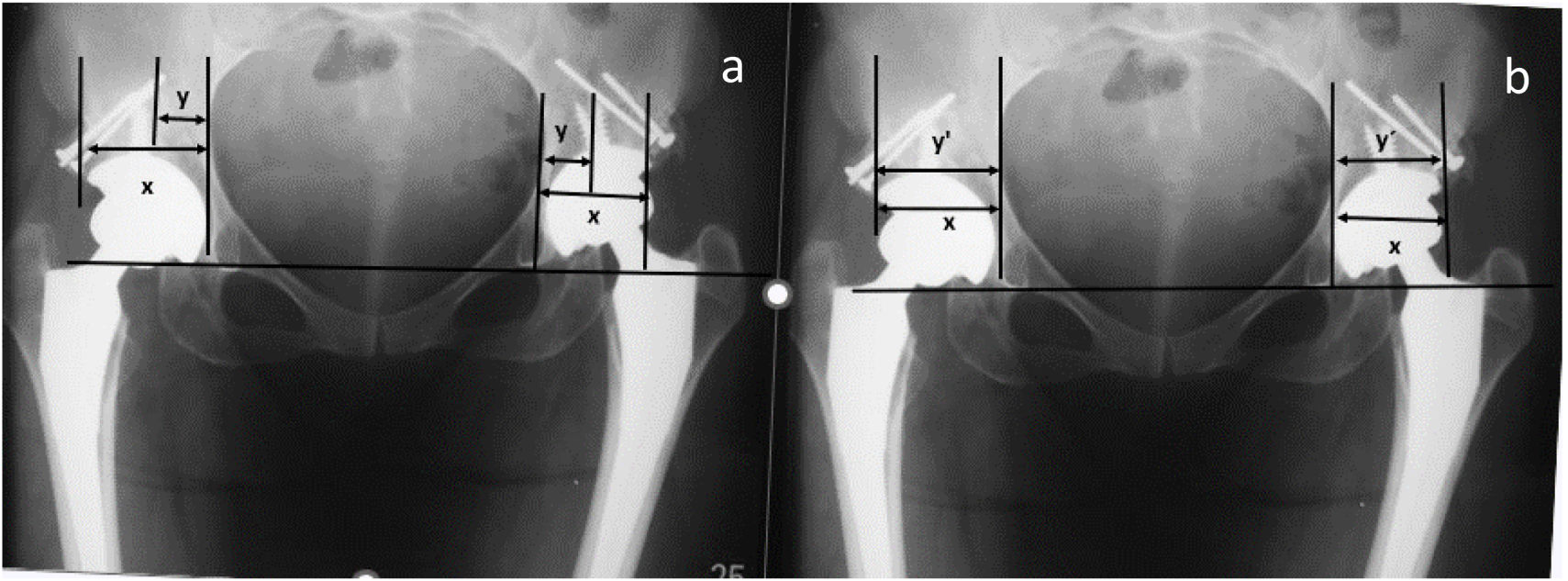
Radiographic signs of cup loosening and polyethylene wear were measured as described by Livermore et al.21 and DeLee and Chanrley,22 and the percentage of preoperative and postoperative coverage was evaluated as described by Ozden et al.23 (Fig. 3). Graft integration was considered when the bone–host–graft interface on the first radiographs could no longer be seen on the control radiographs (Fig. 4).
(a) Immediate postoperative radiograph, the percentage of coverage of the host bone for the cup is measured with the following formula: horizontal distance of the cup (X), the coverage of the host bone over the cup (Y) (Y/X)×100. (b) Last follow-up X-ray: we measure the horizontal distance of the cup (X), the bone coverage of the cup (Y′). The percentage of coverage gained is calculated as (Y′−Y)/X×100.25
(a) Preoperative radiography. (b) Immediate postoperative radiography. The black arrow points to the native bone and bone graft interface. (c) Postoperative radiography at 9 years. The black arrow indicates the continuity between the native bone and the graft, resorption is observed under the screw heads.
The variables studied were functional assessment according to Merle D’aubigne and Postel,14 additional bone coverage, osseointegration and bone resorption. The statistical method used is a Dummy variable model to transform the qualitative variables into quantitative variables. In addition, a Student's T model and Pearson coefficient were applied to determine the statistical validity of the surgical technique used in terms of the variables.
ResultsThe functional evaluation of Merle D’aubigne and Postel (pain, mobility and function) preoperatively had a mean of 8 (σ=.58; CI=8.4–9.6) and postoperatively of 16.75 (σ=.57; CI=16.4–17.06).
