Around 5–10% of deep vein thrombosis occurs in the upper limb. Its most frequent cause is usually cancer, central venous catheter, radio-chemotherapy or hormonal treatment. Less commonly, trauma around the shoulder region can also be a cause of deep vein thrombosis. Its diagnosis is probably more complex than in the lower limb due to its low frequency and clinical suspicion, as well as the clinical presentation, 50% of the cases being asymptomatic or presenting only with mild neck pain or omalgia.
Because of their infrequency, therapeutic recommendations are based on indirect evidence from studies of deep vein thrombosis of the lower limb, considering oral anticoagulation the best treatment.
We report a case of deep vein thrombosis in the upper limb after trauma to the shoulder causing grade III Rockwood acromioclavicular dislocation.
Un 5-10% de las trombosis venosas profundas ocurren en el miembro superior. Su causa más frecuente suele ser secundaria a cáncer, catéter venoso central, tratamiento con radio-quimioterapia u hormonal. Con menor frecuencia, los traumatismos en la región del hombro también pueden ser causantes de una trombosis venosa profunda. Su diagnóstico probablemente sea más complejo que en la extremidad inferior debido a su baja frecuencia, así como por la clínica que presenta, siendo un 50% de los casos asintomáticos o presentando tan solo una cervicalgia u omalgia leves.
Debido a su infrecuencia, las recomendaciones terapéuticas se basan en la evidencia indirecta de estudios de la trombosis venosa profunda de la extremidad inferior, siendo la anticoagulación oral el mejor tratamiento.
Presentamos un caso clínico de trombosis venosa profunda en miembro superior tras sufrir traumatismo directo en el hombro por una caída con bicicleta de montaña, causando una luxación acromioclavicular grado III de Rockwood.
Deep vein thrombosis is a relatively common complication that takes place following trauma and surgeries performed on the lower limbs, although they may also occur in the upper limbs. It has been estimated that between 5% and 10% of the cases appear at this level.1 More often than not, they are secondary to cancer, central venous catheter, treatment with radiochemotherapy, as well as hormone treatments, such as oral contraception or ovarian stimulation for in vitro fertilization. Its diagnosis is probably more complex, given to both its low frequency in traumatic and surgical pathology of the upper limb, as well as to its clinical manifestation. In 50% of the cases, the patient is asymptomatic or presents mild pain in the neck or shoulder that disguise diagnosis.2 The other half will exhibit the typical symptoms of oedema, pain, and the appearance of collateral venous circulation.3
We present a clinical case of deep vein thrombosis in the upper limb after suffering trauma in the shoulder, causing a Rockwood grade III acromioclavicular dislocation.
Clinical caseFifty-year old male who goes to emergency care for pain and deformity in his right shoulder after an accidental fall with direct trauma to said joint while mountain biking. He had no significant medical or surgical history; likewise, he had no known adverse drug effects.
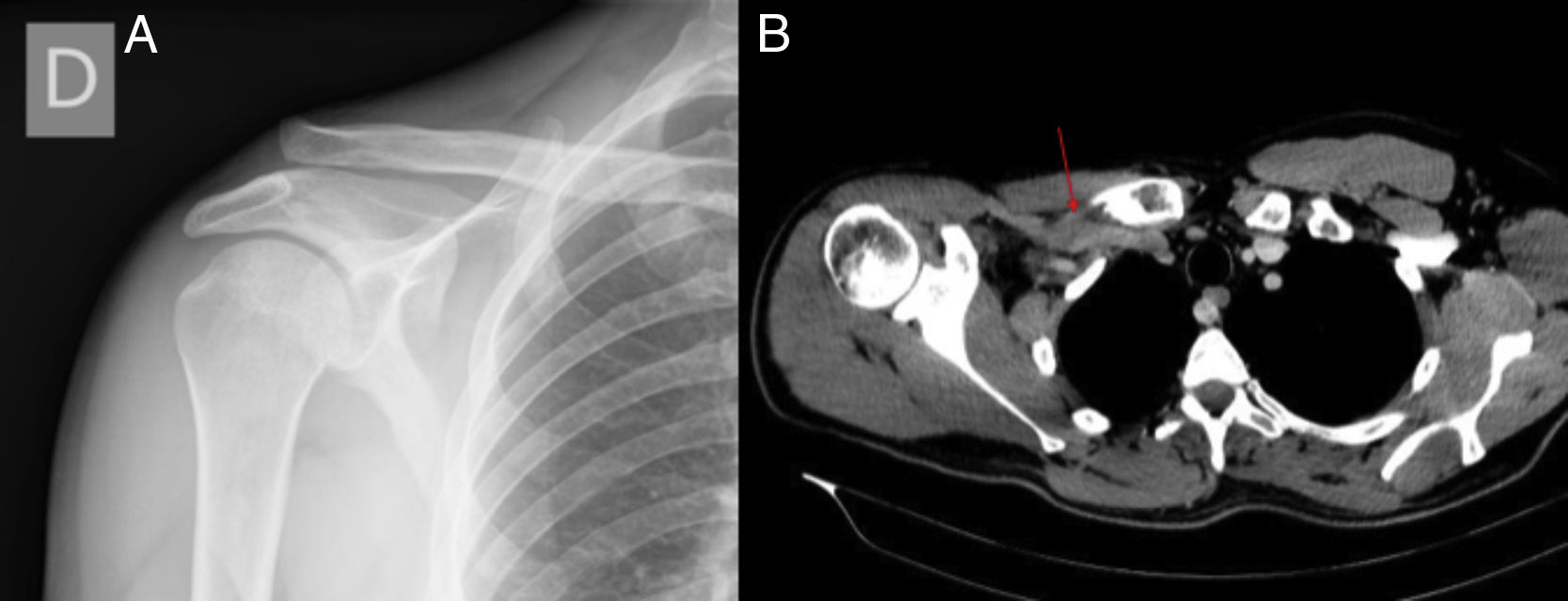
Physical examination revealed deformity and tenderness of the lateral third of his clavicle and right acromioclavicular joint, in addition to limited active joint mobility of the same shoulder due to pain. With the X-ray examination, a diagnosis was established of Rockwood grade III acromioclavicular dislocation (complete rupture of the acromioclavicular and coraco-clavicular ligament. Coraco-clavicular distance 25–100%) (Fig. 1). Surgical treatment for the dislocation was scheduled and the patient was discharged from the Emergency Service with a sling and analgesics, awaiting surgery.
