Acetabular revision surgery is a surgical challenge, especially when complex bone defects appear. This makes primary fixation and osseointegration of the implants difficult, which conditions the appearance of complications. Trabecular titanium implants attempt to solve these problems.
ObjectivesTo evaluate our clinical-radiological results, the survival of the implants and the appearance of mid-term complications in acetabular revision surgery in a series of 37 acetabular replacements with Paprosky type IIIA and IIIB bone defects in which a trabecular titanium Cup-Cage revision implant was used.
Material and methodWe conducted an observational, descriptive and retrospective study of 37 cases with complex acetabular defects (20 type IIIA and 17 type IIIB, five of them with pelvic discontinuity) in which the acetabular component was replaced by trabecular titanium cups between 2011 and 2019. We analysed clinical results (pain and functionality) and radiological parameters (restoration of the hip rotation centre and the mobilisation of the implants), as well as the appearance of complications.
ResultsThe mean follow-up was 61 months. We obtained a median improvement of 8 points on the Merlé D’Aubigné-Postel functionality scale and 6 points on the VAS scale of pain perceived by the patient. We recorded two cases of acetabular loosening, one case of dislocation and three surgical wound infections without affecting the implant.
ConclusionsThe use of trabecular titanium Cup-Cage implants could be a valid option in acetabular revision surgery with complex acetabular defects, presenting good clinical and radiological results and in terms of complications and survival of the implants, mainly due to their good primary fixation and subsequent osseointegration.
La cirugía de revisión acetabular supone un reto quirúrgico, sobre todo cuando aparecen los defectos óseos complejos, pues dificultan la fijación primaria y osteointegración de los implantes, lo que condiciona la aparición de complicaciones. Los cotilos de titanio trabecular intentan solventar estos problemas.
ObjetivosValorar los resultados clínico-radiológicos, la supervivencia de los implantes y aparición de complicaciones a medio plazo en cirugía de revisión acetabular en una serie de 37 recambios acetabulares con defectos óseos tipo IIIA y IIIB de Paprosky en los que se utilizó un implante de revisión tipo cup-cage de titanio trabecular.
Material y métodoRealizamos un estudio observacional, descriptivo y retrospectivo de 37 casos con defectos acetabulares complejos (20 tipo IIIA y 17 tipo IIIB, cinco de ellos con discontinuidad pélvica), en los que se realizó recambio del componente acetabular por implantes de titanio trabecular entre los años 2011 y 2019. Analizamos resultados clínicos (dolor y funcionalidad) y parámetros radiológicos (restauración del centro de rotación de la cadera y la movilización de los implantes), así como la aparición de complicaciones.
ResultadosEl seguimiento medio fue de 61 meses. Obtuvimos una mejoría en la mediana de ocho puntos en la escala de funcionalidad de Merlé D’Aubigné-Postel y de seis puntos en la escala EVA de dolor percibido por el paciente. Registramos dos casos de aflojamiento acetabular, un caso de inestabilidad y tres infecciones de herida quirúrgica sin afectar al implante.
ConclusionesLa utilización de implantes tipo cup-cage de titanio trabecular podría constituir una opción válida en cirugía de revisión acetabular con defectos acetabulares complejos, presentando buenos resultados clínico-radiológicos y en cuanto a complicaciones y supervivencia de los implantes, debido a su buena fijación primaria y osteointegración.
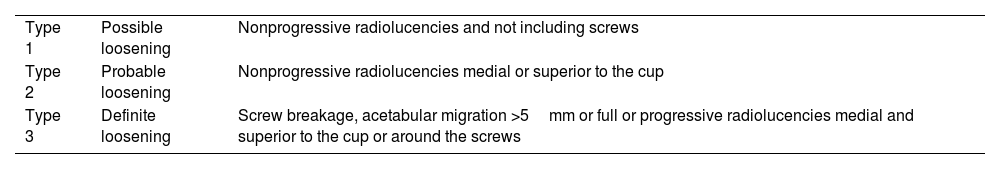
The number of revision surgeries after hip arthroplasty is expected to increase by 137% between 2005 and 2030.1 This type of surgery poses a challenge for the surgeon, especially when complex or major acetabular defects appear, i.e., those where there is less than 50% acetabular coverage and which therefore require the use of implants to guarantee their stability until osseointegration (Table 1).2,3 Likewise, the large loss of bone stock will make it difficult to restore the hip centre of rotation.4
Paprosky classification of acetabular defects.1,2
| Type | Subtype | Migration | Defect |
|---|---|---|---|
| I | No | Ring, roof, columns intactIn contact with host bone >90% | |
| II | <2cm | CavitaryIn walls, with columns intactContact >50% | |
| A | Superomedial | Tectal | |
| B | Superolateral | Superolateral ring | |
| C | Medial | Medial wall | |
| III | >2cm | Walls and columns | |
| A | Superolateral | Ring of 10 to 2Contact 40%–50% | |
| B | Superomedial | Ring of 9 to 5Contact <40%Pelvic discontinuity could be associated | |
Several techniques have been described to treat complex acetabular defects. Sloof et al.5 propose the use of cancellous bone graft to fill the defect on which the polyethylene cup is directly cemented; on the other hand, rings (such as those designed by Müller and Ganz)6,7 and anti-protrusion cages (such as the Burch–Schneider)6,7are used, also combined with both structural and cancellous graft and fixed to the pelvis with the aim of redistributing the load towards the pelvis and thus protect the bone graft. In both cases, a polyethylene insert is also cemented inside the revision component. 6 Both techniques have the disadvantage of not achieving biological fixation or osseointegration of the implant, and are associated with a high percentage of complications, the most important being loosening of components in the medium and long term, between 10% and 40% according to some series.6–8
Other techniques that have fallen into disuse due to their high rates of loosening and instability when used in major acetabular defects include elevation of the hip rotation centre and the use of oblong or bilobed cups.6,9
In an attempt to solve these problems, acetabular implants coated with highly porous metals, mainly trabecular titanium and tantalum, have been designed. These metals are structurally similar to cancellous bone and have higher porosity, coefficient of friction, and osteoconductive capacity compared to conventional components and a modulus of elasticity similar to native bone, giving them ideal osteoconductive characteristics. All this contributes to the biological fixation of implants.10,11 Furthermore, despite the differences between the two metals, both have demonstrated good results.4,12–14
The Cup-Cage acetabular revision system combines the advantages of anti-protrusion cages and trabecular metal. On the one hand, they allow screwing to the pelvis, favouring primary mechanical stability, and their being porous metal-coated cups also favours their osseointegration.4,12,14
The objective of this study was to analyse the medium term clinical and radiological outcomes, implant survival, and complications that we obtained in a series of patients with Paprosky type IIIA and IIIB acetabular defects operated using the Cup-Cage trabecular titanium acetabular revision system.