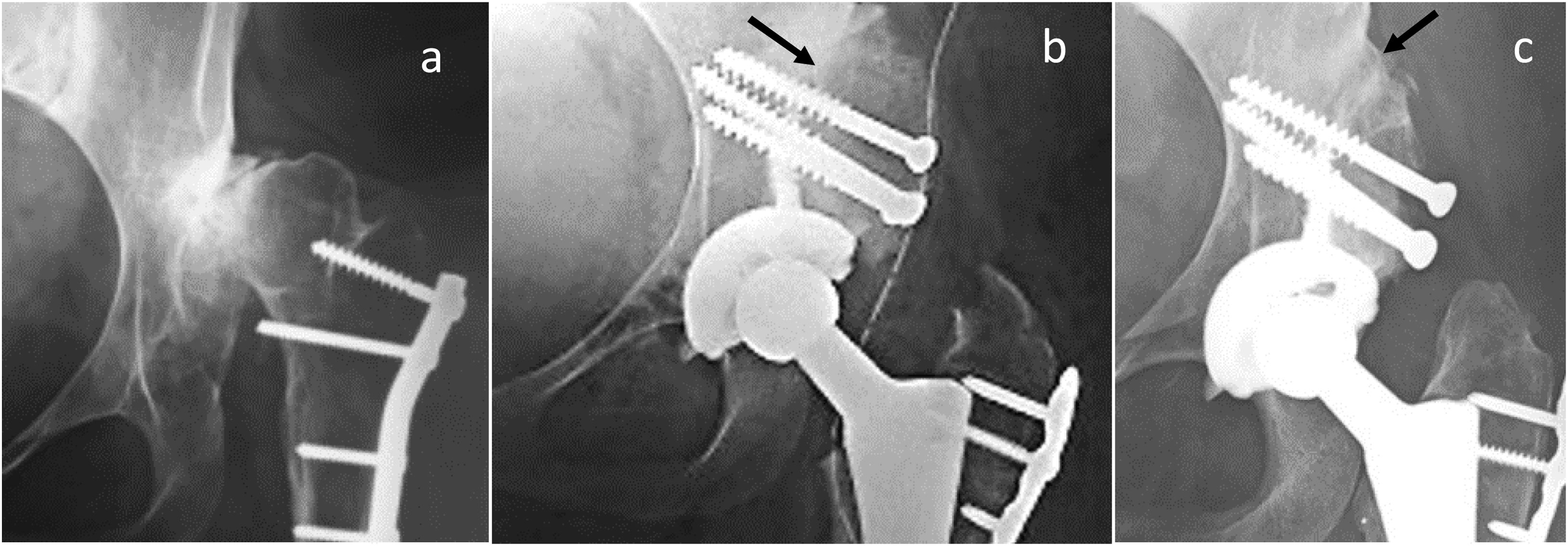
The percentage of cup coverage with host bone was an average of 54.54% and cup coverage with the graft was 45.13% (Fig. 5).
Graft integration was observed in all cases on average 12 weeks postoperatively according to the Knight method.19,20
Graft resorption occurred after the sixth postoperative month, mild in eight cases (50%), moderate in three (31.25%) and severe in five (18.75%), in an area in which the graft does not support load, without compromising the stability of the cup or need for revision, stabilising after 3 years (Fig. 6).
(a) Preoperative radiography. (b) Preoperative planning. (c) Immediate postoperative radiography performed acetabuloplasty with femoral head autograft. (d) Postoperative radiography at 3 years; the integration of the autograft on the cup can be identified. (e) Postoperative radiography at 15 years. It is observed that the bone resorption under the heads has been maintained compared to the image, no wear of the polyethylene is seen.
In 12.5% of cases, transverse subtrochanteric osteotomy was performed with average consolidation 6 months postoperatively.
There were no cases of implant loosening or polyethylene wear that justified revision surgery. No case of infection was reported, the length of the extremities was restored, the result being less than .5cm of discrepancy as the largest difference. No case of heterotopic ossification or neurological injury was observed either. One case of prosthetic dislocation was reported, requiring open reduction for this reason.
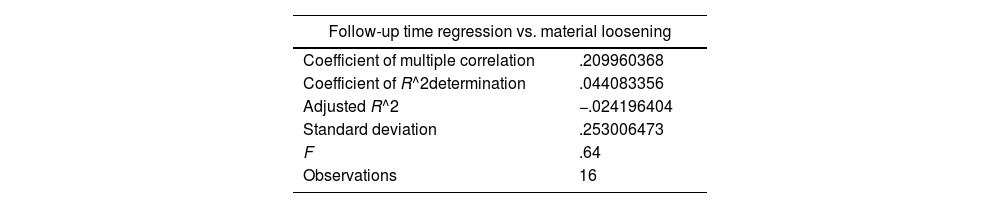
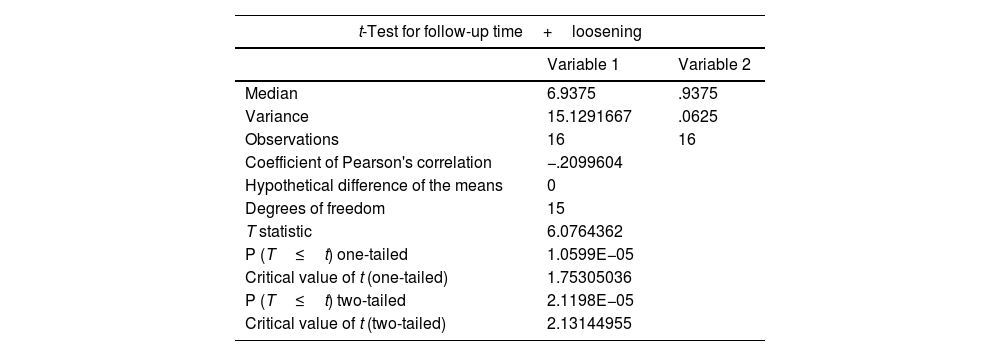
The variables were crossed between follow-up time and material loosening by applying Dummy variables, establishing a direct relationship between the two variables, which allows us to infer that the longer the follow-up time, the greater the osseointegration (Table 2).