(A) Radiological study of the right shoulder where a Rockwood grade III acromioclavicular dislocation (complete rupture of the acromioclavicular and coraco-clavicular ligament. Coraco-clavicular distance 25–100%) can be seen. (B) Computerized axial tomography with contrast in which the partial thrombosis of the subclavian vein suffered by the patient is indicated.
Seven days following the dislocation and coinciding with the day prior to the scheduled surgery, the patient returned to the Emergency Service for inflammation of the upper right limb of 4h of evolution.
On this occasion, the patient's entire right arm was swollen to twice the size of the contralateral arm. Likewise, he displayed generalized, painful tension oedema, painful and a cord-like hardening could be palpated all along the back of the arm. He did not exhibit any sensory or vascular alterations in said limb nor did the patient report any episode of fever in the last several days.
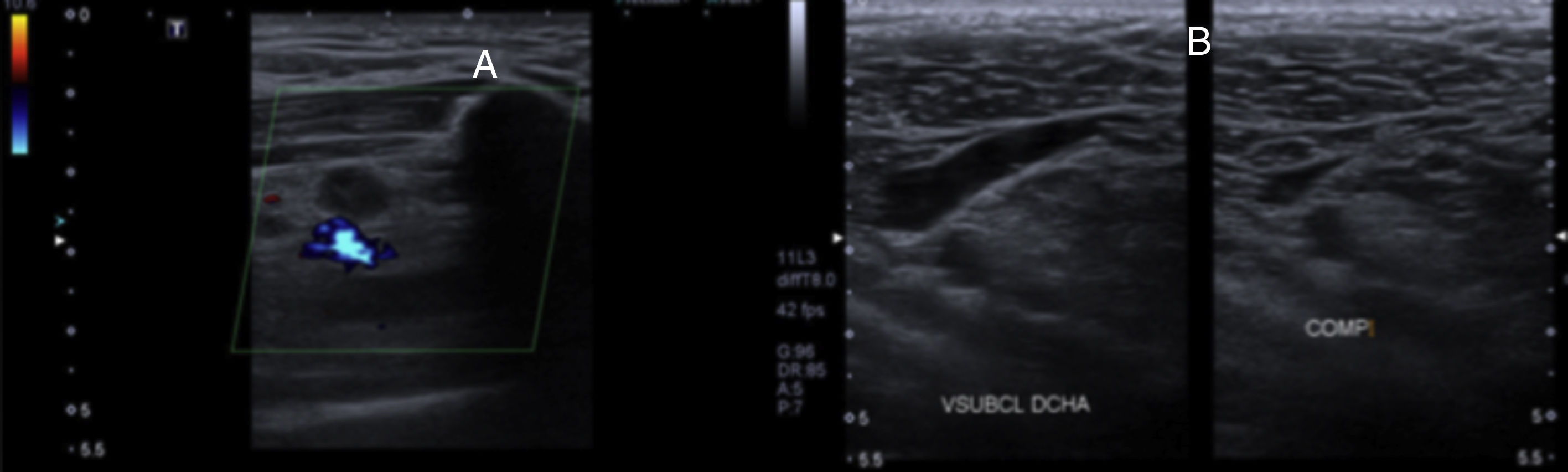
A complete blood workup was ordered (CBC, biochemistry, and coagulation) with dimer d, the result of which exceeded 13,000. In light of the suspicion of deep vein thrombosis, a Doppler ultrasound scan was performed that revealed hypoechogenic images in the subclavian vein (Fig. 2). With this result, a computerized axial tomography scan with contrast was ordered, which confirmed a partial thrombosis of the subclavian vein (Fig. 1).