Material and methodWe conducted an observational, descriptive, and retrospective study of 37 cases with a diagnosis of Paprosky type IIIA and IIIB acetabular defect in 34 patients undergoing surgery at our centre between 2011 and 2019 with the Delta-Revision TT Cup-Cage trabecular titanium acetabular implant (Lima Corporate® Udine, Italy).
The Delta-Revision TT implant is an acetabular component covered in trabecular titanium with three upper extensions in the form of wings that are screwed to the ilium and a lower wing that is attached to the obturator hole to improve primary stability. Augmentations of the same material can be screwed to this implant to fill possible acetabular defects. It also offers the possibility of placing internal modules to increase the offset and improve the tension of the soft tissues, thus avoiding abduction apparatus failure. In the same way, it allows for the placement of flanges of up to 20° that improve acetabular orientation, thus decreasing the risk of dislocation. Finally, it aids the possibility of placing dual mobility heads that improve joint stability and further reduce the risk of dislocation.13
Several classification systems for acetabular defects have been proposed; the Paprosky classification is one of the most widely used (Table 1).2,3 Using this classification we consider complex defects to be type IIIA (superolateral migration >2cm) and IIIB (superomedial migration >2cm).
In our study acetabular defects were classified preoperatively by radiological study and computed tomography (CT) and corrected intraoperatively if there was variability. We found a total of 20 IIIA (54%) and 17 IIIB (46%) defects. Five (29%) of the type IIIB had pelvic discontinuity.
The mean age of the sample was 67.4 years (43–89 years, SD 12.03); 10 patients (29.5%) were male and 24 female (70.5%). The mean body mass index (BMI) was 27.15kg/m2 (18–41kg/m2, SD 5.7). Two patients had bilateral defects (5.8%).
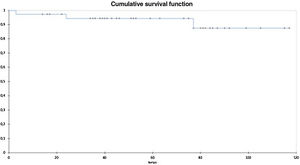
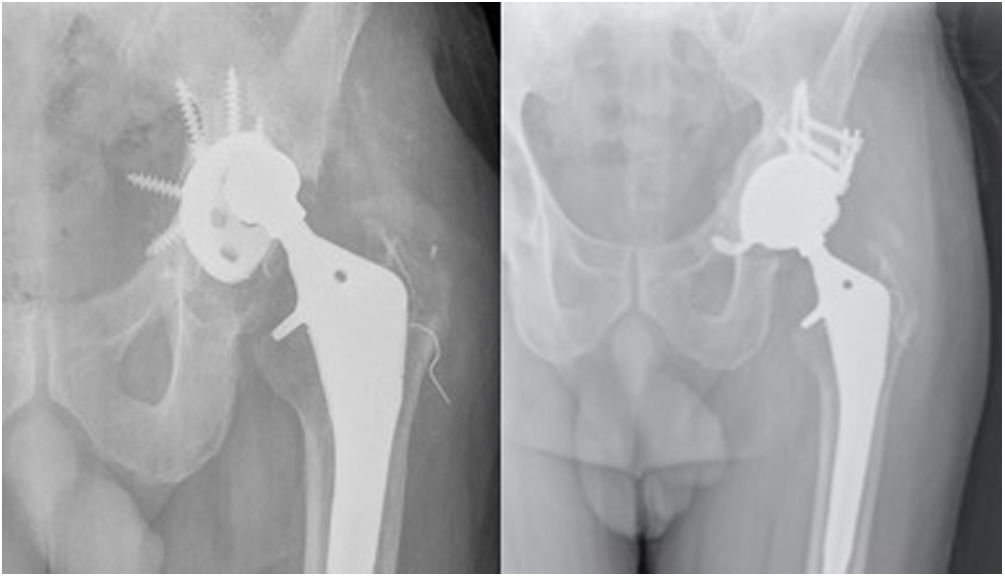
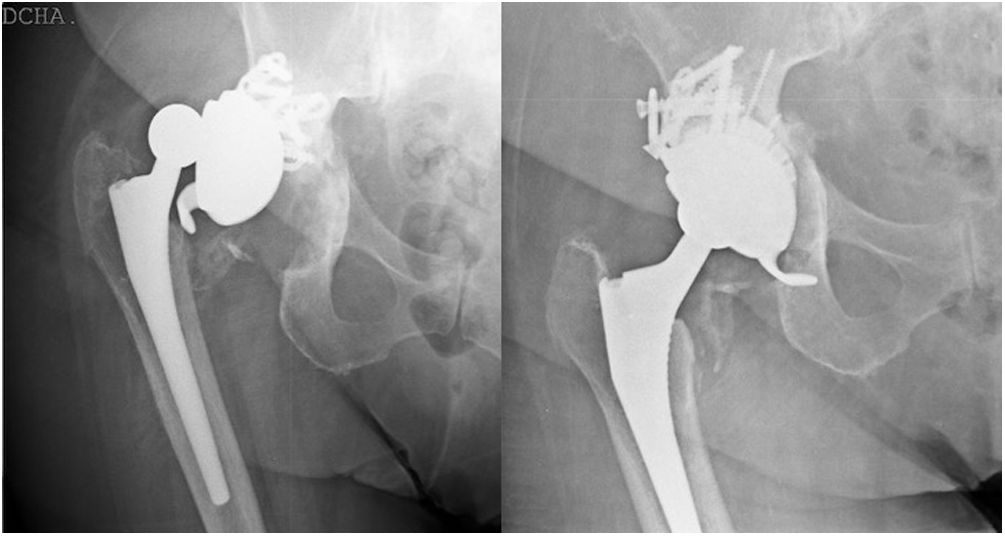
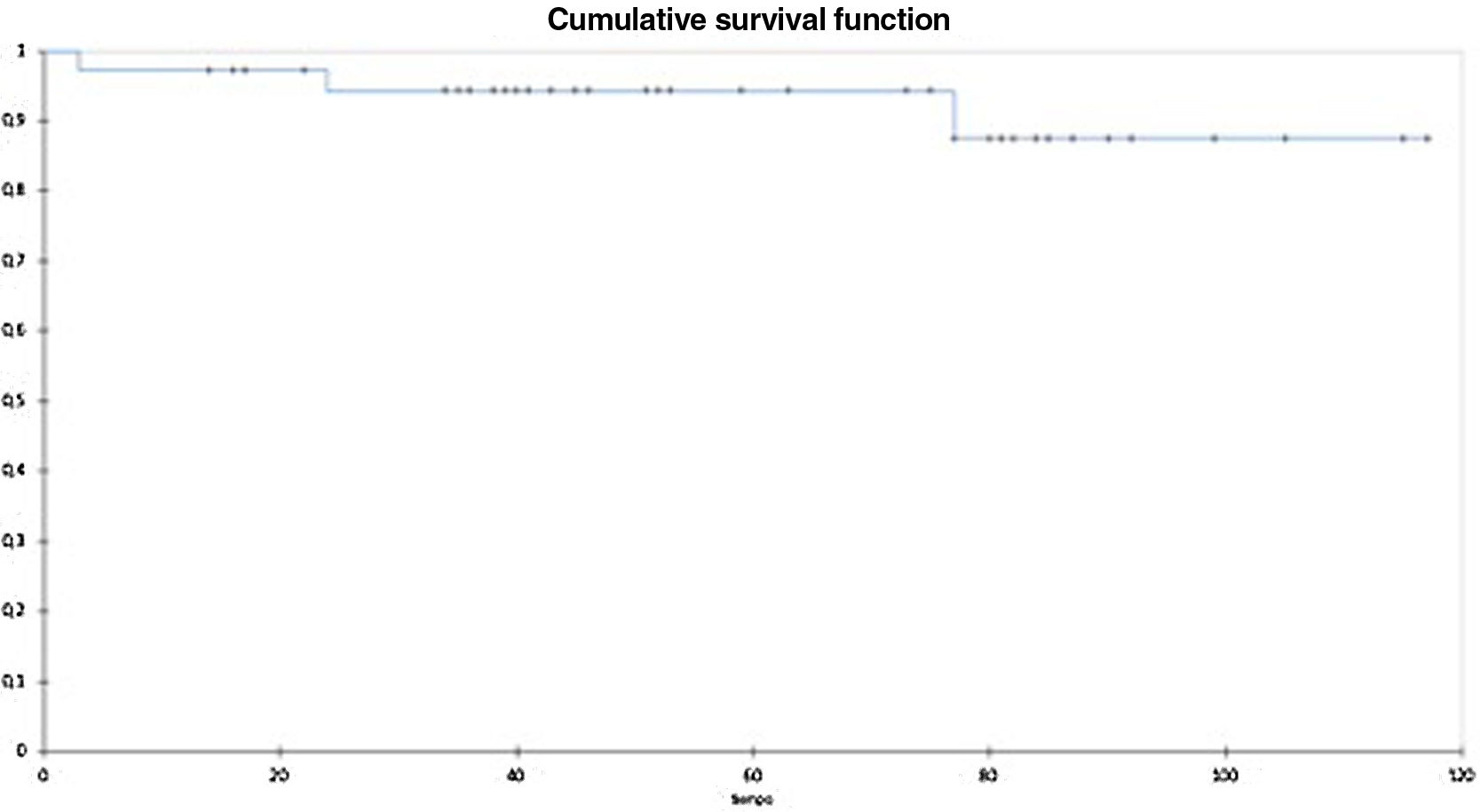
The most frequent cause for which acetabular revision surgery was indicated was aseptic loosening of primary prostheses in 26 cases (70.3%) (Figs. 1 and 2), followed by second stage treatment of prosthetic infection in four cases (10.8%) and recurrent dislocation in four cases (10.8%) in which a severe acetabular defect was observed at the time of removal of the primary implant. Other reasons for revision were insert wear in two cases (5.4%) resulting in osteolysis around the implant, and osteosynthesis failure (2.7%) which had resulted in significant acetabular erosion.
