The aim of the study was to evaluate the validity and safety of Ottawa's ankle rules (OAR) in the urgency department of referral hospital in Peru.
Materials and methodsAn observational-transversal study was conducted for a duration of 5 months (April–June 2016). Target population were all patients older than 18 years with a foot and ankle injury who came to the urgency department. A convenience non-randomised sampling was used. The OAR test was applied and X-rays of the foot and/or ankle were performed in all patients who met the inclusion and exclusion criteria. The data obtained was analysed using the SPSS 20.0 software. Sensitivity, specificity, positive predictive value, negative predictive value and likelihood ratio positive and negative were calculated from statistical analysis.
ResultsA total of 428 patients were evaluated. The OAR test's sensitivity was 97.2%, specificity was 30.3%, positive predictive value was 22.0%, negative predictive value was 98.2%, likelihood ratio positive and negative were 1.39 and 0.09, respectively. With the application of the OAR test, a reduction of 31.2% of the total X-rays was evidenced, which could generate a saving of US $1165.
ConclusionsIn conclusion, OAR's validity and safety in our environment are comparable to international data, with a reduction in the unnecessary use of radiographs. Multicentric studies involving a larger sample and longer study time are necessary to protocolize OAR in emergency units.
Evaluar la validez y seguridad de las reglas de Ottawa para medio pie y tobillo (ROmPT) en el servicio de urgencias de un hospital de referencia en Perú.
Materiales y métodosEl estudio fue observacional, transversal con duración de 5 meses (de febrero a junio de 2016). La población fueron los pacientes mayores de 18 años con un traumatismo de pie y/o tobillo que acudieron al servicio de urgencias. Se realizó un muestreo no aleatorizado por conveniencia. Se aplicaron las ROmPT y se realizaron rayos X de pie y/o tobillo a los pacientes que cumplieron los criterios de inclusión y exclusión. Los datos fueron tabulados y analizados con el programa SPSS v. 20.0. Se calcularon medidas de validez diagnóstica (sensibilidad, especificidad), seguridad diagnóstica (valor predictivo positivo, valor predictivo negativo) y likelihood ratio positiva y negativa.
ResultadosSe evaluaron 428 pacientes. El uso de las ROmPT obtuvo una sensibilidad del 97,2%, una especificidad del 30,3%, un valor predictivo positivo del 22,0%, un valor predictivo negativo del 98,2%, una likelihood ratio positiva de 1,39 y negativa de 0,09. Con la aplicación de las ROmPT, se evidenció una reducción del 31,2% del total de rayos X, que pudo generar un ahorro de 1.165$.
ConclusionesSe concluye que la validez y seguridad de las ROmPT en nuestro medio son comparables a las de estudios internacionales, con una posible reducción del uso de rayos X. Son necesarios estudios multicéntricos, con mayor tiempo de duración y cantidad de pacientes, para protocolizar el uso de este método en servicios de urgencias.