(A) Doppler ultrasound in which hypoechogenic images can be seen in the subclavian vein, suspecting deep vein thrombosis. (B) Doppler ultrasound 6 months following the trauma and treatment with anticoagulation in which there is no imaging evidence of thrombosis and a permeable, elastic subclavian vein can be seen.
The patient was admitted and treatment with enoxaparin sodium was initiated at a therapeutic dose of 80mg every 12h, with the addition of oral anticoagulation with acenocumarol after 48h, as per the Hematology Service's recommended dosage. With this complication, the scheduled surgery was suspended and the decision was made to treat the dislocation by immobilizing the joint with a sling and analgesia. Seventy-two hours after admission, the oedema and pain in the arm had disappeared. The patient was therefore discharged with his haematological oral anticoagulation dosage.
ResultsThree weeks following the trauma, the patient's acromioclavicular joint was pain-free. The sling was removed and physical therapy was initiated. Three months later, the patient had recovered full mobility of the shoulder, without any pain or limitation.
Conversely, 6 months after the diagnosis of venous thrombosis of the subclavian vein, another Doppler ultrasound scan was performed. There was no imaging evidence of thrombosis, revealing the permeability and elasticity of right subclavian vein (Fig. 2). The oral anticoagulation was also suspended and the patient was discharged.
DiscussionThe vast majority of deep vein thromboses occur in the lower extremity. It is estimated that between 5% and 10% of the cases occur in the upper limb.1 Their diagnosis is complex and requires a high degree of clinical suspicion, since it causes various non-specific manifestations,2 the most common symptoms being inflammation, oedema, and a feeling of heaviness of the arm and shoulder. Furthermore, although less usual, it can cause pain, the appearance of collateral venous circulation, palpating the most prominent veins, discolouration of the arm, mottled skin, locally increased temperature, and may even be totally asymptomatic.3,4 As occurs in the lower extremity, these thromboses can become complicated with a symptomatic pulmonary embolism, a recurring deep vein thrombosis, or post-thrombotic syndrome of the arm.5 The more proximal the location of the thrombosis in the upper limb, the more common the appearance of complications.5 The most prevalent are the ones occurring at the level of the subclavian and axillary vein, followed by possible spread towards the innominate vein, the vein cava superior, or internal jugular vein.
Its aetiology is diverse and can be primary or secundary.6 Primary deep vein thrombosis [of the upper extremity], known as Paget-Schroetter syndrome, occurs as a result of strenuous exertion of the upper limb that causes endothelial damage in the vein that spontaneously provokes a venous thrombus.3 This can be idiopathic, spontaneous associated with thrombophilia or not, with effort, or traumatic provoked by a mechanism of retroversion and hyperabduction of the arm,4 causing dislocations and fractures in the area of the shoulder. It can also be due to other extrinsic compressions, such as cervical ribs, a hypertrophic callus in non-union of fractures of the clavicle, tumours, hypertrophy of the scalenes.4
Other causes are secondary to the placement of central venous lines, pacemakers, neoplasms, radio-chemotherapy treatment, oral contraception, hormone stimulation for in vitro fertilization, pregnancy, and other states of hypercoagulability.3
The formation of a thrombosis is multifactorial. Virchow7 established a triad of factors: the activation of blood coagulation (states of hypercoagulability), decrease in the rate of blood flow (venous stasis), and injury to the vascular wall (endothelial injury generally due to direct aggression or to manipulation of the limbs). It has been proven that at least two of these three pathogenic factors are needed for a venous thrombosis to develop. While they are uncommon, cases have been reported in the literature of thrombosis of upper limb in trauma that include injury to the shoulder, such as a fracture of the clavicle,8 anterior glenohumeral dislocation,9 fracture of the humerus,10 acromioclavicular dislocations,8 with greater risk entailed in grades III–VI.8 It etiopathogeny is likely to be due to endothelial injury, in addition to another factor contemplated in Virchow's triad, according to the characteristics of the patient.
In order to establish a diagnosis in individuals in whom there is a clinical suspicion of deep vein thrombosis of the upper limb, dimer d determination and a combined modality ultrasound scan (compression ultrasound or colour Doppler) are recommended.11 In those cases with a negative ultrasound or those that are difficult to assess, serial ultrasound scans or venography are recommended11 (conventional, by means of computerized tomography or magnetic resonance imaging). Given the low percentage of cases and, as a consequence, the lack of controlled clinical studies that have evaluated specific treatment for deep vein thrombosis of the upper limbs, most recommendations are based on indirect evidence derived from studies of deep vein thrombosis of the lower limbs. Therefore, in general, therapeutic management is not very different from that of treatment of deep vein thrombosis of the lower extremities.
It is worth adding, briefly, the good functional outcome of conservative treatment of Rockwood grade III acromioclavicular dislocations, as is the treatment chosen by most surgeons in recent years.12
Level of evidenceLevel of evidence IV.
FundingThere is not source of funding.
Conflict of interestsThere is not conflict of interests.
Please cite this article as: Osca Guadalajara M, Urgel Granados A, Royo Agustín M. Trombosis venosa profunda en extremidad superior como complicación tras luxación de la articulación acromioclavicular. Rev Esp Cir Ortop Traumatol. 2019;63:316–319.