(A) X-ray of a patient diagnosed with aseptic loosening of the left hip acetabular component with Paprosky type IIIA acetabular defect. (B) X-ray control three years after surgery to replace the acetabular component with a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]). TT: TRABECULAR titanium.
(A) X-ray of a patient diagnosed with aseptic loosening of right hip acetabular component with Paprosky type IIIB acetabular defect associated with pelvic discontinuity. (B) Control X-ray at two years after revision of the cup to a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]). TT: trabecular titanium.
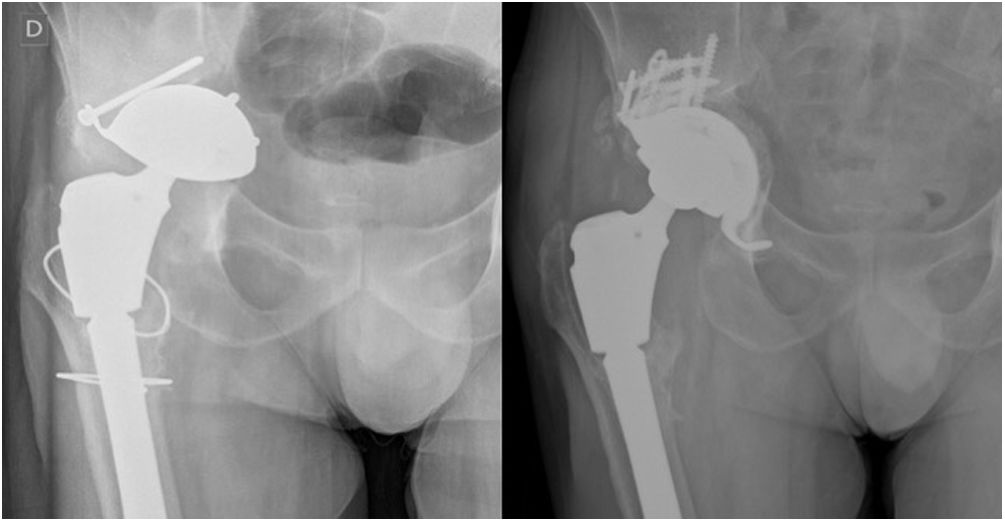
The same surgical team operated on all the patients. The posterolateral approach was used in all cases. Tissue bank cancellous bone allograft chips were used in all the surgeries (Fig. 3A). In 11 cases (29.7%) it was necessary to combine structural allograft fixed with cannulated screws and in one case (2.7%) to supplement with trabecular metal (Fig. 4). In one of the cases with pelvic discontinuity, a neutralisation plate was also used in the posterior column to provide greater stability to the assembly (Fig. 3). A dual-mobility system was used in all cases.
(A and B) Intraoperative images of a patient with a Paprosky type IIIB acetabular defect associated with pelvic discontinuity for which cancellous allograft was used to fill the defect and a posterior spinal stabilisation plate (A) associated with a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]) (B). TT: trabecular titanium.
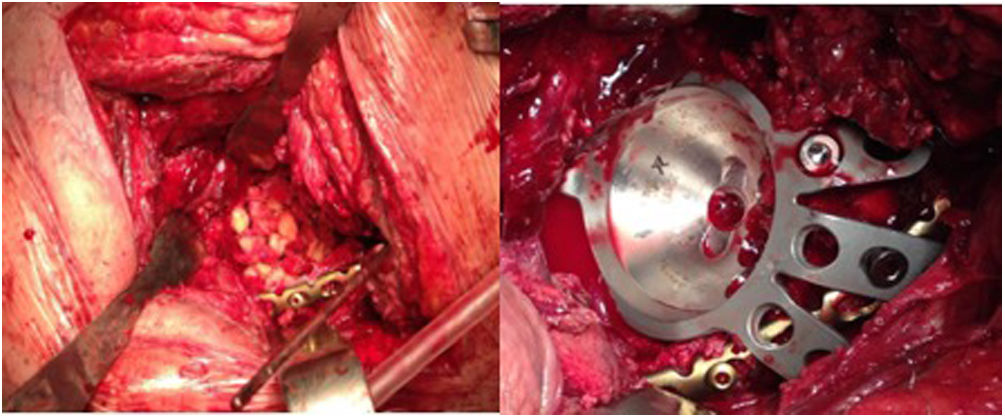
(A) Control X-ray of a patient one month after placement of a trabecular titanium cup (Delta-Revision TT [Lima Corporate®]) showing early loosening of the implant. (B) Radiographic control at six months after replacement of this component with a new revision cup (Delta-Revision TT [Lima Corporate®]) modifying the acetabular orientation and combining increased trabecular titanium in the tectal region. TT: trabecular titanium.