Problems related to foot and ankle trauma are frequent in patients attending hospital emergency departments; they account for approximately 5–12% of all injuries seen in the ED.1–7 Traumatic foot and ankle injuries generate significant morbidity in the population and absenteeism from work. For this reason, they are considered a neglected public health problem in Peru, according to WHO data.8 Soft tissue injuries of the foot and ankle are more frequent than fractures, with fractures accounting for approximately 15% (13–20%) of all foot and ankle injuries.3,5,6,9–14 It is common practice to order X-rays even when the physician is certain that there is no fracture. fractura.5 This situation generates deficiencies in care for both the patient and the health institutions,10 lengthening the waiting time in hospital emergency departments, increasing excessive exposure to radiation from X-rays15 and delaying timely treatment of the foot and ankle condition consulted.16
In 1992, Stiell, a professor at the University of Ottawa and the Minister of Health of Ontario (Canada), developed a clinical prediction rule called the Ottawa Rule for Midfoot and Ankle (OAR). This rule assesses pain on palpation in specific areas of the ankle and midfoot, together with the ability to tolerate load on the ankle and midfoot; its purpose is to determine whether or not X-rays are needed.3,17 The application of OARs yielded results in diagnostic validity testing, with sensitivity values of 100% and specificity of 25%; additionally, it yielded results in diagnostic safety testing, with a positive predictive value (PPV) of 18% and a negative predictive value (NPV) of 100%.3 An analysis of several studies combined showed a sensitivity of 98.5% (confidence interval [CI] 95: 97.2–99.8), a specificity of 31.1% (95% CI: 29.2–33.0, a PPV of 16.9% (95% CI: 15.2–18.6) and an PNV of 99.3% (95% CI: 98.7–99.9).18–20 The use of the OAR significantly reduced the number of X-rays performed in the ED by approximately 30%.11,14,17,20,21 (28% reduction for ankle and 14% for foot)4; it additionally reduced patient waiting time in the ED22, confirming its cost-effectiveness as a tool. According to Stiell's study,3 ankle X-rays are indicated if there is pain on palpation at any malleolus (lateral or medial) at the level of its inferior or posterior aspect, up to 6cm above the lowest point of the malleolus or if the patient is unable to tolerate weight bearing at the accident site and in the emergency department.23 X-rays of the foot would be indicated if there is pain on palpation at the level of the navicular or pain at the base of the fifth metatarsal or if the patient is unable to tolerate weight bearing at the site of the accident and in the emergency department. The use of OARs is not recommended in children under 18 years of age or in patients with injuries of more than 7–10 days of evolution.3,4,24
Physicians frequently express concern regarding medico-legal liability and its association with undetected fractures, due to the possibility of legal action by the patient.5,25 The medico-legal literature recommends the development of appropriately designed and validated clinical practice guidelines by hospital emergency departments for use as a support or defence against legal claims.19,26 The use of OARs is recommended by The Royal College of Radiologists due to their proven usefulness.15
The study sought to evaluate the validity and safety of the OAR in the population attending the emergency department of the Edgardo Rebagliati Martins National Hospital (HNERM) in Peru, during the period from February to June 2016, and to observe how the application of these clinical prediction rules influences the rational use of radiographs and the economic impact it could have.
Materials and methodsThe study was observational and cross-sectional, as the data were collected at a single point in time. The study was conducted over a period of 5 months (February–June 2016). The target population was patients over 18 years of age who presented with foot or ankle trauma, who attended the trauma emergency department of the HNERM to rule out a fracture by means of X-rays of the foot and/or ankle. The unit of analysis consisted of all those patients in the target population who met the inclusion and exclusion criteria. A non-randomised convenience sample drawn from the unit of analysis was used to select the study sample.
Inclusion criteria were:
- •
Any patient over 18 years of age with foot and/or ankle pain regardless of the mechanism of injury.
- •
Time of evolution of the injury<10 days.
- •
Patients attending the trauma emergency department of the HNERM during the period covered by the study.
Exclusion criteria were:
- •
Patients under 18 years of age.
- •
Pregnant women.27
- •
Patients attending the emergency department with previous X-rays taken in another hospital.
- •
Patients previously evaluated, who return.
- •
Patients with evident deformity that impresses dislocation and/or bone exposure at the level of the foot and ankle.
- •
Patients with known previous chronic disease of the foot or ankle related to previous trauma (e.g., osteosynthesis, osteomyelitis, rheumatoid arthritis, Charcot foot).
- •
Patients with diabetes mellitus of more than 5 years of evolution or with diabetic foot.
- •
Polytrauma patients.
- •
Skin lesion located on bony prominences to be evaluated according to the OAR.
- •
Altered state of consciousness due to trauma (Glasgow coma scale<14)28 or dementia.