Summary of statistics for crossing variables between monitoring time and material loosening.
| Follow-up time regression vs. material loosening | |
|---|---|
| Coefficient of multiple correlation | .209960368 |
| Coefficient of R^2determination | .044083356 |
| Adjusted R^2 | −.024196404 |
| Standard deviation | .253006473 |
| F | .64 |
| Observations | 16 |
In addition, the Pearson coefficient was obtained, which indicates an inversely proportional relationship between the two variables, that is, the greater the passage of time, the lower the rate of graft failure (Table 3).
Summary of t test of two paired variables.
| t-Test for follow-up time+loosening | ||
|---|---|---|
| Variable 1 | Variable 2 | |
| Median | 6.9375 | .9375 |
| Variance | 15.1291667 | .0625 |
| Observations | 16 | 16 |
| Coefficient of Pearson's correlation | −.2099604 | |
| Hypothetical difference of the means | 0 | |
| Degrees of freedom | 15 | |
| T statistic | 6.0764362 | |
| P (T≤t) one-tailed | 1.0599E−05 | |
| Critical value of t (one-tailed) | 1.75305036 | |
| P (T≤t) two-tailed | 2.1198E−05 | |
| Critical value of t (two-tailed) | 2.13144955 | |
These results establish that the surgical technique described is a procedure with favourable results in the medium term, with osseointegration in all cases and no cases of bone graft failure observed over time.
DiscussionDDH is a pathology that, despite having received adequate treatment, has high rates of secondary coxarthrosis at an early age, presenting pain, functional limitation, shortening and lame gait, which will limit activities of daily living. The definitive treatment in these cases is total hip arthroplasty, the procedure of which represents a challenge for cirujanos.24,25
In this technique, the femoral head can be used, as an autologous graft or allograft, to increase bone stock.26
The first study that reported favourable results with this technique was described in 1978, where 22 hips were included with excellent results, contraindicating the procedure in patients with rheumatoid arthritis and other causes of osteopenia.27
It is important to restore the centre of rotation of the hip in its anatomical location, placing the cup in the true acetabulum,4 although good results were obtained with a high centre of rotation of the hip.23
Hampton and Harris in 2006 conducted a study, where they included nine patients with an average follow-up of 16 years, and demonstrated a success rate of 92% maintaining the high centre of rotation. However, lameness and septic loosening are a prevalent problem to take into accoun.28
In 2009 Nousiainen et al., with 25 patients with DDH, reported that there was osseointegration in 93% of the cases. There was no displacement of the graft, in 71% of the cases there was resorption of less than a third and in the remaining percentage there was resorption of a third halfway through the graft, of which only two patients required bone graft revision, concluding that it is a technique with effective results.29
Ozden et al. in 2018 reported a study where they included 38 dysplastic hips in 31 patients, with a follow-up of 20.3 years on average; reporting a prosthesis survival of 66%. No revision was performed due to graft resorption, regardless of the position of the centre of rotation.23
Yeganeh and his study group in 2018 reported a short-term prosthesis survival rate of 100% with an improvement in the functional scale from 35.50±9.11 preoperative to 95.10±4.71 postoperative, concluding that it is an accessible and feasible strategy.30
Acetabuloplasty with bone autograft of the femoral head with cementless acetabular components has proven to be a technique with good results in the short and medium term, and bone stock is also improved if revision surgery is necessary.
The results obtained in this study are very similar to those described in world literature. It is recommended to restore the centre of rotation of the hip and place the acetabular component in the paleoacetabulum to reduce the possibility of early loosening and improve the survival of prosthetic implants.
ConclusionsTotal hip arthroplasty with a shelf graft in patients with DDH is a procedure that represents a functional improvement of 8.75 points in relation to pain, mobility and function.
An additional coverage with the bone graft of 45.13% was achieved. In addition, the integration of the graft at 14 weeks was 100%, with a resorption of the graft at the sixth month in a mild form in 8 cases (50%), moderate in 3 (31.25%) and severe in 5 (18.75%), stabilising after 3 years, without compromising the stability of the prosthesis in any of the cases.
Finally, a reintervention (open reduction) for prosthetic dislocation is reported, with a rate of infection, neurological injury and heterotopic ossification of 0% and no revision surgery.
This study allows us to assert that this procedure has good results in the short and medium term, despite the existence of bone resorption of the autograft and with no compromising of stability and with low complication rates.
Level of evidenceLevel of evidence III.
FundingNone declared.
Conflict of interestsThe authors declare that they have no conflicts of interest in the preparation of this article. They also declare that they have complied with all the ethical and legal requirements necessary for publication.