The protocol for a return to walking followed by our patients consisted of keeping the operated limb non-weight bearing for the first month to protect the graft and favour its integration, followed by progressive partial weight bearing until the 12th week, and full weight bearing thereafter.
We assessed the patients clinically and radiologically, preoperatively, and postoperatively at one month, three months, six months, one year, and then annually.
Clinical assessment involved measuring patient-perceived pain, using a visual analogue scale (VAS),15 and function, measured using the modified Merlé D’Aubigné-Postel scale.16
The radiological results were analysed by taking anteroposterior (AP) X-rays of the pelvis and axial X-rays of the operated hip. We assessed the restoration of the hip centre of rotation at the first postoperative radiographic control following the method of Ranawat et al.,17,18 and the presence of acetabular loosening according to Gill's criteria, which includes the appearance of radiolucencies around the screws or the acetabular cup, screw breakage, and implant migration >5mm (Table 2).19 These data were taken at the last available radiological test of each patient.
Gill's criteria for acetabular component loosening.19
| Type 1 | Possible loosening | Nonprogressive radiolucencies and not including screws |
| Type 2 | Probable loosening | Nonprogressive radiolucencies medial or superior to the cup |
| Type 3 | Definite loosening | Screw breakage, acetabular migration >5mm or full or progressive radiolucencies medial and superior to the cup or around the screws |
We recorded complications that arose during follow-up and the need for reoperation for any cause.
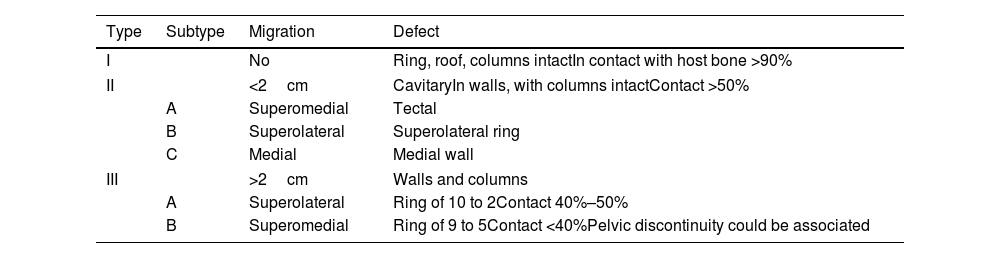
SPSS 22 (IBM, Chicago, IL) was used for the statistical analysis. Continuous quantitative variables were described by mean and standard deviation (SD), discrete quantitative variables by mean and median, nominal qualitative variables by absolute frequencies, and ordinal qualitative variables by median. The parametric Student Fisher t-test was used for the statistical analysis of variables with a normal distribution, and the non-parametric Mann–Whitney U-test was used for variables that did not follow a normal distribution. The Kaplan–Meier method was used to assess cumulative survival rate, considering the need for revision of the acetabular component for any cause as the final event. The level of statistical significance was set at 5%. This study was approved by our centre's Medicines Research Ethics Committee (CEIm), registration number 32/21.
ResultsThe mean follow-up time was 61 months (14–117 months, SD 29.04). Two losses to follow-up (5.8%) were recorded, due to non-revision surgery-related deaths, both patients had Paprosky type IIIA acetabular defects.
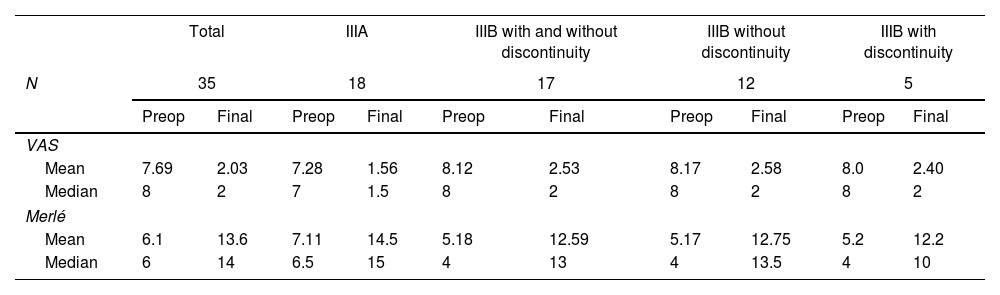
Clinical resultsWith regard to functional assessment measured with the modified Merlé D’Aubigné-Postel scale, the overall results improved from a median of 6/18 points before surgery (mean 6.1/18) to a median of 14/18 points at the end of follow-up (mean 13.6/18); this difference was statistically significant (p=.000). The median improvement was from 1/6 to 5/6 in the pain section (mean improvement from 1.63 to 4.63) (p=.000), from 2/6 to 5/6 in mobility (from 2.2 to 4.69 if we calculate the mean) (p=.000), and from 2/6 to 5/6 in ambulation (from 2.34 to 4.26 if we calculate the mean) (p=.000).
With regard to patient-reported pain assessment, we obtained an improvement from a median of 8 points on the VAS scale pre-surgery (mean 7.69) to a median of 2 (mean 2.03) at the last check-up consultation (p=.000).
If we divide our sample between those with Paprosky type IIIA and IIIB acetabular defects, we obtain worse values for pain and function in those with type IIIB defects, although these differences are not statistically significant (p=.078 for pain and p=.095 for function) (Table 3).