Data were collected by means of a data collection form. The study variables, which included the OARs based on Stiell's original study1 were recorded. The variables were: inability to tolerate load (both at the scene of the accident and on arrival at the emergency room), which was defined as the inability to transfer weight twice on each lower limb (this does not include ambulation with a limp),23 and the variable pain location, which was defined as pain on palpation in the lateral and/or medial malleolus at the level of its inferior or posterior aspect, up to 6cm above its lowest point, or pain on palpation at the level of the navicular and/or base of the fifth metatarsal. Additionally, variables such as sex, age, mechanism of injury (twisting, direct blow, fall from height and traffic accident), time of the accident, time of taking the X-rays and time of discharge from the emergency room were collected. Ankle (anteroposterior and lateral) and/or foot (anteroposterior and oblique) X-rays were taken for all patients included in the study who met the inclusion-exclusion criteria, which could be ankle X-rays, foot X-rays or both. The X-rays were subsequently analysed by the attending physician and the resident physician on duty in the trauma ward, using the Kanteron® PACS-RIS system, which is installed in the emergency department; the operational concept of “significant fracture” was used, which was defined as a bone fragment greater than 3mm in diameter, a displacement greater than 2mm or a fracture trace of 3mm in length. Longitude.3,5,22,28 Each patient was treated according to clinical findings and X-ray findings.
Data collection was performed by third-year orthopaedic surgery and traumatology residents, who were previously trained in the physical examination of the patient and the application of the OAR. The physical examination, the application of the OAR and the recording of data were performed prior to the X-ray examination.
The data from the collection cards were transferred to a data tabulation matrix. SPSS® v. 20.0 was used for data analysis, with which frequencies of patient characteristics and relationships between variables were found. A 2×2 matrix was used to calculate measures of diagnostic validity, such as sensitivity and specificity, and diagnostic safety, such as PPV and NPV; measures such as positive (LR+) and negative (LR−) likelihood ratios were also evaluated. Descriptive frequency statistics were also obtained (sex, age, mechanism of injury, type of fracture, waiting time in the ED and delay in arrival at the ED).