Functional outcomes (mean and median) before surgery and at the end of follow-up in terms of pain measured with the VAS scale and function measured with the modified Merlé D’Aubigné Postel scale.
| Total | IIIA | IIIB with and without discontinuity | IIIB without discontinuity | IIIB with discontinuity | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | 35 | 18 | 17 | 12 | 5 | |||||
| Preop | Final | Preop | Final | Preop | Final | Preop | Final | Preop | Final | |
| VAS | ||||||||||
| Mean | 7.69 | 2.03 | 7.28 | 1.56 | 8.12 | 2.53 | 8.17 | 2.58 | 8.0 | 2.40 |
| Median | 8 | 2 | 7 | 1.5 | 8 | 2 | 8 | 2 | 8 | 2 |
| Merlé | ||||||||||
| Mean | 6.1 | 13.6 | 7.11 | 14.5 | 5.18 | 12.59 | 5.17 | 12.75 | 5.2 | 12.2 |
| Median | 6 | 14 | 6.5 | 15 | 4 | 13 | 4 | 13.5 | 4 | 10 |
Final: value at the end of follow-up; Merlé: modified Merlé D’Aubigné-Postel scale; N: hips included in the study after ruling out losses to follow-up due to causes unrelated to revision surgery; Preop: preoperative value; VAS: visual analogue scale.
Similarly, if we compare the results distinguishing the IIIB defects that are associated with pelvic discontinuity from those that are not, we obtain better functional results in those that do not have discontinuity, although without reaching statistical significance (p=.815). In this case, however, we did not observe differences in terms of patient-perceived pain in either group (Table 3).
Radiological resultsIn terms of radiological results, we obtained restoration of the hip centre of rotation in 30 cases (85.7%) according to the criteria of Ranawat et al.17,18 measured on postoperative X-ray. We recorded two cases (5.7%) of acetabular implant migration of >5mm, compatible with aseptic loosening according to Gill's criteria.19 One of these was observed at the first check-up one month after surgery and the other was a late loosening by the sixth year of follow-up. We found no other cases of migrations greater or less than 5mm, radiolucency, or implant breakage during follow-up.
ComplicationsWe recorded one episode (2.8%) of prosthetic dislocation without previous trauma due to suboptimal position of the revision cup (6° anteversion) and gluteal muscle weakness, which was resolved by changing the internal acetabular modularity with an insert with an offset +5mm and a 20° flange to prevent posterior dislocation. Two cases of aseptic loosening were reported (5.7%). The first had an acetabular defect IIIB without pelvic discontinuity and was resolved by replacing the component with a new revision cup (Delta-Revision TT) and adding a trabecular titanium module in the tectal region (Fig. 4). The second case was a more complex case, as it had a type IIIB acetabular defect associated with a pelvic discontinuity. This case was also replaced with a new Delta-Revision TT cup. However, the result was not satisfactory, as there was an episode of atraumatic dislocation, probably secondary to abductor apparatus weakness as a consequence of the successive surgeries, therefore it was necessary to reintervene, this time to adjust the internal modularity. Despite this, the instability persisted, making it necessary to perform a Girdlestone resection arthroplasty. Minor complications included three cases (8.5%) of superficial surgical wound infection, which were resolved with antibiotics administered orally without complications.
SurvivalKaplan–Meier curve analysis for revision of the acetabular component for any cause identified the cumulative survival at 5 years at 94.3% CI, 86.5%–100% and at 100 months at 87.5% CI, 72.9%–100% (p<.05) (Fig. 5).
DiscussionIn the case of Paprosky's type I and II acetabular defects, in which contact of the implants with the host bone is greater than 50%, the use of hemispherical porous metal acetabular components screwed together,20,21 combined or not with grafting or trabecular metal augmentations,12,22 is sufficient to obtain good primary fixation and biological integration of the components. In the case of Paprosky type IIIA and IIIB acetabular defects, in which the acetabular bone stock is less than 50%, other more stable fixation systems are necessary.4,12,14,23,24 Of the many options available for the treatment of major acetabular defects,12,23Cup-Cage type systems are of choice in our centre and the subject of the present study, combining an anti-protrusion cage system that facilitates primary stability and a trabecular metal-coated cup that favours biological fixation of the implant. Their usefulness has also been demonstrated in cases of pelvic discontinuity, acting as internal fixation between the upper and lower hemipelvis.4,12–14
In our study, we observed significant improvement in functional results according to the Merlé D’Aubigné Postel test, with an improvement of 7.5 points from a mean of 6.1 points preoperatively to 13.6 points at the last check-up. Similarly, Gallart et al.13 also show a significant improvement from a mean preoperative score of 11.1 to 16.6 postoperatively. The higher preoperative and postoperative score obtained in the study by Gallart et al.13 can be explained by the inclusion of both simple and complex acetabular defects, and a better clinical situation of the patients before and after the operation is predictable. The author himself states in his work that the only variable associated with the need for new surgery is the degree of previous acetabular defect. Similarly, in our study we found worse functional results in the cases with a greater degree of acetabular defect.
Along the same lines, Steno et al. report significant improvement in functional outcomes, only evaluating the sections of ambulation and pain, with a mean score of 4.7/12 points preoperatively to 9.8/12 points postoperatively. These results are comparable to those presented in our series if we evaluate the same sections as Steno et al., obtaining an improvement from a mean of 3.9 to 8.9/12 points at the last control.25
In terms of radiological results, by applying the method of Ranawat et al.17 we restored the hip centre of rotation in 85.7% of cases, similar to the 79.4% obtained by Abolghasemian et al.26 in a study on the use of trabecular metal augmentations associated with Cup-Cage implants in the treatment of acetabular defects. Torres-Campos et al.27 reported a 61.19% restoration of the centre of rotation using a Burch-Schneider ring combined with bone grafting. According to the available literature,27 restoration of the anatomical centre of the hip is of great importance in both primary and revision arthroplasty, since reproducing the anatomy and biomechanics of the native hip reduces demands on the implant, positively affecting both the functional results and the survival of the prosthesis.
One of the main advantages of Cup-Cage systems is their superior osseointegration due to trabecular metals, either tantalum or trabecular titanium. In this direction, Villanueva et al.28 in a review on the treatment of pelvic discontinuities conclude that the cause of implant loosening is more a failure of biological integration than a primary fixation problem. Similarly, Beckmann et al.8 demonstrated in a systematic review the superiority of trabecular metal over classic anti-protrusion systems in all types of acetabular defects, but especially in those of greater severity (Paprosky's IIIA and IIIB) and in the presence of pelvic discontinuity, showing lower annual rates of loosening. In our series we obtained a loosening rate of 5.7% with a mean follow-up of five years, comparable with the existing literature. This is the case of Banerjee et al.,11 who in a systematic review published aseptic loosening rates of tantalum implants of less than 10% in studies with an average follow-up of more than five years or Del Gaizo et al.29 who reported loosening rates of 2.7% with five years of follow-up.
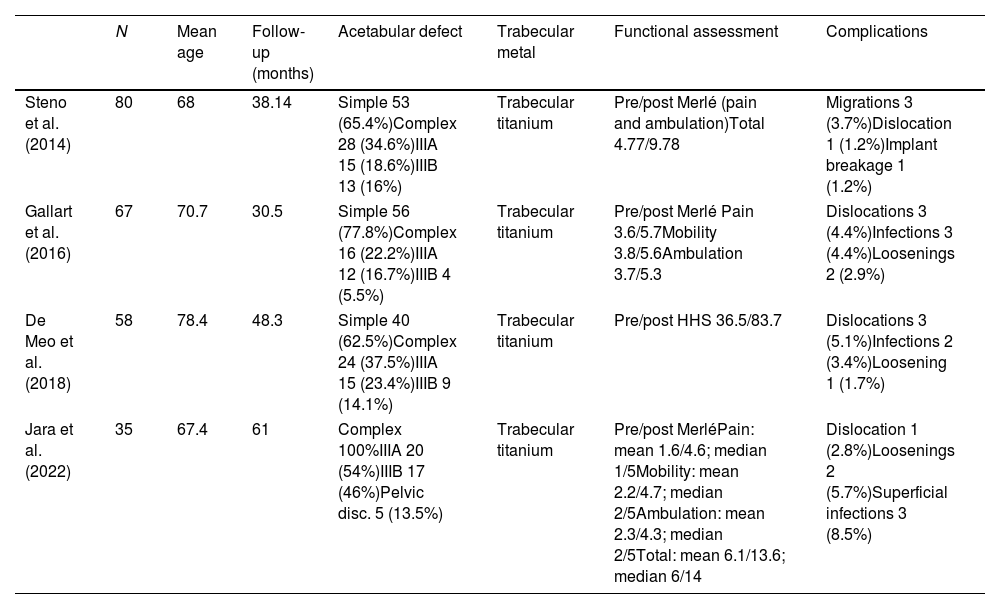
We recorded a complication rate of 17.1%, which included one case of dislocation, two cases of aseptic loosening, and three cases of superficial wound infection. These data are comparable to those found in the literature as shown in Table 4.
Comparative study table between our study and others published in the literature.
| N | Mean age | Follow-up (months) | Acetabular defect | Trabecular metal | Functional assessment | Complications | |
|---|---|---|---|---|---|---|---|
| Steno et al. (2014) | 80 | 68 | 38.14 | Simple 53 (65.4%)Complex 28 (34.6%)IIIA 15 (18.6%)IIIB 13 (16%) | Trabecular titanium | Pre/post Merlé (pain and ambulation)Total 4.77/9.78 | Migrations 3 (3.7%)Dislocation 1 (1.2%)Implant breakage 1 (1.2%) |
| Gallart et al. (2016) | 67 | 70.7 | 30.5 | Simple 56 (77.8%)Complex 16 (22.2%)IIIA 12 (16.7%)IIIB 4 (5.5%) | Trabecular titanium | Pre/post Merlé Pain 3.6/5.7Mobility 3.8/5.6Ambulation 3.7/5.3 | Dislocations 3 (4.4%)Infections 3 (4.4%)Loosenings 2 (2.9%) |
| De Meo et al. (2018) | 58 | 78.4 | 48.3 | Simple 40 (62.5%)Complex 24 (37.5%)IIIA 15 (23.4%)IIIB 9 (14.1%) | Trabecular titanium | Pre/post HHS 36.5/83.7 | Dislocations 3 (5.1%)Infections 2 (3.4%)Loosening 1 (1.7%) |
| Jara et al. (2022) | 35 | 67.4 | 61 | Complex 100%IIIA 20 (54%)IIIB 17 (46%)Pelvic disc. 5 (13.5%) | Trabecular titanium | Pre/post MerléPain: mean 1.6/4.6; median 1/5Mobility: mean 2.2/4.7; median 2/5Ambulation: mean 2.3/4.3; median 2/5Total: mean 6.1/13.6; median 6/14 | Dislocation 1 (2.8%)Loosenings 2 (5.7%)Superficial infections 3 (8.5%) |
Disc: pelvic discontinuity; HHS: Harris Hip Score; Merlé: modified Merlé D’Aubigné-Postel scale; N: hips included in the study after ruling out losses to follow-up due to causes unrelated to revision surgery; post: postoperative; pre: preoperative.