The information obtained was kept confidential. The taking of radiographs of all patients and the consequent radiation exposure of the study subjects was not an ethical problem because it is now a procedure that is routinely requested from patients; the latter determines that the signing of an informed consent form is not necessary.2,21,28,29 The HNERM Ethics Committee approved the study (Approval letter No. 832-2015-1186) and recommended that the patient be informed verbally of the study objectives and that his or her verbal agreement to participate in the study be required.
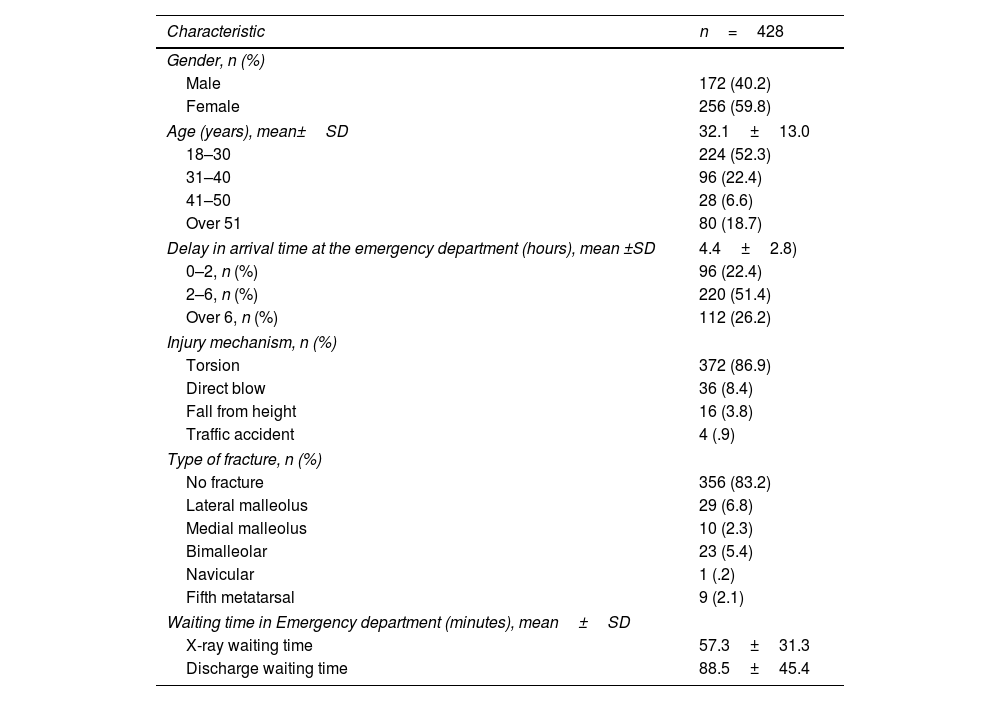
ResultsDuring the study period, 428 patients with foot or ankle trauma who were admitted to the emergency department of the HNERM and who met the inclusion and exclusion criteria were included. The female gender was predominant (59.8%). The mean age and standard deviation were 32.1±13.0 years. The predominant age group was 18–30 years (52.3%). The average time of arrival at the ED from the accident site was 4.4±2.8h, with the most frequent time of arrival at the ED being between 2 and 6h (51.4%). The most frequent mechanism of injury was twisting (86.9%). There were 72 fractures (16.8%) in the population studied, the most frequent being lateral malleolus (6.8%) and bimalleolar fractures (5.4%). Additionally, 9 fractures of the base of the fifth metatarsal (2.1%) and one of the navicular or tarsal scaphoid were found; the latter was later complemented with tomographic studies. It was found that the average waiting time in the ED for X-rays (time from arrival at the ED to X-ray) was 57.3±31.3min; additionally, it was found that the average waiting time in the ED for discharge was 88.5±45.4min (Table 1).
Clinical characteristics of the patients.
| Characteristic | n=428 |
|---|---|
| Gender, n (%) | |
| Male | 172 (40.2) |
| Female | 256 (59.8) |
| Age (years), mean±SD | 32.1±13.0 |
| 18–30 | 224 (52.3) |
| 31–40 | 96 (22.4) |
| 41–50 | 28 (6.6) |
| Over 51 | 80 (18.7) |
| Delay in arrival time at the emergency department (hours), mean ±SD | 4.4±2.8) |
| 0–2, n (%) | 96 (22.4) |
| 2–6, n (%) | 220 (51.4) |
| Over 6, n (%) | 112 (26.2) |
| Injury mechanism, n (%) | |
| Torsion | 372 (86.9) |
| Direct blow | 36 (8.4) |
| Fall from height | 16 (3.8) |
| Traffic accident | 4 (.9) |
| Type of fracture, n (%) | |
| No fracture | 356 (83.2) |
| Lateral malleolus | 29 (6.8) |
| Medial malleolus | 10 (2.3) |
| Bimalleolar | 23 (5.4) |
| Navicular | 1 (.2) |
| Fifth metatarsal | 9 (2.1) |
| Waiting time in Emergency department (minutes), mean±SD | |
| X-ray waiting time | 57.3±31.3 |
| Discharge waiting time | 88.5±45.4 |
SD: standard deviation.
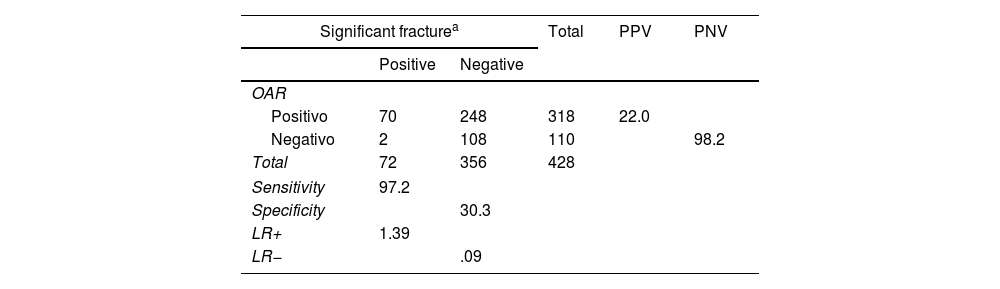
The sensitivity found in the study was 97.2% and specificity 30.3%; the PPV was 22.0% and NPV 98.2%. Additionally, the LR+=1.39 and LR−=.09 were calculated (Table 2).