The most frequently reported complication in our study was aseptic loosening in 5.7% of cases. As mentioned above, this is mainly due to a deficit in bone stock which hinders both primary stability and subsequent osseointegration. This rate is slightly higher than that reported by other authors (Table 4), which may be because in our study only complex acetabular defects are studied, unlike those reported by other authors.
Therefore, we consider that because acetabular revision surgery in major bone defects is complex surgery and not free of complications, it should be performed by orthopaedic surgeons experienced in hip surgery and especially in the treatment of simple bone defects. As for the acetabular implant used in this series, we believe that its being a monobloc system improves the learning curve with respect to systems with independent cages and cups.
In terms of the limitations of our article, firstly, it is a retrospective descriptive study subject to the limitations inherent to this type of study. However, a comparative study between titanium and trabecular tantalum systems needs to be conducted, and between Cup-Cage implants and the other alternatives to reach more valuable conclusions. Furthermore, we believe that studies with longer follow-up periods are needed to corroborate the long-term usefulness of these implants. On the other hand, this is a series with few cases, as only patients with major acetabular defects are assessed. However, it should be noted that the present study is one of the series with the most cases of complex acetabular defects available in the literature.
ConclusionTo conclude, considering that revision surgery in major acetabular defects is technically very demanding, and analysing the data obtained and comparing them with those published by other authors, we believe that the use of Cup-Cage type trabecular titanium implants could be a valid option in acetabular revision surgery for complex acetabular defects due to their good primary fixation and osseointegration, with satisfactory clinical-radiological outcomes, and satisfactory results in terms of complications and implant survival in the medium term.
Level of evidenceLevel of evidence IV.
FundingThe authors declare that they received no funding to conduct this research study.
Conflict of interestsThe authors have no conflict of interest to declare.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics Committee ApprovalApproved by the Ethics Committee for Research with Medicines. Consorcio Hospital General de Valencia.





![(A) X-ray of a patient diagnosed with aseptic loosening of the left hip acetabular component with Paprosky type IIIA acetabular defect. (B) X-ray control three years after surgery to replace the acetabular component with a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]). TT: TRABECULAR titanium. (A) X-ray of a patient diagnosed with aseptic loosening of the left hip acetabular component with Paprosky type IIIA acetabular defect. (B) X-ray control three years after surgery to replace the acetabular component with a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]). TT: TRABECULAR titanium.](https://static.elsevier.es/multimedia/18884415/0000006700000002/v3_202404150803/S1888441522003605/v3_202404150803/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![(A) X-ray of a patient diagnosed with aseptic loosening of right hip acetabular component with Paprosky type IIIB acetabular defect associated with pelvic discontinuity. (B) Control X-ray at two years after revision of the cup to a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]). TT: trabecular titanium. (A) X-ray of a patient diagnosed with aseptic loosening of right hip acetabular component with Paprosky type IIIB acetabular defect associated with pelvic discontinuity. (B) Control X-ray at two years after revision of the cup to a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]). TT: trabecular titanium.](https://static.elsevier.es/multimedia/18884415/0000006700000002/v3_202404150803/S1888441522003605/v3_202404150803/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![(A and B) Intraoperative images of a patient with a Paprosky type IIIB acetabular defect associated with pelvic discontinuity for which cancellous allograft was used to fill the defect and a posterior spinal stabilisation plate (A) associated with a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]) (B). TT: trabecular titanium. (A and B) Intraoperative images of a patient with a Paprosky type IIIB acetabular defect associated with pelvic discontinuity for which cancellous allograft was used to fill the defect and a posterior spinal stabilisation plate (A) associated with a trabecular titanium Cup-Cage implant (Delta-Revision TT [Lima Corporate®]) (B). TT: trabecular titanium.](https://static.elsevier.es/multimedia/18884415/0000006700000002/v3_202404150803/S1888441522003605/v3_202404150803/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![(A) Control X-ray of a patient one month after placement of a trabecular titanium cup (Delta-Revision TT [Lima Corporate®]) showing early loosening of the implant. (B) Radiographic control at six months after replacement of this component with a new revision cup (Delta-Revision TT [Lima Corporate®]) modifying the acetabular orientation and combining increased trabecular titanium in the tectal region. TT: trabecular titanium. (A) Control X-ray of a patient one month after placement of a trabecular titanium cup (Delta-Revision TT [Lima Corporate®]) showing early loosening of the implant. (B) Radiographic control at six months after replacement of this component with a new revision cup (Delta-Revision TT [Lima Corporate®]) modifying the acetabular orientation and combining increased trabecular titanium in the tectal region. TT: trabecular titanium.](https://static.elsevier.es/multimedia/18884415/0000006700000002/v3_202404150803/S1888441522003605/v3_202404150803/en/main.assets/thumbnail/gr4.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)