Contingency table of validity and safety testing of OARs.
| Significant fracturea | Total | PPV | PNV | ||
|---|---|---|---|---|---|
| Positive | Negative | ||||
| OAR | |||||
| Positivo | 70 | 248 | 318 | 22.0 | |
| Negativo | 2 | 108 | 110 | 98.2 | |
| Total | 72 | 356 | 428 | ||
| Sensitivity | 97.2 | ||||
| Specificity | 30.3 | ||||
| LR+ | 1.39 | ||||
| LR− | .09 | ||||
LR: Likelihood ratio; OAR: Ottawa measurement rules; PNV: Predictive Negative Value; PPV: Predictive Positive Value.
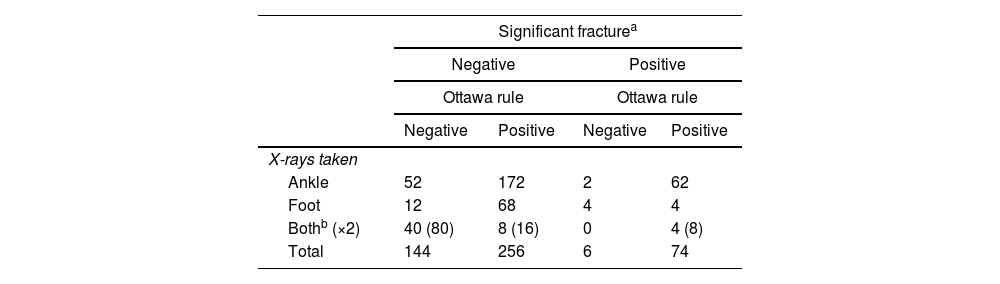
In the emergency department 480 X-rays were taken between ankle and foot, taking into consideration that the item of “both” X-rays counts for 2 as it includes X-rays of foot and ankle, adding for both equally (Table 3). If the OAR are negative, a decrease in the number of X-rays to be taken by 31.2% (150 X-rays) is evident; the latter is deduced by the formula [(X-rays taken in negative OAR)/total X-rays taken×100%]. Separately, the reduction in ankle X-rays was 27.6% and foot X-rays 40%. It is important to highlight that in Peru the average cost of X-rays in state entities is around $7, which could generate a total saving of $1165 in our study.
X-rays taken and the presence of significant fracture and OAR.
| Significant fracturea | ||||
|---|---|---|---|---|
| Negative | Positive | |||
| Ottawa rule | Ottawa rule | |||
| Negative | Positive | Negative | Positive | |
| X-rays taken | ||||
| Ankle | 52 | 172 | 2 | 62 |
| Foot | 12 | 68 | 4 | 4 |
| Bothb (×2) | 40 (80) | 8 (16) | 0 | 4 (8) |
| Total | 144 | 256 | 6 | 74 |
OAR: Ottawa ankle rules for measuring foot and ankle.
Studies since 1981 have focused their efforts on developing a clinical prediction rule for the use of X-rays in foot and ankle trauma.29 The OAR was validated by Stiell in 1991 in Canada. This clinical prediction rule was used in several countries, and results were found to be concordant with each other. Our study worked with a n=428, being a relatively small sample compared to Stiell's studies of 1992.1
Univariate analysis of the data obtained shows a predominance of the female group (59.8%) in foot and ankle injuries, possibly related to the type of high footwear frequently used in this population group. The age group aged 18–30 years showed a higher frequency of foot and ankle injuries in our study (52.3%), which may be due to the practice of risky activities such as high-competition sports. The most frequent mechanism of injury was twisting (86.9%), also closely related to the type of footwear and the sport practised. The total number of fractures found was 72 (16.8%); isolated malleolus fibula fractures (6.8%) and bimalleolar fractures (5.4%) were the most frequent significant fractures; one navicular fracture (0.2%) was also found. Navicular fractures are very difficult to diagnose using radiographs and clinically their mechanism of injury is not typical; this prevented the sensitivity of OAR from being even higher.
In his 1992 study Stiell1 reported that the application of OARs allowed him to achieve a diagnostic validity test result with a sensitivity of 100%, a specificity of 25%, a diagnostic confidence with a PPV of 18% and an NPV of 100%.3 The results of our study are comparable to those of Stiell, with a sensitivity of 97.2%, a specificity of 30.3%, a PPV of 22.0% and an NPV of 98.2%, which could affirm the reproducibility of OAR.
Waiting time for X-rays in our study was on average close to one hour (57.3min), while the range of time the patient spends in the emergency department (from admission to discharge) is on average up to one and a half hours (88.5min). It was observed that less time is spent on patient care compared to taking an X-ray which may be, in some cases, unnecessary. These measures have not been evaluated in previous studies.
In 2003 Bachmann et al., who in their meta-analysis of 27 studies combined, concluded that the application of OARs achieves diagnostic validity figures with a sensitivity of almost 100% and a possible reduction in the number of X-rays of 30–40%.20 The number of radiographs that could have been reduced in our study was 31.2% (the reduction for the ankle was 27.6% and for the foot 40%), given that the Ottawa rule was negative.
Broomhead and Stuart in 2003 described in their study that the OAR has been applied and used satisfactorily in populations such as the USA, France and Holland, but that in Scotland, New Zealand and Singapore they obtained unsatisfactory results attributed to a high false negative rate with a value of approximately 14%.28 In our study the false negative rate was 2.8%, with an LR+ of 1.39, which shows that it is not a good test for the diagnosis of fractures, but an LR− of 0.09, which makes it an excellent test for ruling out fractures or as a screening test according to Bayes’ theorem,30 The latter makes us think that it could be used satisfactorily in our environment.
Parrón Cambero et al. in 2006 evaluated the OAR in a Spanish population with 539 patients, finding diagnostic validity figures such as a sensitivity of 96.6%, a specificity of 34.7%, a PPV of 22.6% and a possible decrease in the number of X-rays of 27.8%31. Our study obtained similar diagnostic validity and safety figures in a different population and found a possible decrease of 31.2% in the number of X-ray tests if the OAR were applied, adding the LR values as a novelty. In our study, we found a possible saving of $,1165 different to that found in the study by Parrón Cambero et al. who found a possible saving of €2496.31 This is due to the economic differences between the two populations.
The main limitation of our study was the sample size (n=428), which is smaller compared to Stiell's original study (n=1660)1; however, it shows similar results in terms of validity and safety, which speaks to the reproducibility of the OAR. Another limitation was the amount of time used for the development of the study (5 months) compared to the original study by Stiell, who used 12 months for the development of his study divided into 2 phases. It is important to mention as a limitation the type of sampling used (non-randomised by convenience). However, the original study used a similar sampling methodology.
In conclusion, the validity and diagnostic safety of OAR are similar to the figures expressed in the international literature and, in our context, it is a reliable procedure, with a low percentage of complications. It represents a good screening tool for fracture screening in patients with foot and ankle trauma, which can be protocolised and applied in the trauma emergency department of our hospital. This clinical prediction rule (OAR) could have an impact on the rational use of X-rays and in economic terms, with a 31.2% reduction in the total number of X-rays, which translated into $1165 in our study. Further multicentre studies with a larger cohort and longer duration are recommended in order to conclude data applicable to hospital centres, which would provide an impact on public health.
Level of evidenceLevel of evidence iii.
Conflict of interestsThe authors have no conflicts of interest to declare.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Our particular thanks to the Department of Orthopaedics and Traumatology and to the HNERM Adult Emergency Service for the facilitating the setting and Access to information.